Published online Aug 21, 2010. doi: 10.3748/wjg.v16.i31.3964
Revised: May 12, 2010
Accepted: May 19, 2010
Published online: August 21, 2010
AIM: To evaluate the capacity of 18F-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) for detecting multiple primary cancer of upper gastrointestinal (UGI) tract.
METHODS: Fifteen patients (12 without cancer histories and 3 with histories of upper GI tract cancer) were investigated due to the suspicion of primary cancer of UGI tract on X-ray barium meal and CT scan. Subsequent whole body 18F-FDG PET/CT scan was carried out for initial staging or restaging. All the patients were finally confirmed by endoscopic biopsy or surgery. The detection rate of multiple primary malignant cancers was calculated based on 18F-FDG PET/CT and endoscopic examinations.
RESULTS: 18F-FDG PET/CT scan was positive in 32 suspicious lesions, 30/32 were true positive primary lesions, and 2/32 were false positive. In 15 suspicious lesions with negative 18F-FDG PET/CT scan, 12/15 were true negative and 3/15 were false negative. Among the 15 patients, 12 patients had 29 primary synchronous tumors confirmed by pathology, including 8 cases of esophageal cancers accompanied with gastric cancer and 4 of hypopharynx cancers with esophageal cancer. The other 3 patients had 4 new primary metachronous tumors, which were multiple primary esophageal cancers. PET/CT imaging detected local lymph node metastases in 11 patients. Both local lymph node metastases and distant metastases were detected in 4 patients. On a per-primary lesion basis, the sensitivity, specificity, accuracy, negative predictive value and positive predictive value of 18F-FDG PET/CT for detecting multiple primary cancer of UGI tract were 90.9%, 85.7%, 89.4%, 80% and 93.7%, respectively.
CONCLUSION: The whole body 18F-FDG PET/CT may play an important role in evaluating the multiple primary malignant tumors of UGI tract cancer.
- Citation: Sun L, Wan Y, Lin Q, Sun YH, Zhao L, Luo ZM, Wu H. Multiple primary malignant tumors of upper gastrointestinal tract: A novel role of 18F-FDG PET/CT. World J Gastroenterol 2010; 16(31): 3964-3969
- URL: https://www.wjgnet.com/1007-9327/full/v16/i31/3964.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i31.3964
Metachronous or synchronous esophageal cancer has been identified in patients with head and neck cancer, gastric cancer or colon cancer[1]. Alcohol drinking and tobacco smoking are the major risk factors for upper aerodigestive tract cancers, accounting for a large proportion of cases in developed countries[2,3]. The occurrence of multiple primary cancers in the aerodigestive tract has been explained by the concept of field carcinogenesis. Combined exposure to alcohol and tobacco has a multiplicative effect on carcinogenesis of upper aerodigestive tract[4,5].
X-ray barium meal examination, endoscopic examination, computed tomography (CT) are the main techniques used for the staging and follow-up of upper gastrointestinal (UGI) tract cancer[6,7]. However, the reported increase in sensitivity of 18F-fluorodeoxyglucose positron emission tomography/computed tomography (PET/CT) over CT has been attributed to the capacity of 18F-FDG PET/CT to detect metabolic abnormalities that precede the morphological changes seen by CT. This study was undertaken to further define the value of 18F-FDG PET/CT in evaluating multiple primary metachronous or synchronous cancer of UGI.
Fifteen patients with multiple UGI tract cancer (13 males and 2 female, aged 49-78 years with a mean age of 61 years) were selected for a retrospective review from our electronic database, who were imaged by 18F-FDG PET/CT between January 2007 and January 2010 because of the suspicious findings for multiple UGI tract cancer by the X-ray barium meal and endoscopic examinations. All the patients were finally confirmed by endoscopic biopsy or surgery.
The patients were asked to fast for at least 4 h before undergoing 18F-FDG PET/CT. Their blood glucose level should be within the normal range (70-120 mg/dL) prior to intravenous injection of 18F-FDG. The patients received an intravenous injection of 370-666 MBq (10-18 mCi) of 18F-FDG. Data acquisition by an integrated PET/CT system (Discovery STE; GE Medical Systems, Milwaukee, WI, USA) was performed within 60 min after injection. The procedure of data acquisition was as follows: CT scanning was performed first, from the head to the pelvic floor, with 110 kV, 110 mA, a tube rotation time of 0.5 s, a 3.3-mm section thickness, which was matched to the PET section thickness. Immediately after CT scanning, a PET emission scan covering the identical transverse field of view was obtained. Acquisition time was 3 min per table position. PET image data sets were reconstructed iteratively by applying the CT data for attenuation correction, and coregistered images were displayed on a workstation.
The 18F-FDG PET/CT images were prospectively interpreted by two experienced nuclear physicians. One had 21 years of experience in both nuclear medicine and radiology, and the other had six years of experience in both nuclear medicine and radiology, who read the 18F-FDG PET/CT images on a high-resolution computer screen, and reached a consensus in cases of discrepancy.
Based the knowledge of the normal biodistribution of 18F-FDG, lesions were identified as foci with increased tracer accumulation relative to that in comparable normal contralateral structures and surrounding soft tissues. The lesions were qualitatively graded as definitely or probably abnormal (categorized as representing a tumor) if the accumulation of 18F-FDG was markedly to moderately increased. Diffuse and mildly increased activity or no increased activity (in the case of an abnormality identified on CT, but no corresponding abnormality was present on PET) was considered to be a normal or benign disease.
The results of PET/CT were quantified using the following definitions: accuracy [(true positive) + (true negative)/(total patients)], sensitivity [(true positive)/(true positive + false negative)], specificity [(true negative)/(true negative + false positive)], positive predictive value [(true positive)/(true positive +false positive)], and negative predictive value [(true negative)/(true negative + false negative)].
At the time of multiple primary lesions of suspected UGI cancer, the mean age of the patients was 61 years with a predominant tendency in men. Twelve men and one woman had heavy tobacco and alcohol consumption histories in this group of patients.
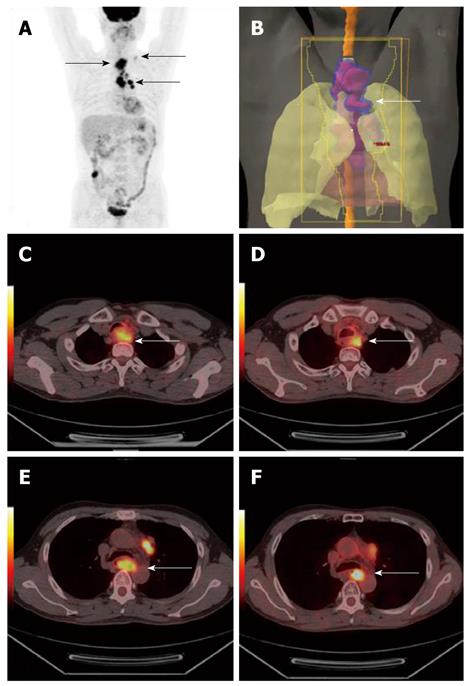
PET/CT is able to demonstrate the entire UGI tract in almost all patients, even following incomplete endoscopic examination due to obstructing upper esophageal tumors in 4 patients (Figure 1). PET/CT imaging is helpful to guide accurately localization of lower esophageal lesions in the remaining patients.
18F-FDG PET/CT scan was positive in 32 suspicious lesions, of which 30 were true positive primary lesions and 2 were false positive. Among 15 suspicious lesions with negative 18F-FDG PET/CT scan, 12 were true negative and 3 were false negative.
On a per-primary lesion basis, sensitivity, specificity, accuracy, negative predictive value and positive predictive value of 18F-FDG PET/CT in detecting multiple primary cancer of UGI tract were 90.9%, 85.7%, 89.4%, 80% and 93.7%, respectively.
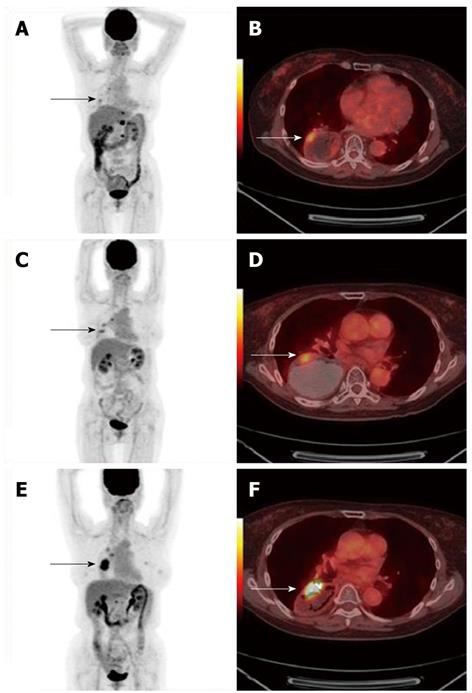
Of the 15 patients, 12 patients had 29 primary synchronous tumors confirmed by pathology (Table 1), including 8 cases of esophageal cancer combined with gastric cancer and 4 had hypopharynx cancer combined with esophageal cancer. The other 3 patients had 4 new primary metachronous tumors (Table 2 and Figure 2).
| Sex/age (yr) | PET/CT findings | Endoscopic results | |||
| T | T | N | M | ||
| F/61 | EPC (lower) | Cardiac | Gastrohepatic | EPC (lower), cardiac | |
| M/60 | Hypopharynx | EPC (mid, lower) | Mediastinal | Hypopharynx | |
| M/62 | EPC (upper) | EPC (lower) | Supraclavicular | EPC (upper) | |
| M/59 | EPC (lower) | Cardiac | Mediastinal, gastrohepatic | EPC (lower), cardiac | |
| M/61 | Hypopharynx | EPC (mid) | Right cervical | Hypopharynx | |
| M/62 | EPC (mid) | Cardiac | Gastrohepatic | EPC (mid), cardiac | |
| M/78 | EPC (lower) | Pylorus | Mediastinal, gastrohepatic | Lung | EPC (lower), pylorus |
| M/57 | EPC (mid, lower) | Cardiac | Mediastinal, gastrohepatic | Lung | EPC (mid, lower) |
| M/52 | EPC (upper) | EPC (mid, lower) | Mediastinal, supraclavicular | EPC (upper, mid) | |
| M/62 | EPC (mid, lower) | Cardiac | Mediastinal, gastrohepatic | Liver | EPC (mid, lower) |
| M/53 | Hypopharynx | EPC (mid, lower) | Cervical, mediastinal, retroperitoneal | Hypopharynx | |
| M/60 | EPC (upper) | EPC (mid) | Supraclavicular, mediastinal | EPC (upper, mid) | |
| Sex/age (yr) | PET/CT findings | Endoscopic results | |||
| Primary | Secondary | N | M | ||
| M/68 | EPC resection 10 yr ago | Hypopharynx | Cervical | Hypopharynx | |
| M/49 | GC resection 25 yr ago | EPC (lower), Cardiac | Supraclavicular | Lung | EPC (lower), cardiac |
| F/63 | EPC resection 5 yr ago | Gastric tube cancer | Retroperitoneal | Gastric tube cancer | |
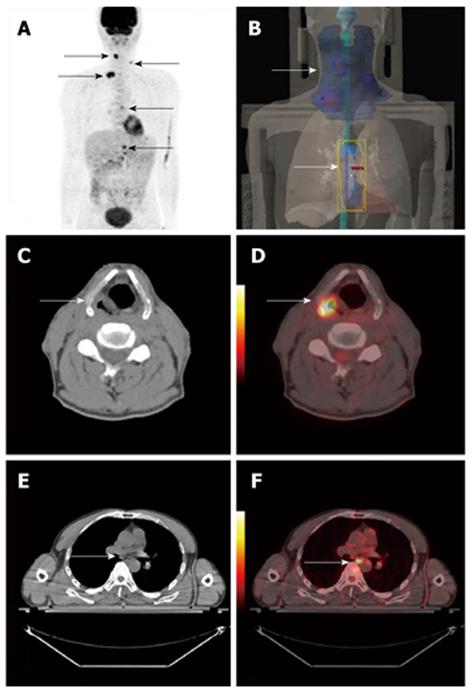
PET/CT imaging detected local lymph node metastases in 11 patients (Figure 3). Both local lymph node metastases and distant metastases were detected in 4 patients.
Clinical treatment plans were changed in 11 (73.3%) patients after PET/CT examination. 18F-FDG PET/CT imaging-guided radiotherapy was performed in 11 patients.
Synchronous cancers were predominantly located in the aerodigestive tract, primarily in the lung, head and neck and esophagus[8]. Kumagai et al[9] reported half of the patients with multiple upper aerodigestive tract squamous cell carcinomas are initially seen with synchronous tumors. It is also believed that these second primary cancers arise independently following exposure to a common carcinogen by a process that has been called field cancerization[10]. At least 75% of head and neck cancers are attributable to a combination of cigarette smoking and alcohol drinking[11]. In our cases, 13 patients (86.7%) had heavy tobacco and alcohol consumption histories. Synchronous tumors of UGI tract were detected in 12 patients. Esophageal cancers combined with gastric cancer (53.3%) were most frequently seen in our study.
Patients with primary head and neck malignancies have a 3%-7% yearly incidence of second primary cancers. Most metachronous squamous cell carcinomas become manifest within 3 years[12]. Detection of second primaries has an important impact on therapy. For the patients treated for advanced squamous cell carcinoma in the oral cavity or oropharynx during the first year after completion of their curative treatment, routine surveillance for detecting early locoregional recurrence, distant metastases, and second metachronous primary tumors is very important[13,14]. Due to the poor prognosis of head and neck cancer, the data of metachronous cancer of UGI tract were limited. In this study, 3 patients had 4 primary metachronous tumors. The interval from first tumor to second tumor ranged from 5 to 10 years.
In the majority of follow-up protocols, radiologic and endoscopic evaluation has been proven to be useful in the early detection of metachronous and recurrent neoplasms in the follow-up of patients with previously treated carcinomas of the ear, nose, and throat. Adequate staging of UGI cancer including CT and endoscopic ultrasonography has been considered to be helpful for avoiding useless surgery[15,16]. However, more than 30% of the distant metastases have been reported to be radiographically occult with conventional diagnostic strategy and surgery. It has been still performed in a considerable number of patients with distant metastases. Moreover, the overall survival after curative resection does not exceed 25%, with an overall median disease-free survival of only 12 mo.
Conventional staging methods consisting of both CT and EUS evaluate local unresectability or metastatic diseases based on the anatomic alterations. Their low sensitivity and low specificity were related to the low accuracy in determining a curative surgery, indicating the demand for a different approach[17,18]. In contrast to conventional anatomic imaging, PET can reveal metabolic alterations in tumor tissues. Most malignant tumors present a high uptake of 18F-FDG due to an increased anaerobic glycolysis[19]. In our previous studies, 18F-FDG PET/CT was found to be valuable in detecting previously unknown metastases in esophageal cancer. Routinely performed 18F-FDG PET/CT in the preoperative work-up of these tumors may therefore reduce the number of unnecessary surgical procedures[20].
There have been several investigations into the utility of 18F-FDG PET or PET/CT in relation to multiple primary cancers detection. Major advantages of the whole body 18F-FDG PET/CT are the capability to perform full-body scan with the potential to detect local and distant metastases in one single examination and the possibility of distinguishing new active disease from scar or necrotic tissues[21,22] since tumors with increased 18F-FDG uptake are more metabolically active and biologically aggressive[23,24].
The accurate staging of multiple primary cancer of UGI tract is essential to select appropriate treatment and to anticipate disease progression. Conventional imaging methods that rely on detection of the structural changes caused by tumors usually have limitations in determining the extent of UGI, especially lymph node metastasis[25,26]. PET/CT is a fundamentally different imaging technique that identifies focal areas of increased metabolism associated with malignancies. PET/CT is more sensitive than regular CT scan in determining regional and distant lymph node involvement in the squamous cell carcinoma as well as adenocarcinoma of the esophagus. PET can play an important role in evaluating the pretreatment staging of esophageal cancer[27,28]. A noteworthy finding in the present study is the high incidence of 100% (13/13) of local lymph node metastases and distant metastases detected by 18F-FDG PET/CT. Furthermore, clinical decisions of treatment were changed in 11 patients after PET/CT examinations.
There are several limitations in this study. First, due to the retrospective feature of the study, we did not get all of the medical details for some of the patients. There are also some disadvantages associated with PET/CT imaging. For example, small tumors might be undetected because partial-volume effects result in a falsely low measurement of true 18F-FDG activity[29]. Another drawback of PET/CT is that 18F-FDG frequently accumulates in areas of inflammation. Variable physiologic FDG uptake patterns and benign pathological causes of 18F-FDG uptake can be specifically recognized and properly categorized in other instances[30].
The choice of diagnostic techniques must be based on the site and histologic characteristics of the synchronous tumors. Although 18F-FDG PET/CT may be the preferred technique for staging UGI cancer, it can not replace other techniques, such as Lugol chromoendoscopy, for detecting synchronous UGI cancer in high-risk populations[31].
Our results suggested that 18F-FDG PET/CT may be useful in evaluating the multiple primary malignant tumors of UGI cancer. It may play an important role in the initial staging of multiple synchronous or metachronous UGI tract cancers.
Multiple primary malignancies in a single patient are relatively rare but have increased in frequency in recent decades. Metachronous or synchronous esophageal cancer has been identified in patients with head and neck cancer, gastric cancer or colon cancer. Alcohol drinking and tobacco smoking are the major risk factors for upper aerodigestive tract cancers, accounting for a large proportion of cases in developed countries. The occurrence of multiple primary cancers in the aerodigestive tract also has been explained by the concept of field carcinogenesis. Combined exposure to alcohol and tobacco has a multiplicative effect on carcinogenesis of upper aerodigestive tract.
Positron emission tomography/computed tomography (PET/CT) provides anatomic landmarks for better characterization of increased 18F-fluorodeoxyglucose (18F-FDG) uptake. PET/CT is a widely accepted imaging method in the management of a wide variety of cancers. The reported increase in sensitivity of PET/CT over conventional techniques has been attributed to the ability of PET/CT to detect metabolic abnormalities that precede the morphologic changes seen by CT. However, the usefulness and limitations of 18F-FDG PET/CT in evaluating multiple primary malignant tumors of upper gastrointestinal tract still need further clinical evaluations.
The early detection of multiple primary malignant tumors of upper gastrointestinal (UGI) cancer will enable prompt management and will increase the cure rate of the disease. Whole body 18F-FDG PET/CT scan could provide valuable information for early detection and might guide salvage treatment for multiple primary malignant tumors of UGI cancer.
18F-FDG PET/CT may be useful in evaluating the multiple primary malignant tumors of UGI cancer. It may play an important role in the initial staging of multiple synchronous or metachronous UGI tract cancers.
The manuscript is very well written and should be accepted for publication.
Peer reviewer: Dr. Andrea Hille, Department of Radiotherapy and Radio-oncology, University of Goettingen, School of Medicine, Robert-Koch-Str. 40, Goettingen, D-37085, Germany
S- Editor Wang YR L- Editor Ma JY E- Editor Ma WH
| 1. | Lo OS, Law S, Wei WI, Ng WM, Wong KH, Tong KH, Wong J. Esophageal cancers with synchronous or antecedent head and neck cancers: a more formidable challenge? Ann Surg Oncol. 2008;15:1750-1756. |
| 2. | Pelucchi C, Gallus S, Garavello W, Bosetti C, La Vecchia C. Alcohol and tobacco use, and cancer risk for upper aerodigestive tract and liver. Eur J Cancer Prev. 2008;17:340-344. |
| 3. | Bosetti C, Gallus S, Peto R, Negri E, Talamini R, Tavani A, Franceschi S, La Vecchia C. Tobacco smoking, smoking cessation, and cumulative risk of upper aerodigestive tract cancers. Am J Epidemiol. 2008;167:468-473. |
| 4. | Thomson PJ. Field change and oral cancer: new evidence for widespread carcinogenesis? Int J Oral Maxillofac Surg. 2002;31:262-266. |
| 5. | Sapkota A, Hsu CC, Zaridze D, Shangina O, Szeszenia-Dabrowska N, Mates D, Fabiánová E, Rudnai P, Janout V, Holcatova I. Dietary risk factors for squamous cell carcinoma of the upper aerodigestive tract in central and eastern Europe. Cancer Causes Control. 2008;19:1161-1170. |
| 6. | Nawaz M, Jehanzaib M, Khan K, Zari M. Role of barium meal examination in diagnosis of peptic ulcer. J Ayub Med Coll Abbottabad. 2008;20:59-61. |
| 7. | Kim HJ, Kim AY, Lee JH, Yook JH, Yu ES, Ha HK. Positioning during CT gastrography in patients with gastric cancer: the effect on gastric distension and lesion conspicuity. Korean J Radiol. 2009;10:252-259. |
| 8. | Kohmura T, Hasegawa Y, Ogawa T, Matsuura H, Takahashi M, Yanagita N, Nakashima T. Cyclin D1 and p53 overexpression predicts multiple primary malignant neoplasms of the hypopharynx and esophagus. Arch Otolaryngol Head Neck Surg. 1999;125:1351-1354. |
| 9. | Kumagai Y, Kawano T, Nakajima Y, Nagai K, Inoue H, Nara S, Iwai T. Multiple primary cancers associated with esophageal carcinoma. Surg Today. 2001;31:872-876. |
| 10. | Chung KY, Mukhopadhyay T, Kim J, Casson A, Ro JY, Goepfert H, Hong WK, Roth JA. Discordant p53 gene mutations in primary head and neck cancers and corresponding second primary cancers of the upper aerodigestive tract. Cancer Res. 1993;53:1676-1683. |
| 11. | Hashibe M, Brennan P, Benhamou S, Castellsague X, Chen C, Curado MP, Dal Maso L, Daudt AW, Fabianova E, Fernandez L. Alcohol drinking in never users of tobacco, cigarette smoking in never drinkers, and the risk of head and neck cancer: pooled analysis in the International Head and Neck Cancer Epidemiology Consortium. J Natl Cancer Inst. 2007;99:777-789. |
| 12. | Yokoyama A, Omori T, Yokoyama T, Sato Y, Kawakubo H, Maruyama K. Risk of metachronous squamous cell carcinoma in the upper aerodigestive tract of Japanese alcoholic men with esophageal squamous cell carcinoma: a long-term endoscopic follow-up study. Cancer Sci. 2008;99:1164-1171. |
| 13. | Krabbe CA, Pruim J, Dijkstra PU, Balink H, van der Laan BF, de Visscher JG, Roodenburg JL. 18F-FDG PET as a routine posttreatment surveillance tool in oral and oropharyngeal squamous cell carcinoma: a prospective study. J Nucl Med. 2009;50:1940-1947. |
| 14. | Abgral R, Querellou S, Potard G, Le Roux PY, Le Duc-Pennec A, Marianovski R, Pradier O, Bizais Y, Kraeber-Bodéré F, Salaun PY. Does 18F-FDG PET/CT improve the detection of posttreatment recurrence of head and neck squamous cell carcinoma in patients negative for disease on clinical follow-up? J Nucl Med. 2009;50:24-29. |
| 15. | Petit T, Georges C, Jung GM, Borel C, Bronner G, Flesch H, Massard G, Velten M, Haegele P, Schraub S. Systematic esophageal endoscopy screening in patients previously treated for head and neck squamous-cell carcinoma. Ann Oncol. 2001;12:643-646. |
| 16. | Leoni-Parvex S, Mihaescu A, Pellanda A, Monnier P, Bosman FT. Esophageal cytology in the follow-up of patients with treated upper aerodigestive tract malignancies. Cancer. 2000;90:10-16. |
| 17. | Choi J, Kim SG, Kim JS, Jung HC, Song IS. Comparison of endoscopic ultrasonography (EUS), positron emission tomography (PET), and computed tomography (CT) in the preoperative locoregional staging of resectable esophageal cancer. Surg Endosc. 2010;24:1380-1386. |
| 18. | Sandha GS, Severin D, Postema E, McEwan A, Stewart K. Is positron emission tomography useful in locoregional staging of esophageal cancer? Results of a multidisciplinary initiative comparing CT, positron emission tomography, and EUS. Gastrointest Endosc. 2008;67:402-409. |
| 20. | Sun L, Su XH, Guan YS, Pan WM, Luo ZM, Wei JH, Zhao L, Wu H. Clinical usefulness of 18F-FDG PET/CT in the restaging of esophageal cancer after surgical resection and radiotherapy. World J Gastroenterol. 2009;15:1836-1842. |
| 21. | Bockisch A, Freudenberg LS, Schmidt D, Kuwert T. Hybrid imaging by SPECT/CT and PET/CT: proven outcomes in cancer imaging. Semin Nucl Med. 2009;39:276-289. |
| 22. | Even-Sapir E, Keidar Z, Bar-Shalom R. Hybrid imaging (SPECT/CT and PET/CT)--improving the diagnostic accuracy of functional/metabolic and anatomic imaging. Semin Nucl Med. 2009;39:264-275. |
| 23. | Jadvar H, Alavi A, Gambhir SS. 18F-FDG uptake in lung, breast, and colon cancers: molecular biology correlates and disease characterization. J Nucl Med. 2009;50:1820-1827. |
| 24. | Gerbaudo VH, Britz-Cunningham S, Sugarbaker DJ, Treves ST. Metabolic significance of the pattern, intensity and kinetics of 18F-FDG uptake in malignant pleural mesothelioma. Thorax. 2003;58:1077-1082. |
| 25. | Kresnik E, Mikosch P, Gallowitsch HJ, Kogler D, Wiesser S, Heinisch M, Unterweger O, Raunik W, Kumnig G, Gomez I. Evaluation of head and neck cancer with 18F-FDG PET: a comparison with conventional methods. Eur J Nucl Med. 2001;28:816-821. |
| 26. | Krabbe CA, Pruim J, van der Laan BF, Rödiger LA, Roodenburg JL. FDG-PET and detection of distant metastases and simultaneous tumors in head and neck squamous cell carcinoma: a comparison with chest radiography and chest CT. Oral Oncol. 2009;45:234-240. |
| 27. | Roh JL, Yeo NK, Kim JS, Lee JH, Cho KJ, Choi SH, Nam SY, Kim SY. Utility of 2-[18F] fluoro-2-deoxy-D-glucose positron emission tomography and positron emission tomography/computed tomography imaging in the preoperative staging of head and neck squamous cell carcinoma. Oral Oncol. 2007;43:887-893. |
| 28. | Schwartz DL, Ford E, Rajendran J, Yueh B, Coltrera MD, Virgin J, Anzai Y, Haynor D, Lewellyn B, Mattes D. FDG-PET/CT imaging for preradiotherapy staging of head-and-neck squamous cell carcinoma. Int J Radiat Oncol Biol Phys. 2005;61:129-136. |
| 29. | Shammas A, Lim R, Charron M. Pediatric FDG PET/CT: physiologic uptake, normal variants, and benign conditions. Radiographics. 2009;29:1467-1486. |
| 30. | Costelloe CM, Murphy WA Jr, Chasen BA. Musculoskeletal pitfalls in 18F-FDG PET/CT: pictorial review. AJR Am J Roentgenol. 2009;193:WS1-WS13, Quiz S26-S30. |
| 31. | Piazza C, Dessouky O, Peretti G, Cocco D, De Benedetto L, Nicolai P. Narrow-band imaging: a new tool for evaluation of head and neck squamous cell carcinomas. Review of the literature. Acta Otorhinolaryngol Ital. 2008;28:49-54. |