Published online Nov 14, 2010. doi: 10.3748/wjg.v16.i42.5388
Revised: August 25, 2010
Accepted: September 2, 2010
Published online: November 14, 2010
The rendezvous procedure combines an endoscopic technique with percutaneous transhepatic biliary drainage (PTBD). When a selective common bile duct cannulation fails, PTBD allows successful drainage and retrograde access for subsequent rendezvous techniques. Traditionally, rendezvous procedures such as the PTBD-assisted over-the-wire cannulation method, or the parallel cannulation technique, may be available when a bile duct cannot be selectively cannulated. When selective intrahepatic bile duct (IHD) cannulation fails, this modified rendezvous technique may be a feasible alternative. We report the case of a modified rendezvous technique, in which the guidewire was retrogradely passed into the IHD through the C2 catheter after end-to-end contact between the tips of the sphincterotome and the C2 catheter at the ampulla’s orifice, in a 39-year-old man who had been diagnosed with gallbladder carcinoma with a metastatic right IHD obstruction. Clinically this procedure may be a feasible and timesaving technique.
- Citation: Lee TH, Park SH, Lee SH, Lee CK, Lee SH, Chung IK, Kim HS, Kim SJ. Modified rendezvous intrahepatic bile duct cannulation technique to pass a PTBD catheter in ERCP. World J Gastroenterol 2010; 16(42): 5388-5390
- URL: https://www.wjgnet.com/1007-9327/full/v16/i42/5388.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i42.5388
Selective deep cannulation of the bile duct is essential for the successful treatment of biliary obstructions. However, even the most experienced endoscopists fail to cannulate the biliary tract in 5%-10% of cases[1-4]. When a selective biliary cannulation fails, percutaneous transhepatic biliary drainage (PTBD) allows successful drainage and retrograde access for subsequent rendezvous techniques. Traditionally, rendezvous procedures such as the PTBD-assisted over-the-wire cannulation method, the parallel cannulation technique, or others may be available when a bile duct cannot be selectively cannulated[5-9]. When a selective intrahepatic bile duct (IHD) cannulation fails, a rendezvous technique may be an alternative.
We describe a modified rendezvous technique in a case of right IHD obstruction caused by metastatic gallbladder malignancy. After end-to-end contact between the tips of the sphincterotome and the C2 catheter at the ampulla’s orifice, the guidewire was retrogradely passed into the IHD through the C2 catheter. Clinically this procedure is feasible and timesaving. To the best of our knowledge, this technique has not yet appeared in the English language literature.
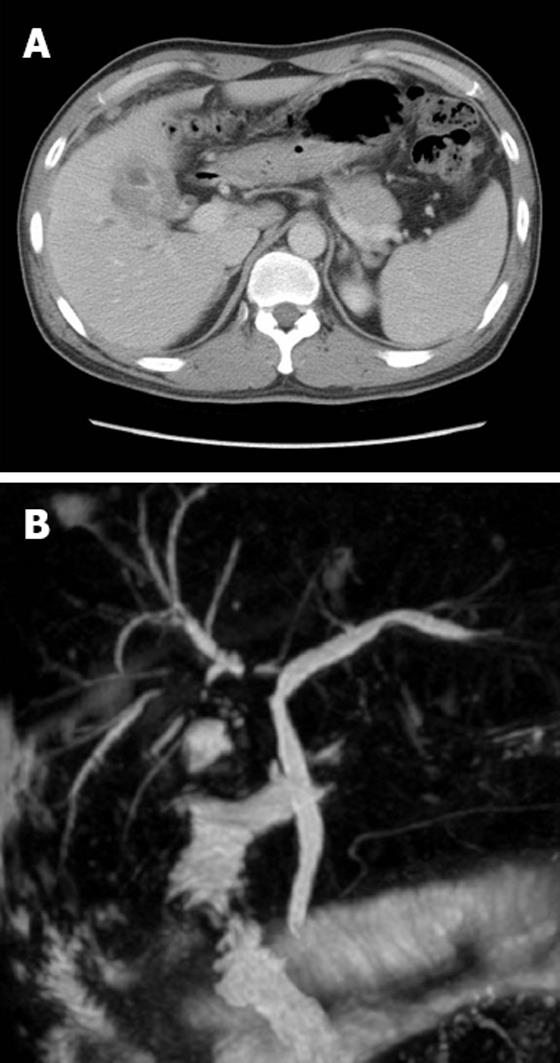
A 39-year-old man with no specific medical history presented with right upper quadrant abdominal pain and weight loss that had started to worsen a month before presentation. Laboratory tests revealed the following: total bilirubin, 28 mg/L (normal 2-12 mg/L); aspartate transaminase/alanine transaminase, 132/331 IU/L (normal 0-40 IU/L); alkaline phosphatase, 497 IU/L (normal 39-117 IU/L); γ-glutamyltransferase, 571 IU/L (normal 0-52 IU/L); and CA19-9, 56.3 U/mL (normal 0-34 U/mL). Abdominal computed tomography revealed diffuse low-attenuated wall thickening of the gallbladder with multiple metastatic nodules on the subhepatic and right-lower abdomen. Magnetic resonance cholangiopancreatography images showed severe segmental stricture of the right IHD with mild peripheral ductal dilatation (Figure 1).
Subsequent endoscopic retrograde cholangiopancreatography (ERCP) showed that the contrast did not pass through. Selective cannulation of the right IHD was impossible even using various sized guidewires and papillotomes such as Autotome (Boston Scientific, Microvasive, Marlboro, MA, USA) because of severe obstruction (Figure 2). Access to the strictured IHD was obtained by PTBD using a 5 F, 75 cm C2 catheter (Cook Endoscopy, Winston-Salem, NC, USA). After PTBD, a C2 catheter was placed into the duodenum through the stricture site and CBD (Figure 3). In the second ERCP, a rendezvous procedure was planned to selectively access the right IHD. A guidewire-preloaded sphincterotome was positioned onto the ampulla and the C2 catheter was then slowly pulled out near the ampulla’s orifice. After end-to-end contact between the tips of the sphincterotome and the C2 catheter at the ampulla’s orifice, the guidewire was passed into the IHD through the C2 catheter, while simultaneously, the sphincterotome was pushed and the C2 catheter was pulled out (Figures 3 and 4). The guidewire was then selectively placed into the IHD. Finally, following balloon dilatation (Hurricane balloon, 4 mm, 60 s; Boston Scientific, MA, USA), a 7 F Amsterdam stent (Cook Endoscopy) was successfully inserted into the IHD. However, endoscopic biopsy or cytology on the stricture site was not performed. A ultrasonography-guided biopsy of the metastatic mass in the right-lower abdomen diagnosed it as an adenocarcinoma (immunohistochemical stains; CK7+, CK20-, and CDX2-). The patient was placed on concurrent systemic chemotherapy and radiotherapy.
When a selective CBD cannulation cannot be performed at ERCP despite trying various endoscopic techniques, PTBD followed by a combined rendezvous technique is often successful[5-13]. This combined technique increases the success rate of biliary tract cannulation and facilitates the diagnosis and treatment of biliary tract diseases. Initially, a PTBD-placed guidewire is grasped at the tip of the duodenoscope; then the duodenoscope and wire are withdrawn[8]. This technique has some limitations, such as the two sessions required for the endoscopic procedure, difficulty grasping the wire with forceps, and kinking of the guidewire. Mönkemüller et al[9] recommend advancing the guidewire into the catheter’s tip so that it can guide cannulation of the ampulla, but this can be difficult and requires that the wire be passed carefully. Dickey suggested a parallel cannulation technique using a sphincterotome retrogradely, alongside a biliary drainage catheter[7]. This technique can be performed in one session if CBD cannulation is difficult.
However, even if selective CBD cannulation is successful, when a selective IHD cannulation fails, this modified rendezvous technique may be useful. In our case, the right IHD was almost totally obstructed due to direct invasion of a gallbladder carcinoma, which prevented selective IHD cannulation despite various attempts at cannulation. Moreover, even though PTBD was successful, a 5 F C2 catheter, rather than a 7-10 F catheter which is commonly used, was placed because of severe stricture and abdominal pain during the procedure. The modified rendezvous procedure described above was then performed successfully. In cases of tight bile duct obstruction without marked ductal dilatation, it is difficult to place a metal stent via a PTBD route. In addition, plastic stent insertion is not possible via PTBD. The size of the transhepatic track necessary to insert a plastic stent percutaneously is related to the high complication rates of percutaneous stenting[14]. Endoscopic retrograde access was also impossible because of the inserted PTBD catheter. In such cases, this rendezvous technique can be a viable alternative.
In conclusion, this modified rendezvous technique for selective IHD cannulation appears to be a safe and feasible procedure. This technique is useful in selected cases such as the one presented here and in cases of failed selective CBD cannulation.
Peer reviewer: Dr. Hyoung-Chul Oh, Assistant Professor, Department of Internal Medicine, Chung-Ang University, College of Medicine, #65-207 Hanganro-3ga Yongsan-gu, Seoul, 140757, South Korea
S- Editor Sun H L- Editor Webster JR E- Editor Lin YP
| 1. | Sherman S, Hawes RH, Lehman GA. Management of bile duct stones. Semin Liver Dis. 1990;10:205-221. |
| 2. | Vaira D, D'Anna L, Ainley C, Dowsett J, Williams S, Baillie J, Cairns S, Croker J, Salmon P, Cotton P. Endoscopic sphincterotomy in 1000 consecutive patients. Lancet. 1989;2:431-434. |
| 4. | Cotton PB. Endoscopic management of bile duct stones; (apples and oranges). Gut. 1984;25:587-597. |
| 5. | Freeman ML, Guda NM. ERCP cannulation: a review of reported techniques. Gastrointest Endosc. 2005;61:112-125. |
| 6. | Martin DF. Combined percutaneous and endoscopic procedures for bile duct obstruction. Gut. 1994;35:1011-1012. |
| 7. | Dickey W. Parallel cannulation technique at ERCP rendezvous. Gastrointest Endosc. 2006;63:686-687. |
| 8. | Calvo MM, Bujanda L, Heras I, Cabriada JL, Bernal A, Orive V, Miguelez J. The rendezvous technique for the treatment of choledocholithiasis. Gastrointest Endosc. 2001;54:511-513. |
| 9. | Mönkemüller KE, Linder JD, Fry LC. Modified rendezvous technique for biliary cannulation. Endoscopy. 2002;34:936. |
| 10. | Shorvon PJ, Cotton PB, Mason RR, Siegel JH, Hatfield AR. Percutaneous transhepatic assistance for duodenoscopic sphincterotomy. Gut. 1985;26:1373-1376. |
| 11. | Peterson BT. Biliary rendezvous or solo combined procedure for therapy of sump syndrome. Gastrointest Endosc. 1996;43:176-177. |
| 12. | Chang JH, Lee IS, Chun HJ, Choi JY, Yoon SK, Kim DG, You YK, Choi MG, Choi KY, Chung IS. Usefulness of the rendezvous technique for biliary stricture after adult right-lobe living-donor liver transplantation with duct-to-duct anastomosis. Gut Liver. 2010;4:68-75. |
| 13. | Qian XJ, Zhai RY, Dai DK, Yu P, Gao L. Treatment of malignant biliary obstruction by combined percutaneous transhepatic biliary drainage with local tumor treatment. World J Gastroenterol. 2006;12:331-5. |