Published online Jan 28, 2010. doi: 10.3748/wjg.v16.i4.526
Revised: November 12, 2009
Accepted: November 19, 2009
Published online: January 28, 2010
Conventional hepatectomy is an effective way to treat hepatocellular carcinoma. However, it is invasive and stressful. The use of laparoscopy in hepatectomy, while technically demanding, reduces surgical invasiveness and stressfulness but still achieves complete resection with adequate margins. Compared with conventional hepatectomy, laparoscopic hepatectomy provides a better chance and situation for further surgery in the case of recurrence of hepatocellular carcinoma. Even aged patients can successfully endure repeated hepatectomy using laparoscopy, as shown in the present report. This report presents a case of repeated laparoscopic hepatectomy treating hepatocellular carcinoma and its recurrence in an aged patient having cirrhosis, a disease causing extra difficulty for performing laparoscopic hepatectomy. The report also describes techniques of the operation and displays characteristic results of laparoscopic hepatectomy such as smaller wounds, less blood loss, less pain, less scars and adhesion, shorter postoperative hospital stay, and faster recovery.
- Citation: Cheung TT, Ng KKC, Poon RTP, Chan SC, Lo CM, Fan ST. A case of laparoscopic hepatectomy for recurrent hepatocellular carcinoma. World J Gastroenterol 2010; 16(4): 526-530
- URL: https://www.wjgnet.com/1007-9327/full/v16/i4/526.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i4.526
Laparoscopic surgery, a kind of minimally invasive surgery, has recently gained considerable advances. Nonetheless, laparoscopic hepatectomy still presents various kinds of difficulties to surgeons. Initial laparoscopic approaches in hepatic surgery were first limited to staging procedures, then extended to non-anatomical resection for hepatic lesions such as cyst, adenoma, hemangioma, and solitary liver metastasis[1-3]. Challenges of liver manipulation, parenchymal transection and hemostasis were hurdles in the progress of laparoscopic hepatectomy. Hazards such as gas embolism and difficulty in controlling bleeding discouraged many surgeons. However, with the accumulation of experience, laparoscopic hepatectomy, albeit technically demanding, is being employed to treat hepatocellular carcinoma (HCC), and reports on its safety, efficacy and reproducibility are emerging.
Like conventional hepatectomy, laparoscopic hepatectomy allows complete resection of tumors with adequate margins; but on top of this, it has a number of advantages over the former. It causes smaller wounds, less blood loss, less pain, less scars and adhesion, and smaller chance of incisional hernia. These advantages provide a better chance and situation for further surgery in the case of HCC recurrence which is common and hence anticipated[4]. Moreover, they render the operation less invasive and less stressful, and so make it a good treatment option for aged patients. Patients also need shorter postoperative hospital stay and have faster recovery. In the past, laparoscopic hepatectomy was not recommended for cirrhotic livers because of their high tendency towards bleeding during operation, but with improved magnification and illumination in laparoscopy today, the risk of bleeding has lessened and laparoscopic hepatectomy is no longer precluded by cirrhosis[5-7].
This report presents a case of repeated laparoscopic hepatectomy treating HCC and its recurrence in an aged cirrhotic patient and describes the surgical techniques therein.
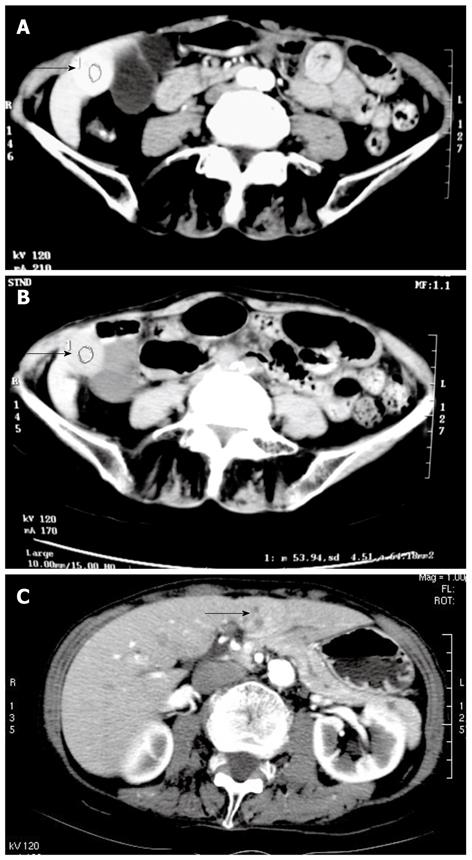
An 85-year-old woman who had left radical mastectomy performed 30 years ago for carcinoma of the left breast was referred to us because of deranged liver function associated with elevated serum alpha-fetoprotein level. An ultrasound study was carried out and revealed a 2.7-cm hypoechoic lesion at the inferior tip of the right hepatic lobe. She had a serum alpha-fetoprotein level of 80 ng/mL and γ-glutamyl transferase level of 226 U/L. Her platelet count was 132 × 109/L. She was negative for both hepatitis B virus and hepatitis C virus, and her liver function was classified as Child-Pugh class A. Her indocyanine green retention rate at 15 min was 12.7%. Computed tomography (CT) scan with contrast revealed a 2.5-cm hypervascular tumor with early washout of contrast in segment 5 of the liver (Figure 1A and B). The overall picture was indicative of HCC, and laparoscopic wedge resection was planned.
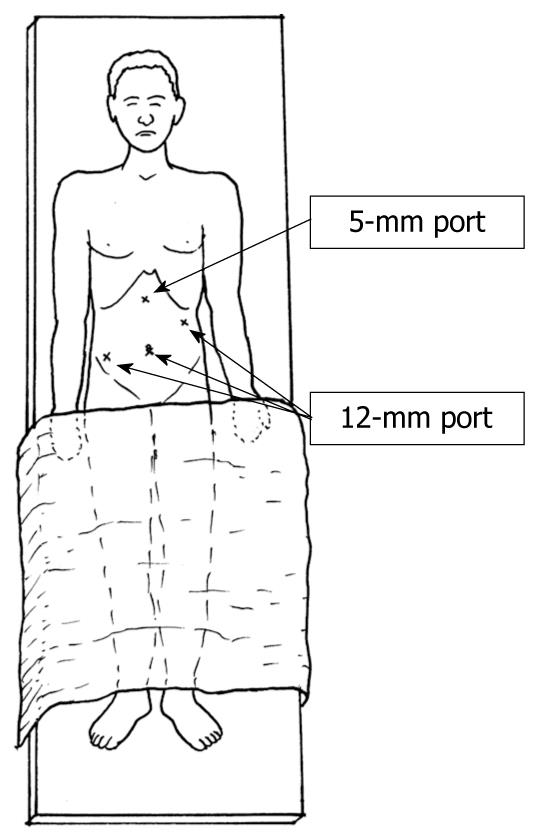
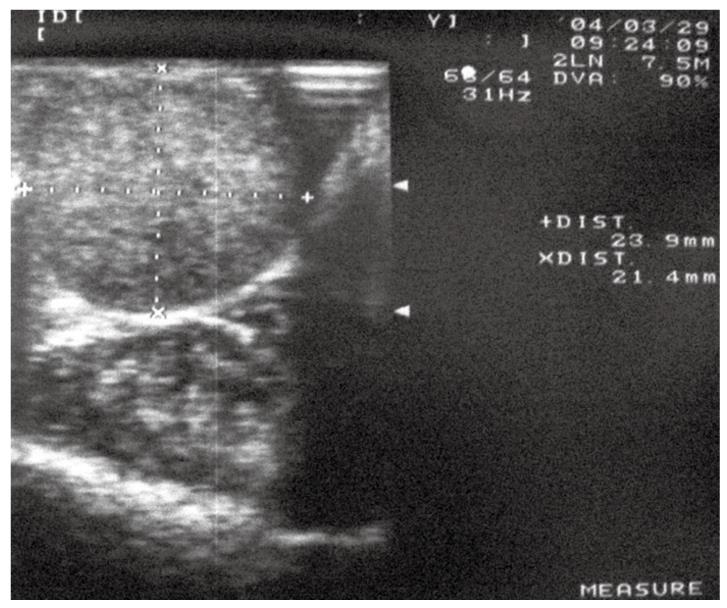
The operation was performed under general anesthesia. The patient was placed in a supine position with a 30-degree Trendelenburg adjustment. The surgeon and an assistant stood at the right side of the patient. A 12-mm port was created using the open method. Pneumoperitoneum was introduced by insufflation of CO2, and intra-abdominal pressure was maintained at 12 cmH2O. A second 12-mm port was created 2 cm below the left costal margin along the anterior axillary line. A third 12-mm port was made at the right iliac fossa. Three trocars were positioned along a semicircular line, with the concavity facing the right subcostal margin. Finally, a 5-mm port was made in the subxiphoid region (Figure 2). Standard diagnostic and staging laparoscopy was performed, and the liver was examined using laparoscopic ultrasound (Aloka, Tokyo, Japan) to confirm the extension of the tumor and its relationship to the vasculature (Figure 3). The area to be transected was marked by diathermy. Resection was performed with the no-touch technique, and the liver parenchyma was transected using electrocautery supplemented by 6 cycles of radiofrequency ablation using a 3-cm single cooled-tip electrode. Each cycle of radiofrequency ablation lasted for 2 min. Hemostasis was achieved using metallic clips and by argon beam coagulation. A 1-cm resection margin was achieved. The operation lasted 180 min. No complication occurred during the operation. Blood loss of 120 mL was recorded and no blood transfusion was needed. Pringle maneuver was not applied in the operation.
Feeding started on the second day of the operation. Liver function returned to preoperative level on the fifth day. The patient was discharged home on the sixth day.
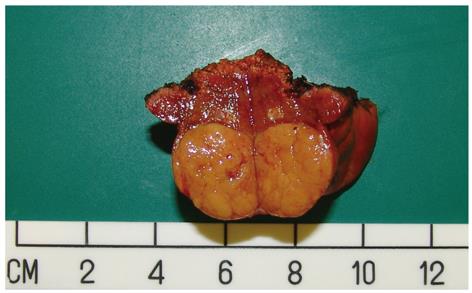
Pathology confirmed the presence of moderately differentiated HCC measuring 2.5 cm, 8 mm from the resection margin (Figure 4).
The patient was regularly followed up with CT scan and serum alpha-fetoprotein check every three months. Her serum alpha-fetoprotein level returned to 50 ng/mL three months after surgery and remained static in subsequent follow-ups, until the end of the first year when it rose to 3489 ng/mL.
CT scan with contrast was done and revealed an arterial enhancing mass measuring 3 cm × 1.8 cm × 3 cm in segment 2 and segment 3 of the liver, which suggested HCC (Figure 1C). Repeated laparoscopic hepatectomy was to be performed.
The patient was placed in the Lloyd-Davis position under general anesthesia. The surgeon stood between the legs with one assistant on each side. Ports were re-created at sites as in the previous operation, and pneumoperitoneum was performed. The ports measured between 5 mm and 12 mm, allowing easy change of instruments, offering flexibility in the use of ultrasonic dissector with both hands, and facilitating the introduction of endo-staplers. The falciform ligament was divided and laparoscopic ultrasound was applied to identify the vasculature of the liver. The left lateral segment was mobilized and parenchymal transection was performed with a Cavitron ultrasonic surgical aspirator (CUSA). The left lateral segment pedicle was divided using an endovascular stapler. The liver was delivered through a 6-cm left subcostal incision. The operation lasted 250 min. No adhesion was encountered and no complication occurred. Blood loss of 200 mL was recorded and no blood transfusion was needed. Pringle maneuver was not applied in the operation.
The patient was monitored in the intensive care unit for one day, and was transferred to the general surgical ward on the second day when feeding was resumed. Her liver function returned to preoperative level on the fifth day. She was discharged home on the ninth day.
Pathology confirmed the presence of moderately differentiated HCC measuring 7 cm, 7 mm from the resection margin.
The patient was faring well and remained disease-free at follow-up 18 mo later.
Different new techniques for hepatic resection have arisen, but they remain controversial. Amongst these new techniques, the minimally invasive approach using laparoscopy has been drawing much attention[8-11]. Since the introduction of laparoscopic cholecystectomy in 1987, the laparoscopic approach has been developed for different kinds of abdominal surgery, such as gastrointestinal treatment. As to hepatic treatment, initial laparoscopic procedures in hepatectomy were limited to biopsy, tumor staging, fenestration of liver cysts, and resection of benign liver tumors. Currently, there are a few reported series on laparoscopic resection of HCC in patients with cirrhosis[6,7,12-15]. Experience of laparoscopic hepatectomy is still scarce, and laparoscopic resection of cirrhotic liver is still considered technically difficult, especially in patients with deranged liver function.
Lesurtel et al[16] reported the results of 16 laparoscopic left lateral segmentectomies for benign liver diseases, HCC and metastasis. Compared with laparotomy, laparoscopic left lateral lobectomy displayed longer operation time (202 min vs 145 min, P < 0.01) and longer portal triad clamping time (39 min vs 23 min, P < 0.05), but less blood loss (236 mL vs 429 mL, P < 0.05). The morbidity rate of the laparoscopic group was 11% and that of the open group was 15%. No death occurred. No specific complication of hepatic resection (hemorrhage, subphrenic collection, biliary leak) was observed after the laparoscopic operation, but in the open group there were some such complications.
Wounds created by laparoscopic surgery are generally smaller than those made by open surgery. In laparoscopic hepatic surgery, 4 to 5 ports are used, each measuring 5 mm to 12 mm only, so the wounds are smaller than those in traditional hepatectomy, resulting in less severe pain and smaller dosage of postoperative narcotics. The risk of incisional hernia after laparoscopic liver resection is also lower. Moreover, shorter hospital stay is observed. In most studies, the mean hospital stay after laparoscopic hepatectomy was 2 d shorter than that after open hepatectomy[16-18].
Another generally observed advantage of laparoscopic surgery over open resection is that it causes less scarring and less adhesion. Future hepatectomy and repetition of laparoscopic resection for recurrent HCC thus become feasible. Abdominal postsurgical adhesions develop following mesothelial trauma, which can be caused by surgical handling and contact of instruments and foreign materials such as sutures and glove dusting powder, as well as by desiccation and overheating. Postoperative adhesions occur after most surgical procedures and can result in serious complications including intestinal obstruction, infertility and pain. This is a long-term unpredictable problem and impacts surgical workload and hospital resources, resulting in considerable healthcare expenditure[19-21].
Adhesions result from normal peritoneal wound-healing response and develop in the first five to seven days after injury. Adhesion formation and adhesion-free re-epithelialization are the two alternative pathways, and both begin with coagulation which initiates a cascade of events resulting in the build-up of fibrin gel matrix. If not removed, the fibrin gel matrix may become the progenitor of adhesion by forming a band or bridge when two peritoneal surfaces coated with it are apposed. The band or bridge is the basis for organization of adhesion. Protective fibrinolytic enzyme systems of the peritoneum, such as the plasmin system, can remove the fibrin gel matrix. However, surgery dramatically diminishes fibrinolytic activity. The apposition of two damaged surfaces and the extent of fibrinolysis are pivotal in determining whether the pathway taken is adhesion formation or adhesion-free re-epithelialization[20,22].
Oncologic clearance is an important issue in laparoscopic liver resection. Risks of tumor-cell seeding and port-site metastasis are of great concern. In the early era of laparoscopic surgery in the management of malignant diseases, it was particularly worrying that pneumoperitoneum would increase tumor seeding and promote peritoneal or even intraportal spread[23]. In the first operation of the present case, the tumor to be resected was maintained intact and put in a plastic specimen bag before removal through the subumbilical port[24,25]. The tumor resection margin was 1 cm. This was to minimize the risk of tumor seeding during laparoscopic handling of the malignant tissue. In the second operation, the laparoscopic approach was again adopted for resection of the recurrent tumor because it was well localized, without invasion to any major vessel or organ, and free of adhesion. It was proven technically feasible to resect the tumor with a clear margin.
Elderly patients and patients having multiple diseases are prone to morbidity and mortality instigated by open hepatectomy. Choices of surgical management are relatively limited when the possibility of complications is taken into consideration. Minimally invasive surgery provides a chance of complete surgical resection of recurrent tumors for these patients. In the present case, the patient underwent two hepatic resections completed in the laparoscopic approach under general anesthesia within 13 mo and recovered well without complications. This is, to our knowledge, the first report regarding repeated laparoscopic hepatectomy in an elderly HCC patient with cirrhosis.
Laparoscopic hepatectomy demands a high level of technical skill, especially when bleeding is anticipated. Control of major vessel bleeding is difficult and there may be indications of conversion. With recent advancement in laparoscopic instruments, laparoscopic surgical difficulties are decreasing. Various instruments have been designed for safe transection of the liver. In the present case, we adopted a combined use of radiofrequency ablation, ultrasonic dissector, endoscopic CUSA, and endovascular stapler. We completed the liver transection by applying the endovascular stapler to the Glisson’s pedicle of the left lateral segment. This stapling technique makes it fast and safe to control hepatic pedicles with an outside chance of complications, and is widely employed in both the open approach and the laparoscopic approach because it reduces the risk of bleeding and shortens operation time[8,9,12,26,27].
Owing to anticipated technical difficulties and the possibility of bleeding during surgery, laparoscopic hepatectomy is still not a common practice amongst most hepatic surgeons. However, it is given recognition for causing less intraoperative blood loss, intractable ascites, encephalopathy and other complications of decompensation of cirrhosis. These advantages can partly be attributed to good illumination and magnification in laparoscopy. Magnification in laparoscopy can be increased up to five times without compromise of the visual field and allows even small vessels to be clearly identified, which helps in decreasing blood loss. The performance of diagnostic ultrasonographic assessment of laparoscopy can avoid unnecessary laparotomy for tumors that are too advanced.
In conclusion, laparoscopic hepatectomy for HCC is a good alternative to open hepatectomy because it has advantages including causing less adhesion after surgery, which renders re-operation much easier in cases of recurrence. It is a comparatively less invasive procedure that offers a chance of surgical clearance of tumors. Further studies with greater numbers of patients and longer follow-up are needed for a better perspective regarding the role of laparoscopic hepatectomy in the management of HCC.
Peer reviewer: Martin Schilling, Professor, Department of Surgery, University of Saarland, Kirrbergerstrasse, Homburg 66424, Germany
S- Editor Wang YR L- Editor Logan S E- Editor Ma WH
| 1. | Descottes B, Lachachi F, Sodji M, Valleix D, Durand-Fontanier S, Pech de Laclause B, Grousseau D. Early experience with laparoscopic approach for solid liver tumors: initial 16 cases. Ann Surg. 2000;232:641-645. |
| 2. | Ardito F, Tayar C, Laurent A, Karoui M, Loriau J, Cherqui D. Laparoscopic liver resection for benign disease. Arch Surg. 2007;142:1188-1193; discussion 1193. |
| 3. | Descottes B, Lachachi F, Durand-Fontanier S, Sodji M, Pech de Laclause B, Valleix D. [Laparoscopic treatment of solid and cystic tumors of the liver. Study of 33 cases]. Ann Chir. 2000;125:941-947. |
| 4. | Poon RT, Fan ST, Lo CM, Liu CL, Wong J. Intrahepatic recurrence after curative resection of hepatocellular carcinoma: long-term results of treatment and prognostic factors. Ann Surg. 1999;229:216-222. |
| 5. | Belli G, Fantini C, D'Agostino A, Belli A, Russolillo N. Laparoscopic liver resections for hepatocellular carcinoma (HCC) in cirrhotic patients. HPB (Oxford). 2004;6:236-246. |
| 6. | Belli G, Fantini C, D'Agostino A, Belli A, Langella S. Laparoscopic hepatic resection for completely exophytic hepatocellular carcinoma on cirrhosis. J Hepatobiliary Pancreat Surg. 2005;12:488-493. |
| 7. | Abdel-Atty MY, Farges O, Jagot P, Belghiti J. Laparoscopy extends the indications for liver resection in patients with cirrhosis. Br J Surg. 1999;86:1397-1400. |
| 8. | Belli G, Fantini C, D'Agostino A, Belli A, Cioffi L, Russolillo N. Laparoscopic left lateral hepatic lobectomy: a safer and faster technique. J Hepatobiliary Pancreat Surg. 2006;13:149-154. |
| 9. | Chen HY, Juan CC, Ker CG. Laparoscopic liver surgery for patients with hepatocellular carcinoma. Ann Surg Oncol. 2008;15:800-806. |
| 10. | Cherqui D, Husson E, Hammoud R, Malassagne B, Stéphan F, Bensaid S, Rotman N, Fagniez PL. Laparoscopic liver resections: a feasibility study in 30 patients. Ann Surg. 2000;232:753-762. |
| 11. | Samama G, Chiche L, Bréfort JL, Le Roux Y. Laparoscopic anatomical hepatic resection. Report of four left lobectomies for solid tumors. Surg Endosc. 1998;12:76-78. |
| 12. | Belli G, Fantini C, D'Agostino A, Cioffi L, Langella S, Russolillo N, Belli A. Laparoscopic versus open liver resection for hepatocellular carcinoma in patients with histologically proven cirrhosis: short- and middle-term results. Surg Endosc. 2007;21:2004-2011. |
| 13. | Laurent A, Cherqui D, Lesurtel M, Brunetti F, Tayar C, Fagniez PL. Laparoscopic liver resection for subcapsular hepatocellular carcinoma complicating chronic liver disease. Arch Surg. 2003;138:763-769; discussion 769. |
| 14. | Cherqui D, Laurent A, Tayar C, Chang S, Van Nhieu JT, Loriau J, Karoui M, Duvoux C, Dhumeaux D, Fagniez PL. Laparoscopic liver resection for peripheral hepatocellular carcinoma in patients with chronic liver disease: midterm results and perspectives. Ann Surg. 2006;243:499-506. |
| 15. | Ker CG, Chen HY, Juan CC, Chang WS, Tsai CY, Lo HW, Yau MT. Laparoscopic subsegmentectomy for hepatocellular carcinoma with cirrhosis. Hepatogastroenterology. 2000;47:1260-1263. |
| 16. | Lesurtel M, Cherqui D, Laurent A, Tayar C, Fagniez PL. Laparoscopic versus open left lateral hepatic lobectomy: a case-control study. J Am Coll Surg. 2003;196:236-242. |
| 18. | Morino M, Morra I, Rosso E, Miglietta C, Garrone C. Laparoscopic vs open hepatic resection: a comparative study. Surg Endosc. 2003;17:1914-1918. |
| 19. | Ergul E, Korukluoglu B. Peritoneal adhesions: facing the enemy. Int J Surg. 2008;6:253-260. |
| 20. | Senthilkumar MP, Dreyer JS. Peritoneal adhesions: pathogenesis, assessment and effects. Trop Gastroenterol. 2006;27:11-18. |
| 21. | Stanciu D, Menzies D. The magnitude of adhesion-related problems. Colorectal Dis. 2007;9 Suppl 2:35-38. |
| 22. | Cheong YC, Laird SM, Li TC, Shelton JB, Ledger WL, Cooke ID. Peritoneal healing and adhesion formation/reformation. Hum Reprod Update. 2001;7:556-566. |
| 23. | Chen WS, Lin W, Kou YR, Kuo HS, Hsu H, Yang WK. Possible effect of pneumoperitoneum on the spreading of colon cancer tumor cells. Dis Colon Rectum. 1997;40:791-797. |
| 24. | Zmora O, Weiss EG. Trocar site recurrence in laparoscopic surgery for colorectal cancer. Myth or real concern? Surg Oncol Clin N Am. 2001;10:625-638. |
| 25. | Zmora O, Gervaz P, Wexner SD. Trocar site recurrence in laparoscopic surgery for colorectal cancer. Surg Endosc. 2001;15:788-793. |