INTRODUCTION
Although tuberculosis (TB) can affect all human organs, the most commonly affected region is the lung[1]. Among the extra-pulmonary patterns, bones and the urinary system are the most frequently affected (30% and 24%, respectively), followed by lymph nodes (13%) and other localizations[1]. It is estimated that 1.3 million cases of TB and 450 000 deaths due to TB occur worldwide annually[1].
Intestinal TB is rare in Western countries[2], with incidence rates of 35.7 and 0.43 per 100 000 per year for the immigrant and native populations, respectively[3]. Despite a clear increase in the frequency of extra-pulmonary TB in immuno-suppressed patients, the clinical features of intestinal TB are rarely seen[3]. Blind gut and ileum are the most common gastrointestinal localizations, while appendix involvement is infrequent. Prompt diagnosis is dependent on a high index of suspicion as clinical signs may be non-specific and microbiological confirmation is difficult. Furthermore, the tuberculin skin test and chest radiograph may initially be negative in as many as 50% of patients[4]. We report a case of appendicular TB and the difficulty in its diagnosis.
CASE REPORT
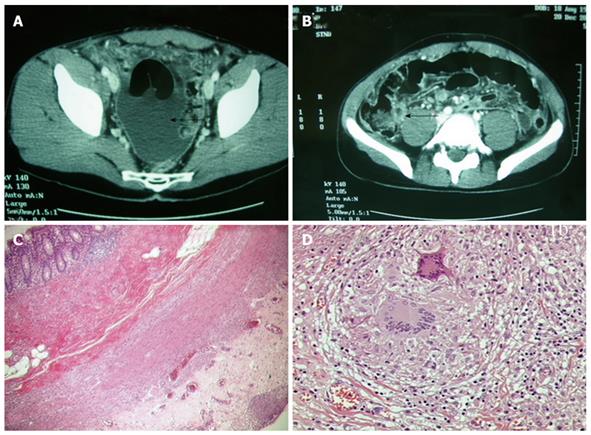
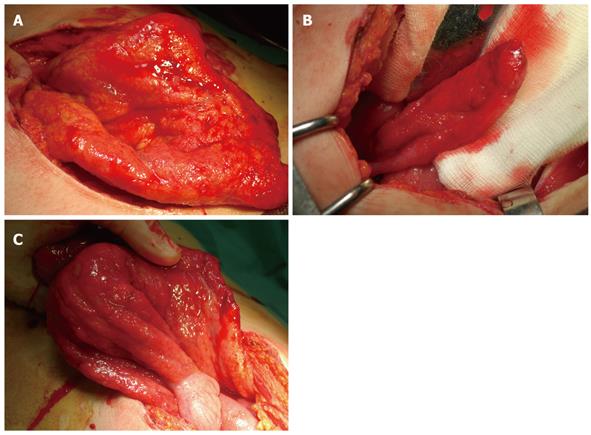
A 25-year-old male was admitted to the Infective Diseases Department of our hospital with asthenia and a light evening temperature since about a month. Backache and earache were also present. The patient was an Italian white man who had not traveled to foreign countries in the recent past. During the last two weeks the patient had a high temperature (up to 40°C), together with nausea and vomiting. The physical examination showed signs of bilateral pleural deposit, globoid abdomen, tense and hardly manageable but still canalized to gas and feces. Clinical examination only showed enhancement of the sedimentation rate. After a first assessment with thoracic X-ray and abdominal ultrasound (US) examination which demonstrated the presence of thoracic and modest abdominal fluid deposit, the patient underwent a thoracic and abdominal computed tomography (CT)-scan which confirmed the presence of a light bilateral pleural deposit, heavier on the right side, ascites and an unexpected appreciable peritoneal deposit (Figure 1A). This was associated with a solid-liquid bilobate formation of about 8 cm in diameter, with a thickened wall and peripheral enhancement (Figure 1B). The CT-scan did not describe or identify the origin of the formation from the ileum or the appendix and the patient was promptly transferred to our department and submitted to surgery, which consisted of an explorative laparoscopy soon converted to laparotomy with appendectomy and omentectomy. At a first view after laparotomy, the abdomen seemed to be affected by a diffuse peritoneal carcinosis (Figure 2A), however, on closer inspection showed the presence of a diffuse micro-nodular aspect involving the bowels and omentum, and tenacious adhesions especially in the appendix-ileum-blind gut region were identified (Figure 2B). The aspect was diffusely inflammatory (Figure 2C), hyperemic and edematous and was soon defined as “military” in the operative theater. A diagnosis of TB was suspected and was confirmed by definitive histopathological examination, which described the presence of “granulomatous nodular epithelioid appendicitis and mesenteritis with gigantic and Langhans cells and diffuse caseous necrosis” (Figure 1C-D). The patient was started on specific antibiotic therapy for two months consisting of daily doses of isoniazid 400 mg, rifampicin 600 mg and pirazinamide 2 g, followed by four months of isoniazid and rifampicin therapy; the treatment lasted six months and the patient made a complete recovery without complications. One, three, six and twelve months after antibiotic therapy, the patient showed no signs of recurrence on thoracic X-ray and expectorate culture.
Figure 1 CT scan pre-operative images and histopathological images.
A: CT-scan image showing relevant amount of fluid in the Douglas; B: CT-scan image showing clear thickening of the appendicular wall (arrows) and “target” image as an evident sign of appendicitis; C, D: Histopathological aspects of the bioptic and resected samples.
Figure 2 Specimen after laparotomy.
A: Diffuse military aspect, simulating a peritoneal carcinosis; B: Tenacious adhesions in the appendix-ileum-blind gut region; C: Diffuse inflammatory, hyperemic and edematous aspects of the intestine.
DISCUSSION
According to the WHO Report of 2009 (WHO/HTM/TB/2009.411) an estimated one third of the world’s population is infected with Mycobacterium tuberculosis, and nearly 9 million people develop disease caused by M. tuberculosis each year. This resurgence is accompanied by a rise in multidrug-resistant TB (MDR TB), which is resistant to the two most effective first-line therapeutic drugs, isoniazid and rifampicin. In addition, virtually untreatable strains of M. tuberculosis are emerging globally. Extensively drug-resistant TB (XDR TB) is MDR TB that is also resistant to the most effective second-line therapeutic drugs used commonly to treat MDR TB; these drugs are fluoroquinolones and at least one of three injectable second-line drugs used to treat TB (amikacin, kanamycin, or capreomycin). XDR TB has been identified in all regions of the world. Because of the limited responsiveness of XDR TB to available antibiotics, mortality rates among patients with XDR TB are similar to those of TB patients in the pre-antibiotic era[5]. The peritoneum is one of the most common extra-pulmonary sites of TB infection. Peritoneal TB remains a significant problem in parts of the world where TB is prevalent. Increasing population migration, the use of more potent immuno-suppressant therapies and the acquired immunodeficiency syndrome epidemic have contributed to a resurgence of this disease in regions where it had previously been largely controlled[6]. Gastrointestinal TB can occur as a primary or secondary form: the first form is due to a primary infection of the intestinal mucosa by Mycobacterium bovis; the second form is usually a consequence and complication of primary pulmonary TB by M. tuberculosis. It may involve any part of the intestinal tract but the most common localizations are the ileum, the blind gut and the ascending colon. Appendicular TB is rare and of uncertain physiopathological etiology. Several authors agree that the appendix as a secondary localization by a more frequent ileum, cecal or genital infection due to blood contamination[7]. In our case, no signs of TB involvement were detected other than in the appendix itself, and all the other CT aspects were compatible with reactive signs and referable to the appendicular infection. This led us to consider it as a primary localization of TB since there was no other way to distinguish it from a secondary infection in the absence of other demonstrable localizations. Histopathological examination distinguishes three types of intestinal TB: the ulcerative form, which represents 60% of all cases and the hypertrophic and ulcer-hypertrophic forms, which represent 10% and 30%, respectively, of the remaining cases. Clinical presentation is usually dominated by ascites (100%), fever (76.2%) and abdominal pain (73.8%)[8]. Signs and symptoms of abdominal TB are nonspecific and similar to those of several other chronic abdominal diseases such as Crohn’s syndrome; otherwise it may simulate an acute appendicitis such as the present case. It is very important to make a correct differential diagnosis, but in most cases this is not possible until histopathological examination is carried out, which is almost always after surgery. The diagnosis of a secondary localization by a pulmonary infection is usually more simple since the radiological aspects of pulmonary TB are often characteristic and a secondary interest in the bowel become at least assumable. In the case of a primary abdominal infection there are no characteristic radiological or serological signs and a presumptive diagnosis is really difficult to make. In these cases, great attention should be paid to the history of the patients and their contact with active TB[9]. Other than surgical diagnosis, when TB is first suspected a tuberculin skin test (TST) should be carried out although the positivity has been reported to be only 18%-27%[10-12] in several studies. The literature also shows that culture positivity of peritoneal fluid is rarely seen[11,13-15]. High levels of adenosine deaminase (ADA) in the ascitic fluid have been shown to be compatible with the diagnosis of TB with high sensitivity (100%) and specificity (97%), but the analysis of ADA activity may not be available everywhere[15-17]. US can also be useful in detecting ascites and, in very expert hands, the caseous necrosis causing hypoechogenic centers of the bloated lymph nodes[9,15]. The most accurate diagnostic alternative to surgery may be endoscopic biopsy of the lesions, but this still depends on the localization of the lesion itself (impossible in a case such as ours) and on the gravity of the case, possibly requiring urgent surgery. Serum tests are usually negative, other than nonspecific inflammatory signs, similar to radiological signs, which are evident but not specific for suspected TB such as mucosal wall thickening, distortions of the intestinal crests, ulcers and stenosis. During laparoscopy or open surgery, the intestinal wall appear thicker and it is usually possible to identify an inflammatory mass near the ileum-cecal region; mesenteric lymph nodes are frequently bloated and hardened with a caseous necrosis; the mucosa is often hyperemic, edematous and sometimes infected. Cytology shows the presence of Langhans cells. With or without surgical intervention, antibiotic therapy is always necessary and is similar to that of the pulmonary forms, consisting of isoniazid 300 mg/d, etambutol 15 mg/kg per day, and rifampicin 600 mg/d. Many authors suggest combining corticosteroid administration with specific antibiotic treatment to reduce the complications of abdominal TB[18-20].
In conclusion, appendicular tuberculosis is a very rare occurrence but still a significant cause of morbidity and mortality worldwide. In the absence of specific symptoms and signs, its diagnosis is delayed, thus resulting in a high percentage of important, and sometimes lethal, complications. An assumed diagnosis of TB should be made in all patients presenting with ascites not liver related, accompanied by fever and abdominal pain. Appendicular TB is more frequent in younger patients and especially in these cases, when surgery is not yet necessary, TST, ADA peritoneal activity, culture of peritoneal fluid or endoscopic biopsy should be performed. Moreover, in patients with features similar to peritoneal carcinosis seen during surgery, TB in its military form should always be suspected. Histopathological examination after surgery for acute appendicitis often remains the only way to reach a secure diagnosis and to establish the best therapy, since surgery is often necessary but specific antibiotic therapy must be started as soon as possible. We are all seeing a resurgence of this old disease even in developed countries where it was thought to have disappeared. This is probably due to the migration of a great, and not always controlled, number of people from countries where TB still has a high incidence. The only way to resolve this problem is prophylaxis and prevention worldwide, but in the meanwhile a renewed acquaintance with this old disease is imperative.