Published online Oct 7, 2010. doi: 10.3748/wjg.v16.i37.4733
Revised: March 26, 2010
Accepted: April 2, 2010
Published online: October 7, 2010
AIM: To investigate the clinical application of ultrasonic elastography in quantitative assessment of fatty liver grading.
METHODS: A total of 105 patients with fatty liver were divided into mild group (n = 46), moderate group (n = 39), and severe group (n = 20). Forty-five healthy individuals served as a normal control group. All patients who underwent routine ultrasound scan and further ultrasonic elastography were evaluated accordingly to the evaluation standards for ultrasonic elastography. The ratio of surface areas of blue region/total surface area in the desired region was measured.
RESULTS: Ultrasonic elastography technique, in comparison to traditional ultrasound, had a rather high consistence in grading of fatty liver [κ value = (95.3%-63.6%)/(1%-63.6%) = 0.87, P = 0.001]. The score of ultrasonic elastography increased with the severity of fatty liver with a sensitivity of 97.14% and a specificity of 91.11%. A significant difference was found in the ratio of surface areas of blue regions between different groups (P < 0.05).
CONCLUSION: Ultrasonic elastography can be used in quantitative assessment of the severity of fatty liver.
- Citation: Li YY, Wang XM, Zhang YX, Ou GC. Ultrasonic elastography in clinical quantitative assessment of fatty liver. World J Gastroenterol 2010; 16(37): 4733-4737
- URL: https://www.wjgnet.com/1007-9327/full/v16/i37/4733.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i37.4733
Fatty liver is one of the important hepatic diseases in China and a threat to the public health. Moderate fatty liver can lead to significant necrosis and inflammation in hepatocytes. Severe fatty liver can lead to fibrosis and pseudo-lobe formation. If it is not immediately controlled or appropriately treated, the condition can progress to liver cirrhosis. No better and convenient auxiliary examination is currently available for the objective evaluation of fatty liver grading.
In recent years, ultrasonic imaging technique has transformed to functional imaging from anatomical imaging. Ultrasonic elastography technique is one of the new functional ultrasonic imaging techniques, which was developed in the past few years and can be used in quantitative and semi-quantitative assessment of diffused lesions in liver, such as cirrhosis after hepatitis, alcoholic cirrhosis, hepatic dysfunction after surgery, and other diseases[1-4]. Although many researchers have employed ultrasonic elastography in study of chronic hepatic diseases, few studies are available on the diagnosis of fatty liver[5,6]. This study was to investigate its application in clinical quantitative assessment of fatty liver grading.
Color ultrasonic equipment model HV900 with a linear probe and a frequency of 4-9 MHz was purchased from HITACHI Company (Japan).
One hundred and five patients with diagnosed fatty liver in the First Affiliated Hospital of China Medical University between November 2008 and March 2009, were divided into mild group (n = 46), moderate group (n = 39), and severe group (n = 20). Forty-five healthy individuals served as a control group. Their fatty liver was graded as previously described[7-10]. Informed consent was obtained from each patient.
The inclusion criteria for normal liver were as follows: smooth hepatic capsule with a linear hyperechogenicity, left lobe with a sharp edge and left outer edge with an angle < 45°, evenly distributed iso-echo in hepatic parenchyma, intrahepatic pipeline system with a normal distribution and well sound-transparent power similar to the normal renal parenchyma echo, clear hepatic and portal vein with unobstructed blood flow, no expanded intrahepatic bile duct, normal liver function, and negative hepatitis test.
Patients were placed in supine position and the 8th or 9th intercostal space was selected as the scanning site. Appropriate depth and enhancement were adjusted. The function of elastography was initiated, then the size of desired region was identified (2 cm above and below the boundary of desired region, and the width was not limited) with vascular branches avoided and pressure index strictly controlled at level 2 or 3.
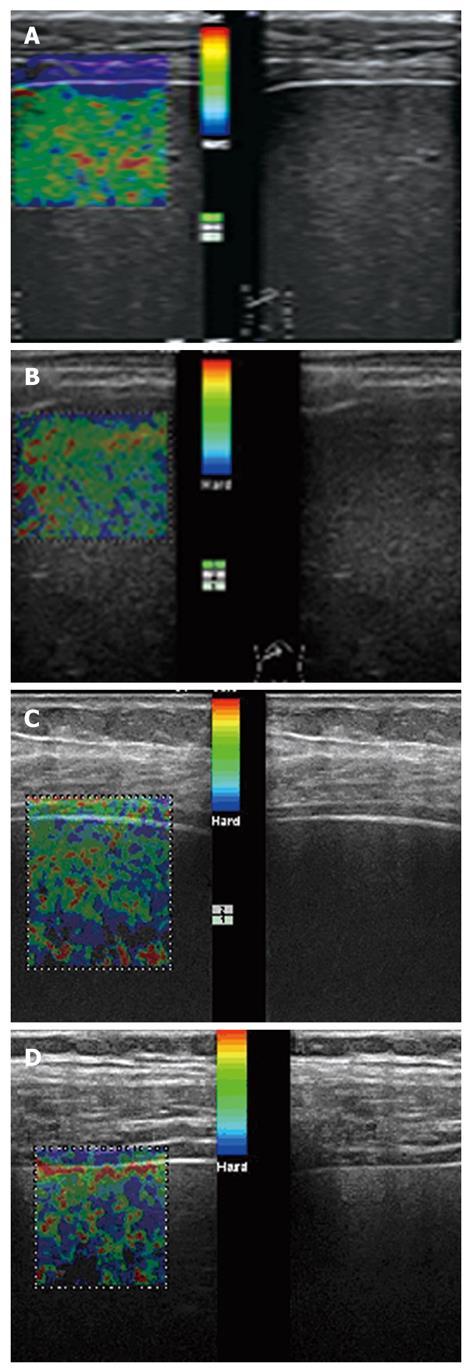
Images were evaluated according to the following standards: one score: a few blue dots in green region of elasticity image with liver membrane blue colored, two scores: liver elasticity image primarily green colored with a few blue spots and liver membrane blue colored, three cores: obvious blue region (< 1/2 of desired region) in elasticity image and liver membrane green colored, four scores: more obvious blue region (> 1/2 of desired region) in elasticity image and liver membrane red colored (Figure 1). These images were evaluated by two physicians with 6-year experience.
Ultrasonic elastography was performed and the image showed the quasi-circular blue area in the desired image region. The sum of surface area of each blue region was measured on 2D image, and defined as the total surface area of blue regions. The ratio of surface area of blue region was calculated according to the following equation: The ratio of surface area of blue region (BAR) = total surface area of blue regions/total surface area in desired region.
Statistical analysis was performed using SPSS 13.0 software. Numeral data were analyzed viaκ value to test the consistency of traditional ultrasound and ultrasonic elastography in grading of fatty liver. Quantitative data were expressed as mean ± SD. t-test was used for intergroup comparison of averages. P < 0.01 was considered statistically significant.
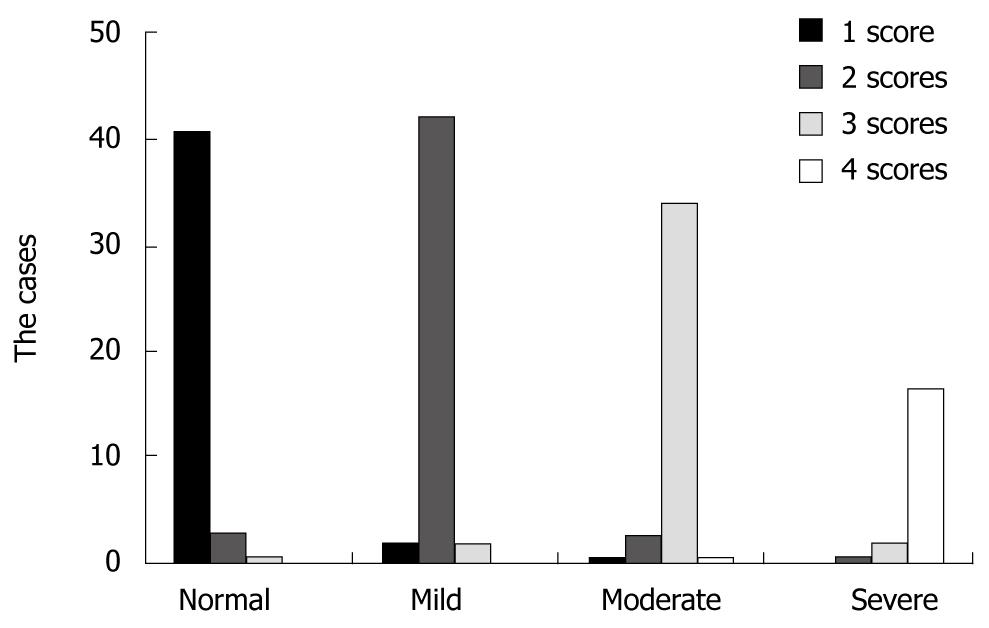
The results of ultrasonic elastography were as follows. Of the 45 patients in control group, 41 had one score, 3 had two scores, and 1 had three scores. Of the 46 patients in mild group, 42 had two scores, 2 had one score, and 2 had three scores. Of the 39 patients in moderate group, 34 had three scores, 1 had one score, 3 had two scores, and 1 had four scores. Of the 20 patients in severe group, 17 had four scores, 2 had three scores, and 1 had two scores. The observed consistency rate was 95.3%, the chanced consistency rate was 63.8%, the κ value was 0.87 (P = 0.001). κ analysis showed that the consistency of ultrasonic elastography and traditional ultrasound was high in grading of fatty liver, where the κ value was 0.87 (Table 1).
| Traditional ultrasound | Elastography | Total | |||
| 1 score | 2 scores | 3 scores | 4 scores | ||
| Normal | 41 | 3 | 1 | 0 | 45 |
| Mild | 2 | 42 | 2 | 0 | 46 |
| Moderate | 1 | 3 | 34 | 1 | 39 |
| Severe | 0 | 1 | 2 | 17 | 20 |
| Total | 44 | 49 | 39 | 18 | 150 |
The score of ultrasonic elastography increased with the severity of fatty liver (Figure 2). The primary score of ultrasonic elastography was 1, 2, 3 and 4, respectively in control, mild, moderate, and severe groups, accounting for 91.1%, 91.3%, 87.1%, and 85.0% of each group, respectively.
All the 150 patients underwent examination. Of the 105 patients who were diagnosed as fatty liver by traditional ultrasound, 102 were diagnosed as fatty liver and 3 as normal by ultrasonic elastography, Of the 45 patients who were diagnosed as normal by traditional ultrasonic examination, 41 were diagnosed as normal and 4 as fatty liver by ultrasonic elastography with a sensitivity of 97.14% and a specificity of 91.11% (Table 2).
| Traditional ultrasound | Elastography | Total | |
| Positive | Negative | ||
| Positive | 102 | 3 | 105 |
| Negative | 4 | 41 | 45 |
| Total | 106 | 44 | 150 |
The BAR value was 0.0943 ± 0.0851, 0.1947 ± 0.0582, 0.3242 ± 0.0662, and 0.5005 ± 0.0943, respectively, in control, mild, moderate, and severe groups (P < 0.001), which increased with the severity of fatty liver.
Ultrasonic elastography is a brand new ultrasonic technique. Its basic principle relies on the application of dynamic or static/semi-static stimulation from an intrinsic (including autonomous) or extrinsic source of tissues. Under physical regulation of elastic mechanics and biomechanics, tissues would generate a strain as a response to relocation, reactions, and possibly a certain change in the speed, which is shown as a disturbance in distribution. Therefore, ultrasonic elastography can obtain quantitative information on distributions of elasticity in tissues. Currently, these distributions are marked by various colors, including red, blue, yellow, and green, with blue representing sclerosis and red representing softness. Many types of ultrasonic elastography available at present, can be divided into strain elastography which produces an imaging of pressure by comparing differences in tissues before and after the operator applies a certain force, transient elastography which discovers relocation of tissues once transient vibration is applied at a low frequency, and vibration sonoelastography which produces a resonance image of tissues once vibration is applied at a low frequency[11]. Different manufacturers of ultrasonic equipments would design software systems for ultrasonic elastography based on different imaging principles. The first technique, strain imaging, is more susceptible to human factors. Strain and relocation can vary greatly due to different pressures and frequencies of pressure. In order to compensate for such variations, the instrument is equipped with a display device to show the comprehensive indices such as pressures and frequencies of pressure.
Since the invention of ultrasonic elastography, it has been applied to the detection of masses and lesions in mammary and liver tissues, thus, more research results on mammary lesions are available[12,13].
Fatty liver, also known as intra-hepatic lipid degeneration, is caused by accumulation of lipid in liver due to various reasons. In fact, lipid is accumulated in normal liver, accounting for 5% of fresh liver. When the amount of lipid is over 5% in liver, it is defined as fatty liver, where lipids are mostly in a form of triacylglycerol. Based on the amount of lipids in liver, fatty liver is further divided into mild (accounting 5%-10% of fresh liver), moderate (accounting for 10%-25% of fresh liver), and severe (accounting for over 25% of fresh liver). With the aggravation of fatty liver, hepatic fibrosis also worsens. Currently, ultrasonic examination is the most preferable diagnostic method for fatty liver. However, it costs more and no objective index is available. Therefore, ultrasonic elastography was performed to detect hepatic fibrosis in patients with fatty liver in this study, which showed significant variations in different groups. The images of control group showed evenly distributed green color with few red dots. As fatty liver worsened, more blue regions gradually appeared and the color of liver enveloping membrane was also significantly changed, indicating that ultrasonic elastography can provide more direct real-time images. Therefore, ultrasonic elastography can be used in detection and diagnosis of fatty liver and scores of ultrasonic elastography can be used as an auxiliary diagnostic index for fatty liver.
Liu et al[14] believed that subcutaneous fat is not related to the severity of fatty liver but is an interfering factor for elastography. When subcutaneous fat between skin and liver enveloping membrane is over 3 cm and the liver is situated in depth, it would be difficult to obtain good elastography images. In this study, the subcutaneous fat between skin and liver enveloping membrane was over 3.1 cm in 3 patients, and elastography images with a better resolution were not obtained. Del Poggio et al[15] also believed that instant elastography cannot reliably determine fatty liver if the patient is obese.
In this study, the consistency of traditional ultrasound and ultrasonic elastography was rather high in grading of fatty liver (κ value > 0.75) with a sensitivity of 97.14% and a specificity of 91.11%, indicating that ultrasonic elastography can be used in grading of fatty liver. Liver biopsy has been recognized as the gold standard for diagnosing hepatic fibrosis, but it leads to severe complications and false negative results[16-19]. The complications of liver biopsy include post biopsy pain, bleeding, organ perforation, and even death. Taking into account the complications of liver biopsy, we did not perform it.
Ultrasonic elastography relies on the strain imaging, which requires application of certain pressures before it is formed. This technique requires highly skilled operators due to its rigorous operating criteria, such as the size and location of sample window, range of scan, enhancement of 2D image, and control of pressure index, which would affect the research results.
Blue region in the desired region represents the hardness of tissues and the increased blue region indicates the severity of fatty liver. Our study showed that an increased BAR value when fatty liver worsened, suggesting that BAR value can be used as a quantitative index for the severity of fatty liver.
Friedrich-Rust et al[20] showed that ARFI imaging is a promising US-based method for the assessment of liver fibrosis in chronic viral hepatitis, with a similar diagnostic accuracy of TE. However, it also has some inadequacies.
In conclusion, ultrasonic elastography technique can be used as an auxiliary examination for the assessment of fatty liver. It provides new clinical diagnostic indicators and is able to reduce the false positive and negative rate, thus allowing the doctors to make the right diagnosis in a limited time.
Ultrasonic elastography technique is one of the new functional ultrasonic imaging techniques, which is developed over the past few years and can be used for quantitative and semi-quantitative assessment of liver sclerosis and diffused lesions.
Ultrasonic elastography is a brand new ultrasonic technique. Since the invention of ultrasonic elastography, it has been applied to mammary tissues with more research results on mammary lesions available.
The clinical application of ultrasonic elastography in quantitative assessment of the severity of fatty liver was studied.
This research showed the area of blue region value can be used as a quantitative index for the severity of fatty liver.
In this study, the authors showed that ultrasonic elastography can be used as an auxiliary examination for the quantificational assessment of fatty liver. It would be more interesting if biopsies were done in those with fatty liver.
Peer reviewers: Søren Rafaelsen, MD, Consultant Radiologist, Associate Professor, Department of Radiology, Vejle Hospital, Vejle, 7100, Denmark; Bernardo Frider, MD, Professor, Department of Hepatology, Hospital General de Agudos Cosme Argerich, Alte Brown 240, Buenos Aires 1155, Argentina
S- Editor Wang JL L- Editor Wang XL E- Editor Ma WH
| 1. | Castera L, Forns X, Alberti A. Non-invasive evaluation of liver fibrosis using transient elastography. J Hepatol. 2008;48:835-847. |
| 2. | Kim SG, Kim YS, Jung SW, Kim HK, Jang JY, Moon JH, Kim HS, Lee JS, Lee MS, Shim CS. [The usefulness of transient elastography to diagnose cirrhosis in patients with alcoholic liver disease]. Korean J Hepatol. 2009;15:42-51. |
| 3. | Kim SU, Ahn SH, Park JY, Kim do Y, Chon CY, Choi JS, Kim KS, Han KH. Prediction of postoperative hepatic insufficiency by liver stiffness measurement (FibroScan((R))) before curative resection of hepatocellular carcinoma: a pilot study. Hepatol Int. 2008;2:471-477. |
| 4. | Di Marco V, Bronte F, Cabibi D, Calvaruso V, Alaimo G, Borsellino Z, Gagliardotto F, Almasio PL, Capra M, Craxì A. Noninvasive assessment of liver fibrosis in thalassaemia major patients by transient elastography (TE) - lack of interference by iron deposition. Br J Haematol. 2010;148:476-479. |
| 5. | de Lédinghen V, Vergniol J. Transient elastography (FibroScan). Gastroenterol Clin Biol. 2008;32:58-67. |
| 6. | Sporea I, Sirli R, Deleanu A, Tudora A, Curescu M, Cornianu M, Lazar D. Comparison of the liver stiffness measurement by transient elastography with the liver biopsy. World J Gastroenterol. 2008;14:6513-6517. |
| 7. | Franzese A, Vajro P, Argenziano A, Puzziello A, Iannucci MP, Saviano MC, Brunetti F, Rubino A. Liver involvement in obese children. Ultrasonography and liver enzyme levels at diagnosis and during follow-up in an Italian population. Dig Dis Sci. 1997;42:1428-1432. |
| 8. | Sanyal AJ. AGA technical review on nonalcoholic fatty liver disease. Gastroenterology. 2002;123:1705-1725. |
| 9. | Palmentieri B, de Sio I, La Mura V, Masarone M, Vecchione R, Bruno S, Torella R, Persico M. The role of bright liver echo pattern on ultrasound B-mode examination in the diagnosis of liver steatosis. Dig Liver Dis. 2006;38:485-489. |
| 10. | Zeng MD, Li YM, Chen CW, Lu LG, Fan JG, Wang BY, Mao YM. Guidelines for the diagnosis and treatment of alcoholic liver disease. J Dig Dis. 2008;9:113-116. |
| 11. | Taylor LS, Porter BC, Rubens DJ, Parker KJ. Three-dimensional sonoelastography: principles and practices. Phys Med Biol. 2000;45:1477-1494. |
| 12. | Melodelima D, Bamber JC, Duck FA, Shipley JA, Xu L. Elastography for breast cancer diagnosis using radiation force: system development and performance evaluation. Ultrasound Med Biol. 2006;32:387-396. |
| 13. | Bercoff J, Chaffai S, Tanter M, Sandrin L, Catheline S, Fink M, Gennisson JL, Meunier M. In vivo breast tumor detection using transient elastography. Ultrasound Med Biol. 2003;29:1387-1396. |
| 14. | Liu KH, Chan YL, Chan JC, Chan WB, Kong WL. Mesenteric fat thickness as an independent determinant of fatty liver. Int J Obes (Lond). 2006;30:787-793. |
| 15. | Del Poggio P, Colombo S. Is transient elastography a useful tool for screening liver disease? World J Gastroenterol. 2009;15:1409-1414. |
| 16. | McHutchison J, Poynard T, Afdhal N. Fibrosis as an end point for clinical trials in liver disease: a report of the international fibrosis group. Clin Gastroenterol Hepatol. 2006;4:1214-1220. |
| 17. | Regev A, Berho M, Jeffers LJ, Milikowski C, Molina EG, Pyrsopoulos NT, Feng ZZ, Reddy KR, Schiff ER. Sampling error and intraobserver variation in liver biopsy in patients with chronic HCV infection. Am J Gastroenterol. 2002;97:2614-2618. |
| 18. | Persico M, Palmentieri B, Vecchione R, Torella R, de SI. Diagnosis of chronic liver disease: reproducibility and validation of liver biopsy. Am J Gastroenterol. 2002;97:491–492. |
| 19. | Ratziu V, Charlotte F, Heurtier A, Gombert S, Giral P, Bruckert E, Grimaldi A, Capron F, Poynard T. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology. 2005;128:1898-1906. |