Published online Jan 7, 2011. doi: 10.3748/wjg.v17.i1.98
Revised: July 13, 2010
Accepted: July 20, 2010
Published online: January 7, 2011
AIM: To compare diverse endoscopic interventions in the management of occluded uncovered self-expanding metal stents (SEMSs) that had been placed for palliative treatment of unresectable malignant biliary obstruction.
METHODS: A retrospective review was undertaken in 4 tertiary endoscopic centers to determine optimal management of different types of occluded SEMSs. The technical success of performed treatment in occluded SEMSs, the patency of the stent, the need for re-intervention and the financial costs of each treatment were analyzed.
RESULTS: Fifty four patients were included in the analysis; 21 received Hanaro, 19 Wallstent and 14 Flexus. For the relief of obstruction, a plastic stent was inserted in 24 patients, a second SEMS in 25 and mechanical cleaning was performed in 5 patients. The overall median second patency rates between second SEMSs and plastic stents did not differ (133 d for SEMSs vs 106 d for plastic stents; P = 0.856). Similarly, no difference was found between the overall survival of SEMS and plastic stent groups, and no procedure-related complications occurred. Incremental cost analysis showed that successive plastic stenting was a cost-saving strategy at least in Greece.
CONCLUSION: Insertion of uncovered SEMSs or plastic stents is a safe and effective treatment for occluded uncovered SEMSs; insertion of plastic stents appears to be the most cost-effective strategy.
- Citation: Katsinelos P, Beltsis A, Chatzimavroudis G, Paikos D, Paroutoglou G, Kapetanos D, Terzoudis S, Lazaraki G, Pilpilidis I, Fasoulas K, Atmatzidis S, Zavos C, Kountouras J. Endoscopic management of occluded biliary uncovered metal stents: A multicenter experience. World J Gastroenterol 2011; 17(1): 98-104
- URL: https://www.wjgnet.com/1007-9327/full/v17/i1/98.htm
- DOI: https://dx.doi.org/10.3748/wjg.v17.i1.98
The treatment of choice for patients with unresectable malignant biliary obstructions with survival time beyond 6 mo, is the insertion of self-expanding metal stents (SEMSs), either endoscopically or percutaneously[1-4]. The main advantages of SEMSs over plastic stents in the palliation of malignant biliary strictures are their longer patency, greater complication-free survival, and cost-effectiveness, despite the initial cost; stent patency is critical because it significantly affects patient survival[5-7]. However, despite their large lumen, SEMSs are prone to occlusion by tissue ingrowth or overgrowth and biliary sludge/debris[8,9], resulting in recurrent jaundice or cholangitis; unlike plastic stents, the major disadvantage of SEMSs is the difficulty with repositioning or extraction once deployed[10]. In contrast, plastic stents are less expensive and easier to remove or to change, although they have a shorter duration of patency and a higher risk of clogging and dislocation[11]. There are currently limited data comparing the efficacy of different treatment options and reporting on the follow-up of SEMS occlusion; only 3 studies[12-14] described the management of occluded Wallstents and one with different types of SEMSs[15]. As SEMSs with different characteristics are more frequently used worldwide, we anticipate that occluded SEMSs of different types will be more commonly encountered in current clinical practice. Since experience and consensus regarding the optimal management of occlusion of different types of SEMSs is lacking, such data would be useful in clinical decisions. In this respect, in countries (e.g. Greece) where endoscopic retrograde cholangiopancreatography (ERCP) costs are very low compared to those with SEMSs, initial endoscopic retrograde biliary drainage by a plastic stent appears to be less expensive.
We conducted this study to compare diverse endoscopic interventions, but with significant cost difference, in the management of different types of occluded SEMSs by 4 tertiary level centers over a 10-year period.
A retrospective study was performed between September 1999 and December 2008 in 4 tertiary endoscopic centers in Northern (n = 3) and Central (n = 1) Greece, in patients undergoing therapeutic ERCP for unresectable malignant distal biliary obstruction. Medical records were reviewed to determine the management and clinical course until death of patients with occluded SEMSs or the end of the study period (cut-off date, January 31, 2009). Additional information was also obtained by phone contact with the patients’ referring physicians or relatives. The study was approved by the institutional review boards of all participating hospitals.
We identified patients through the endoscopy database. Age, sex, indication for first SEMS placement, information from outpatient visits, diagnostic tests, interventions and treatments that patients underwent at the 4 centers were reviewed. Three types of uncovered SEMS had been used. The Wallstent (Boston Scientific, USA) original SEMS is considered the industry standard. It consists of a braided stainless steel mesh with soft barbed ends, is available in 40, 60 and 80 mm lengths, and 8 or 10 mm diameter, and costs 2200 Euros. The Flexus (formerly Mometherm and Luminex) (ConMed, USA) is a highly flexible nitinol stent with flared ends. The stent is made from a laser-cut single piece of nitinol, a nickel-titanium alloy that provides a high degree of flexibility, and the interstices of the lattice work are large enough to permit cannulation and, after dilatation, placement of another stent in “Y” configuration for palliation of hilar strictures and costs 1950 Euros. The Hanaro (MI Tech, Korea) is also made of nitinol and costs 1650 Euros. The interstices of the lattice are larger compared to those of a Wallstent and similar to those of the Flexus stent.
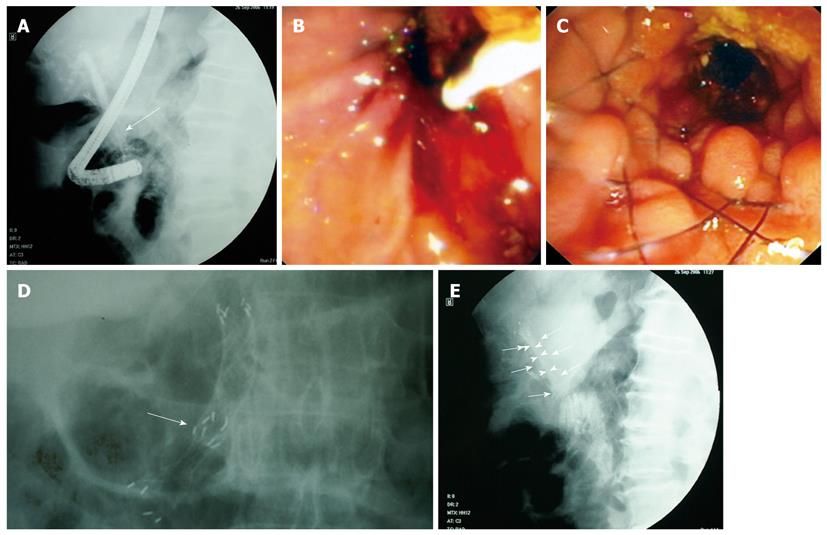
Stent occlusion was diagnosed when a patient developed symptoms and/or signs of cholangitis (fever, right upper quadrant tenderness, and/or a ≥ 2-fold increase in bilirubin concentration above baseline at the post endoscopic retrograde biliary drainage period) or when bilirubin concentration increased ≥ 2-fold above baseline after endoscopic retrograde biliary drainage, even without cholangitis symptoms and/or signs or an imaging study confirming biliary obstruction recurrence. The reason for stent occlusion was classified as predominantly tumor ingrowth, tumor proximal or distal overgrowth or obstruction from sludge/debris. Tumor ingrowth and proximal overgrowth were identified when cholangiography showed a stricture within the stent (Figure 1A) or a new stricture proximal to the stent, respectively. Distal overgrowth was diagnosed by direct endoscopic visualization (Figure 1B). Occlusion from debris or sludge was diagnosed when cholangiography showed filling defects within the lumen of the stent and cleaning of the stent produced passage of debris/sludge confirmed endoscopically. Management of occluded SEMSs included insertion of either an additional uncovered SEMS (Figure 1C and D) or a 10 Fr plastic stent (length 7, 9 or 10 cm) (Figure 1E) within the first or mechanical cleaning of the occluded SEMS. Mechanical cleaning was accomplished by flushing the obstructed SEMS with normal saline solution and repetitive passage of an inflated stone extraction balloon through the SEMS. Successful endoscopic management of stent occlusion was defined as a significant decrease in bilirubin level after the procedure and/or resolution of cholangitis or imaging improvement. First stent patency was defined as the time (in days) elapsed from the initial stent placement to the first occlusion that required one of the aforementioned interventions (placement of a second SEMS, plastic stent or mechanical cleaning). Second stent patency was defined as the time (in days) elapsed from the intervention to resolve the first occlusion to the first subsequent intervention or patient death with a patent stent. Overall second stent patency was defined as the time until a second SEMS became obstructed or the patient died with a patent SEMS, or, in the case of plastic stents, the time until no further stent exchanges could be performed or the patient died with a patent stent. For each treatment strategy to resolve the first SEMS obstruction (new SEMS, plastic stent or mechanical cleaning) we retrospectively counted the total amount of stents of either type used until the patient’s death and calculated the cost per patient.
The incremental cost per patient (excluding the cost of the initial SEMS) was calculated by multiplying the number of stents of each type used by their price adding the cost of a balloon catheter (160 Euros) for each mechanical cleaning procedure, 70 Euros for daily hospital charges and cost of hospitalization because of cholangitis until the endpoint, and 150 Euros for each ERCP, according to the financial policy of the Greek National Health System.
The analysis was performed using the statistical program Statistical Package for Social Sciences (SPSS, version 13.0, Chicago, IL, USA). The estimation of patient survival and stent patency in the various groups of the study was performed using the Kaplan-Meier method, supplemented by the log-rank test used for comparisons of groups in relation to their survival and the duration of patency of the stents.
For the purpose of statistical data analysis the χ2 test, Fisher’s exact test, the Mann-Whitney U test and the Kruskal-Wallis test were used. For comparisons between groups the Bonferroni adjusted P-value was used. Significance was set at P < 0.025.
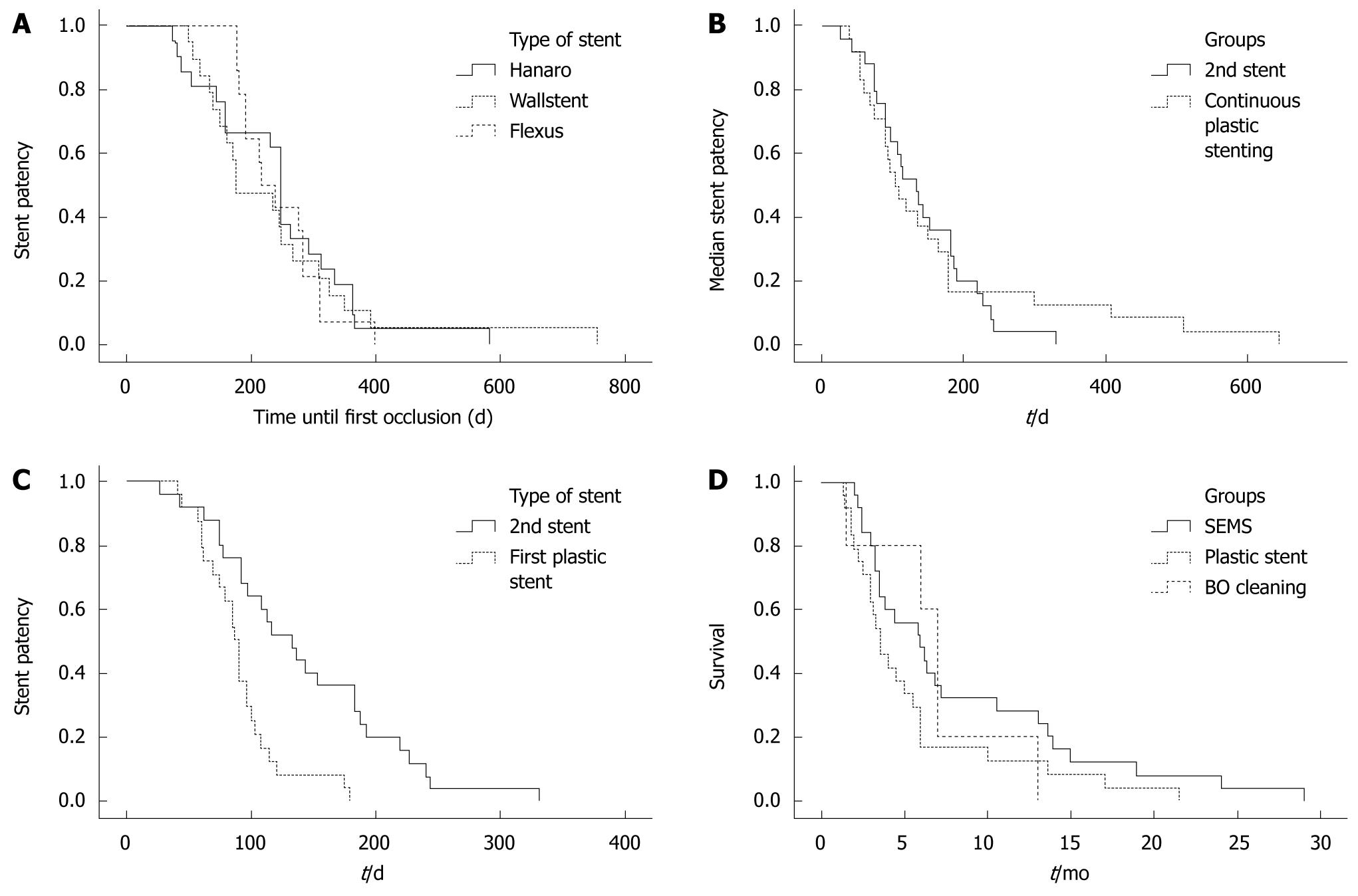
Between September 1999 and December 2008, 219 patients with distal unresectable biliary obstruction received uncovered SEMSs of 3 different types, at 4 tertiary endoscopy centers. Hanaro stents were used in 74, Wallstents in 81 and Flexus stents in 64 patients. Sixty-three (28.8%) patients who underwent an ERCP because of SEMS (Hanaro 26, Wallstent 20 and Flexus 17) occlusion as determined by an increasing serum bilirubin level and/or an imaging study confirming recurrence of biliary obstruction were identified. Nine patients were excluded from the study because data were incomplete for analysis. There were 54 patients, 31 male, 23 female; median age 71 (range, 54-86 years) who were followed up until death and were included in the analysis. Of the 54 uncovered SEMSs that were occluded, 21 were Hanaro, 19 Wallstent and 14 Flexus stents (Table 1). Indications for SEMSs insertion were: pancreatic carcinoma in 28, cholangiocarcinoma in 10, papillary cancer in 8, metastatic lymphadenopathy in 7 and hepatocellular carcinoma in 1 case (Table 1). Hepatic metastases were present in 6 patients with metastatic lymphadenopathy (Table 1). The cause of first SEMS occlusion was ingrowth in 35 patients (64.8%), overgrowth in 14 patients (25.9%) and sludge/debris in 5 patients (9.3%) (Table 1). There was no difference in the etiology of occlusion between the 3 types of SEMS (P = 0.773) (Table 1). The first occlusion presented as cholangitis in 31 (57.4%) and painless jaundice in 23 (42.6%) patients, without any significant difference between the 3 types of SEMS (P = 0.116) (Table 1). A plastic stent had been placed before SEMS insertion in 9 patients (Table 1). The overall median (range) duration of the first SEMS patency was 242.5 (74-754) d. More specifically, for Hanaro stents the patency period was 248 (74-582) d, for Wallstents 176 (98-754) d, and for Flexus stents 228.5 (178-398) d, with no significant difference between them (P = 0.936) (Table 1 and Figure 2A).
| Flexus | Hanaro | Wallstent | All stents | |
| No. of patients | 14 | 21 | 19 | 54 |
| Sex (M/F) | 5/9 | 9/12 | 9/10 | 23/31 |
| Median age (range) | 75 (59-86) | 69 (54-83) | 73 (60-83) | 71 (54-86) |
| Indication | ||||
| Pancreatic cancer | 7 | 12 | 9 | 28 |
| Biliary cancer | 3 | 3 | 4 | 10 |
| Hilar metastatic lymphadenopathy | 1 | 4 | 2 | 7 |
| Papillary tumor | 3 | 2 | 3 | 8 |
| Hepatocellular carcinoma | 1 | 1 | ||
| Hepatic metastases | 1 | 3 | 2 | 6 |
| Prior plastic stent | 5 | 2 | 2 | 9 |
| Presentation of first occlusion | ||||
| Painless jaundice | 3 | 12 | 8 | 23 |
| Cholangitis | 11 | 9 | 11 | 31 |
| Cause of obstruction | ||||
| Ingrowth | 7 | 16 | 12 | 35 |
| Overgrowth | 4 | 5 | 5 | 14 |
| Sludge and/or debris | 3 | 2 | 5 | |
| Median time to first occlusion (range) (d) | 228.5 (178-398) | 248 (74-582) | 176 (98-754) | 242.5 (7-754) |
| Type of intervention for first occlusion | ||||
| Self-expanding metal stent | 5 | 15 | 5 | 25 |
| Plastic stent | 6 | 6 | 12 | 24 |
| Mechanical cleaning | 3 | 2 | 5 |
The outcomes and financial costs of interventions in the course of treatment of first SEMS occlusion are summarized in Table 2. From the 25 patients managed by a second SEMS insertion, 17 (68%) died after a median 116 (62-227) d without requiring further intervention, but 8 (32%) patients presented with re-occluded stents after a median 144 (26-331) d (Table 2). Those with re-occluded stents were treated with either plastic stent insertion (5 patients) or mechanical cleaning (3 patients) and 9 plastic stents were required in total (Table 2). From the 24 patients managed by plastic stent insertion, 13 patients (54.2%) died after a median 84 (40-179) d without requiring further intervention but 11 (45.8%) patients presented with re-occluded stents after a median 91 (60-74) d and were treated with plastic stent exchanges as many times as required, resulting in the insertion of 20 additional plastic stents (Table 2). In 2 patients, both with papillary tumors, stent exchange was unsuccessful on the third and fourth ERCP due to duodenal invasion by the tumor. They refused further intervention and died. Of the 5 patients who were treated by mechanical cleaning alone, only one (20%) required no further interventions and died 39 d later, while the other 4 (80%) presented with a second obstruction after a median 112 (21-180) d, treated by plastic stent insertion in 3 patients and SEMS insertion in one (Table 2). Two patients required an additional plastic stent. Overall, 31 patients (57.4%) required no further interventions until their death after a median 97 (39-227) d and 23 patients (42.6%) presented with a second obstruction after a median 96 (21-331) d (Table 2).
| Plastic stent | Second SEMS | Mechanical cleaning | All types | P | |
| Intervention for first occlusion | |||||
| No. of patients | 24 | 25 | 5 | 54 | |
| Νo further interventions required | |||||
| No. of patients | 13 (54.2%) | 17 (68%) | 1 (20%) | 31 (57.4%) | |
| Survival after first occlusion without further interventions | 84 (40-179) | 116 (62-227) | 39 | 97 (39-227) | |
| Further intervention(s) required | |||||
| No. of patients | 11 (45.8%) | 8 (32%) | 4 (80%) | 23 (42.6%) | |
| Types of intervention | 11 plastic stents insertion | 5 plastic stents insertion | 3 plastic stents insertion | 19 plastic stents insertion | |
| 3 mechanical cleaning | 1 insertion of SEMS | 1 insertion of SEMS | |||
| 3 mechanical cleaning | |||||
| Time to second occlusion (d) | 91 (60-74) | 144 (26-331) | 112 (21-180) | 96 (21-331) | |
| Overall second stent patency | 106 (39-645) | 133 (26-331) | 0.856 | ||
| Second stent patency | 88 (40-179) | 133 (26-331) | < 0.001 | ||
| Survival after first occlusion | 106 (40-645) | 177 (60-870) | 210 (39-390) | 142 (39-870) | 0.180 |
| Number of interventions per patient | 1 (1-5) | 1 (1-4) | 2 (1-3) | 1 (1-5) | 0.199 |
| Cost per patient in euros | 590 (380-2550) | 2170 (1870-3620) | 1020 (380-2550) | 1685 (380-3620) | < 0.001 |
Apart from cholangitis, other complications including post-endoscopic retrograde biliary drainage bleeding, cholecystitis, pancreatitis or stent migration were not observed and there was no complication-related mortality.
Median overall patency of the second SEMS was 133 (range, 26-331) d and for successive plastic stenting 106 (range, 39-645) d (P = 0.856) (Figure 2B). However, when compared with the patency of the first plastic stent, which was 88 (range, 40-179) d, the patency of the second SEMS was significantly longer (P < 0.001) (Figure 2C). Survival after the first occlusion was 142 (range, 39-870) d: 106 (range, 40-645) d for plastic stent placement, 177 (range, 60-870) d for a second SEMS, and 210 (range, 39-870) d for mechanical cleaning (P = 0.180) (Figure 2D).
Overall, the average cost was 1685 (380-3620) Euros per patient: 2170 (1870-3620) Euros per patient for insertion of a second SEMS at initial obstruction, 590 (380-2550) Euros per patient for insertion of a plastic stent at the same setting and 1020 (380-2550) Euros per patient treated by mechanical cleaning (P < 0.001) (Table 2).
Although endoscopic biliary stenting is accepted as the treatment of choice in patients with inoperable malignant biliary obstruction, and has been associated with reduced morbidity and short hospital stay, the major problem faced after endoscopic stent insertion is stent occlusion. Relative data on the optimal management of occluded SEMSs, are very limited to case reports and small retrospective studies[12-15]. Our retrospective multicenter series includes the largest number of patients with occluded SEMSs managed endoscopically and is the second study to include different types of occluded SEMSs, thereby better depicting the daily practice worldwide. The initial occlusion rate of SEMSs in our series was 28.8%, consistent with that of previous studies[12,13]. Moreover, the occlusion rate was similar between the 3 types of SEMS (Hanaro 35.1%, Wallstent 24.7%, Flexus 26.6%), irrespective of the different design and material. The major cause of SEMSs occlusion was tumor ingrowth (64.8%), confirming the previous observations[12-15]. This is thought to have been secondary to the growth of tumors within the interstices of the uncovered SEMSs. It is interesting that the rate of ingrowth was similar among the 3 types of SEMS (Hanaro 76.2%, Wallstent 63.2%, Flexus 50%) despite the larger interstices of mesh in Hanaro and Flexus stents.
Our finding that mechanical cleaning of sludge/debris is an ineffective treatment for occluded SEMSs, presenting with high re-occlusion rates in a short time (median: 94 d, range: 21-180) is compatible with other series[12-14]. Notably, sludge is accrued because the stent surface allows for the adherence of proteins, glycoproteins, or bacteria and the bile flow is insufficient to clean the surface; stent clogging may be caused by microbiological adhesion and biliary stasis. In this regard, treatment with antibiotics and/or ursodeoxycholic acid to prevent clogging of biliary stents in patients with malignant stricture of the biliary tract, however, cannot be recommended routinely on the basis of the existing randomized clinical trials[16].
Placement of either a second SEMS, independent of its type, or a plastic stent inside the occluded SEMS, was equally effective in resolving the jaundice or the symptoms of cholangitis, in accordance with other series[12-15,17]. We found that the overall stent patency between second SEMSs and plastic stents for resolution of the first obstruction was not statistically different (133 d vs 106 d, P = 0.856) (Figure 2B). However, the patency of the second SEMS was significantly longer than that of the first plastic stent [133 (26-331) d vs 88 (40-179) d, P < 0.001] (Figure 2C), confirming the previous series. There was no difference on second SEMS patency between the 3 types of SEMS [Hanaro 144 (range, 42-331) d, Wallstent 97 (range, 26-243) days, Flexus 133 (range, 92-184) d] (P = 0.943). SEMS patency before the first occlusion was not predictive of the duration of the patency of the SEMS placed within the initial stent. This is in contrast to the observation of Katsinelos et al[11] of a positive correlation between the patency of the first Wallstent and the period of patency of the second Wallstent, but in accordance with Bueno et al[3] and Rogart et al[13] studies.
Kaplan-Meier analysis in our study revealed that survival of patients with a second SEMSs was similar to that with plastic stents (Figure 2D). Interestingly, patients who underwent a second SEMS placement had fewer subsequent interventions compared with patients who had plastic stents inserted, but the difference was not statistically significant (P = 0.33).
Several studies[3-10,12-15] have attempted to address the cost-effective management of occluded SEMS for malignant biliary obstruction. In our series, incremental cost analysis showed that the most cost-effective method appeared to be plastic stent insertion (P < 0.001) unlike the previous studies[3,12,13], but similar to the study by Abraham et al[1]. However, based on the special characteristics of our health system, our financial analysis is disproportionally influenced by the direct cost of stents, either SEMS or plastic, over the cost of ERCPs and the indirect cost of hospitalizations related to stent occlusion. Therefore, the cost-effectiveness data from our study may not apply directly to countries with different health systems.
Our study has limitations similar to those of prior studies, with retrospective analysis and a relatively small number of patients having a variety of causes for SEMS placement and expected survival. Because the subjects were not randomly allocated, firm conclusions cannot be drawn until a prospective randomized and stratified study in larger numbers confirms our findings. However, data from such a study are unlikely to be available in the near future.
In conclusion, our findings support the use of plastic stents as the main intervention in patients with occluded SEMSs despite the increased number of subsequent ERCPs, because it is cost-effective, especially in health systems where the cost of expendables markedly exceeds that of the medical services.
Self-expandable metal stents (SEMSs) remain the treatment of choice for patients with unresectable malignant biliary stricture and survival time beyond 6 mo. However, despite their large lumen, they are prone to occlusion. The reported experience on the management of occluded SEMSs of different types is limited.
Experience and consensus on the optimal management of occlusion of different types of SEMSs, which are used more frequently worldwide is lacking. However, such data are useful in clinical decisions about the treatment of occluded biliary uncovered SEMSs.
The present retrospective multicenter study investigated the diverse endoscopic interventions in the management of different types of occluded SEMSs. The findings support the use of a cost-effective plastic stent as the main intervention in patients with occluded uncovered SEMSs.
These findings are of potential financial importance especially in healthy systems where the cost of SEMSs markedly exceeds the medical service costs.
Uncovered SEMSs are occluded by tissue ingrowth or overgrowth and biliary sludge/debris, resulting in recurrent jaundice or cholangitis.
In this good retrospective study, the authors found that a cheap plastic biliary stent was as good as an expensive SEMS for the treatment of occluded SEMSs.
Peer reviewers: Ibrahim A Al Mofleh, Professor, Department of Medicine, College of Medicine, King Saud University, PO Box 2925, Riyadh 11461, Saudi Arabia; Yuk-Tong Lee, MD, Department of Medicine and Therapeutics, Prince of Wales Hospital, Shatin, New Territories, Hong Kong, China
S- Editor Tian L L- Editor Cant MR E- Editor Ma WH
| 1. | Abraham NS, Barkun JS, Barkun AN. Palliation of malignant biliary obstruction: a prospective trial examining impact on quality of life. Gastrointest Endosc. 2002;56:835-841. |
| 2. | Arguedas MR, Heudebert GH, Stinnett AA, Wilcox CM. Biliary stents in malignant obstructive jaundice due to pancreatic carcinoma: a cost-effectiveness analysis. Am J Gastroenterol. 2002;97:898-904. |
| 3. | Bueno JT, Gerdes H, Kurtz RC. Endoscopic management of occluded biliary Wallstents: a cancer center experience. Gastrointest Endosc. 2003;58:879-884. |
| 4. | Katsinelos P, Kountouras J, Paroutoglou G, Paikos D, Moschos J, Chatzimavroudis G, Zavos C, Makrigiannis E. Uncovered Hanaro Versus Luminex metal stents for palliation of malignant biliary strictures. J Clin Gastroenterol. 2008;42:539-545. |
| 5. | Davids PH, Groen AK, Rauws EA, Tytgat GN, Huibregtse K. Randomised trial of self-expanding metal stents versus polyethylene stents for distal malignant biliary obstruction. Lancet. 1992;340:1488-1492. |
| 6. | Hawes RH. Diagnostic and therapeutic uses of ERCP in pancreatic and biliary tract malignancies. Gastrointest Endosc. 2002;56:S201-S205. |
| 7. | Kaassis M, Boyer J, Dumas R, Ponchon T, Coumaros D, Delcenserie R, Canard JM, Fritsch J, Rey JF, Burtin P. Plastic or metal stents for malignant stricture of the common bile duct? Results of a randomized prospective study. Gastrointest Endosc. 2003;57:178-182. |
| 8. | Kim HS, Lee DK, Kim HG, Park JJ, Park SH, Kim JH, Yoo BM, Roe IH, Moon YS, Myung SJ. Features of malignant biliary obstruction affecting the patency of metallic stents: a multicenter study. Gastrointest Endosc. 2002;55:359-365. |
| 9. | Maire F, Hammel P, Ponsot P, Aubert A, O‘Toole D, Hentic O, Levy P, Ruszniewski P. Long-term outcome of biliary and duodenal stents in palliative treatment of patients with unresectable adenocarcinoma of the head of pancreas. Am J Gastroenterol. 2006;101:735-742. |
| 10. | Katsinelos P, Paikos D, Kountouras J, Chatzimavroudis G, Paroutoglou G, Moschos I, Gatopoulou A, Beltsis A, Zavos C, Papaziogas B. Tannenbaum and metal stents in the palliative treatment of malignant distal bile duct obstruction: a comparative study of patency and cost effectiveness. Surg Endosc. 2006;20:1587-1593. |
| 11. | Katsinelos P, Kountouras J, Paroutoglou G, Chatzimavroudis G, Paikos D, Zavos C, Karakousis K, Gelas G, Tzilves D. Migration of plastic biliary stents and endoscopic retrieval: an experience of three referral centers. Surg Laparosc Endosc Percutan Tech. 2009;19:217-221. |
| 12. | Menon K, Barkun A. Management of occluded biliary Wallstents. Gastrointest Endosc. 1999;49:403-405. |
| 13. | Rogart JN, Boghos A, Rossi F, Al-Hashem H, Siddiqui UD, Jamidar P, Aslanian H. Analysis of endoscopic management of occluded metal biliary stents at a single tertiary care center. Gastrointest Endosc. 2008;68:676-682. |
| 14. | Tham TC, Carr-Locke DL, Vandervoort J, Wong RC, Lichtenstein DR, Van Dam J, Ruymann F, Chow S, Bosco JJ, Qaseem T. Management of occluded biliary Wallstents. Gut. 1998;42:703-707. |
| 15. | Togawa O, Kawabe T, Isayama H, Nakai Y, Sasaki T, Arizumi T, Matsubara S, Ito Y, Yamamoto N, Sasahira N. Management of occluded uncovered metallic stents in patients with malignant distal biliary obstructions using covered metallic stents. J Clin Gastroenterol. 2008;42:546-549. |
| 16. | Galandi D, Schwarzer G, Bassler D, Allgaier HP. Ursodeoxycholic acid and/or antibiotics for prevention of biliary stent occlusion. Cochrane Database Syst Rev. 2002;CD003043. |
| 17. | Moss AC, Morris E, Mac Mathuna P. Palliative biliary stents for obstructing pancreatic carcinoma. Cochrane Database Syst Rev. 2006;CD004200. |