Published online Jan 21, 2010. doi: 10.3748/wjg.v16.i3.345
Revised: October 26, 2009
Accepted: November 1, 2009
Published online: January 21, 2010
AIM: To re-evaluate the theory that colonic diverticulosis is associated with relapse of Clostridium difficile associated disease (CDAD) in light of data suggesting increasing rates of CDAD infection and relapse.
METHODS: Charts were reviewed for patients with recurrent CDAD who had also had a prior colonoscopy or flexible sigmoidoscopy. An age and gender matched control group was used to compare the prevalence of diverticulosis.
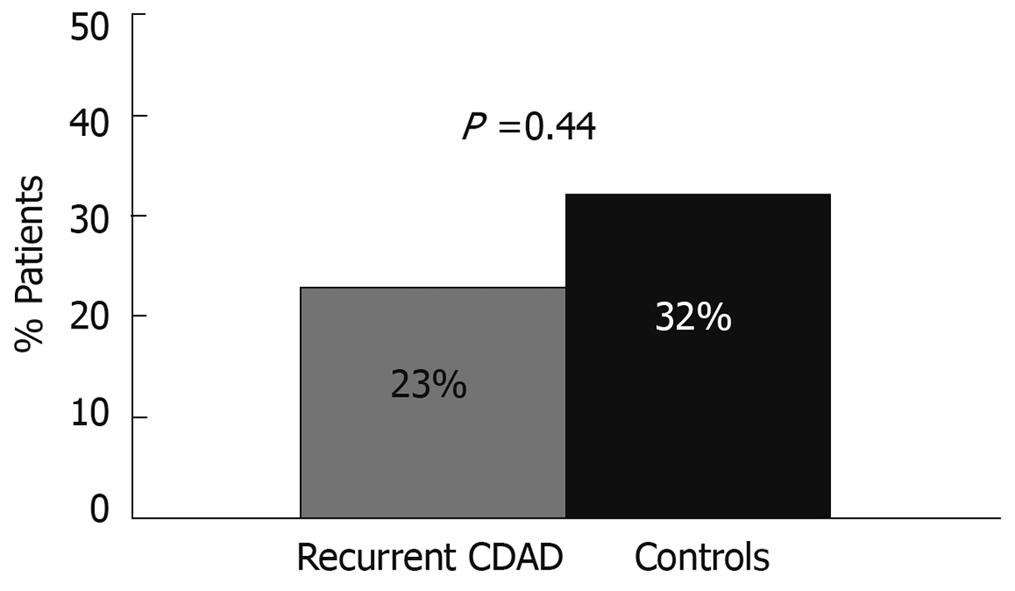
RESULTS: Twenty-two patients met the study criteria, and the prevalence of diverticulosis in patients with CDAD relapse was 23% compared to 32% in age and sex matched controls (P = 0.44). A significant proportion of patients with CDAD relapse had co-morbidities associated with immune suppression.
CONCLUSION: Diverticulosis does not appear to be associated with CDAD relapse.
-
Citation: Lipp MJ, Pagovich OE, Rabin D, Min AD, Bernstein BB. Prevalence of diverticulosis in recurrent
Clostridium difficile infection. World J Gastroenterol 2010; 16(3): 345-347 - URL: https://www.wjgnet.com/1007-9327/full/v16/i3/345.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i3.345
The incidence of Clostridium difficile (C. difficile) associated disease (CDAD) has reached epidemic proportions, increasing both in terms of frequency and severity. The rates of C. difficile associated disease have steadily increased since the 1980s, with a marked increase in infection over the past 10 years. In one region of Canada there was a four-fold increase from 2002 to 2003 alone[1]. The cost associated with CDAD in 2008 in the U.S. has been estimated at $32 million per day with nearly 40 000 extra hospital inpatient days due to C. difficile infection[2].The increased incidence and virulence of C. difficile infection are felt to be caused by a new hypervirulent strain which produces significantly more toxins A and B. In addition to increasing morbidity and mortality, this hypervirulent strain has also led to an increase in relapse rates, which have been reported to be as high as 47.2%[3], compared to historic relapse rates of approximately 20%[4].
The exact etiology of CDAD relapse is incompletely understood, but it is probably multifactorial. Relapse of CDAD is usually caused by the original strain, although a percentage of patients are infected with a new strain[5]. One of the earliest theories for CDAD relapse was the presence of colonic diverticula, which were thought to serve as reservoirs for C. difficile spores. This was largely based on an early study by Tedesco et al[6] which found that 18 of 22 patients (82%) with recurrent C. difficile infection had diverticulosis. It was theorized that C. difficile spores in diverticula were impervious to antibiotics and so could germinate after the completion of treatment. Tapered and pulsed antibiotic regimens for recurrent C. difficile infection were thus aimed at treating these dormant spores[7]. To our knowledge no paper has re-evaluated the association between diverticulosis and C. difficile relapse. Our study aimed to re-evaluate the association between diverticulosis and recurrent C. difficile infection at our medical center in light of increasing rates of CDAD infection and relapse.
We reviewed positive ELISA-based C. difficile toxin assays from 2005-2007 at our tertiary level hospital. We reviewed the charts of patients with a minimum of two positive toxin assays more than 14 d apart who also had a prior colonoscopy or flexible sigmoidoscopy at our institution. Patient charts were reviewed for the presence of diverticulosis, prior antibiotic use, comorbidities, recent hospitalizations, C. difficile treatment course, and number of relapses.
Relapse was defined as recurrent diarrhea with a positive toxin assay or pseudomembranous colitis after completion of treatment for C. difficile infection within the previous 3 mo. To be included in the study, patients must have completed full initial antibiotic therapy for a minimum of 10 d with symptomatic improvement. An age and gender matched control group was used to compare the prevalence of diverticulosis at our institution. Patients in the control group had colonoscopies performed for the purpose of colorectal cancer screening. This study was approved by our medical center’s institutional review board.
Twenty-two patients met the study criteria, with an average of 2.3 episodes of C. difficile infection. All patients were treated with standard metronidazole (po or iv) and/or oral vancomycin therapy. The prevalence of diverticulosis in patients with C. difficile relapse was 23%, with a mean patient age of 62. The prevalence of diverticulosis in the age and sex matched control group was 32% (P = 0.44, using χ2 analysis, Figure 1). Table 1 shows the baseline characteristics of patients with recurrent C. difficile relapse. The inpatient mortality in this group was 18%.
| Baseline characteristics | |
| Mean age (yr) | 62 (30-90) |
| Female | 13 (59%) |
| Recent hospitalizations( < 3 mo) | 18 (82%) |
| Lymphoma/malignancy | 8 (36%) |
| HIV/AIDS | 3 (14%) |
| Systemic steroid use | 3 (14%) |
| Liver cirrhosis | 2 (9%) |
Patients with recurrent C. difficile infection at our institution did not have a higher prevalence of colonic diverticulosis than age and sex matched controls. The prevalence of diverticulosis in patients with relapsing C. difficile and controls was 23% and 32%, respectively (P = 0.44), which is consistent with historical controls. To our knowledge this is the first paper to reevaluate the association between diverticulosis and recurrent C. difficile infection since first described by Tedesco et al[6].
We found that a high percentage of patients with recurrent C. difficile infection suffered from co-morbidities often associated with immune suppression. These results are not surprising since growing data suggest that host immunity plays a large role in promoting relapse[8-14]. One of the earliest studies to support this theory came from Kyne et al[15] where 22 patients with resolved C. difficile infection were compared to 22 patients with relapsing disease. Patients with relapsing C. difficile infection were found to have significantly lower levels of serum antibodies to toxin A. Additional independent risk factors for C. difficile recurrence include older age[16] and prolonged hospitalization[17].
Patients with impaired host immunity during chemotherapy have been found to have higher rates of CDAD[8], even without prior antibiotic use[9]. Higher rates of CDAD infection have been found in patients on nephrology, hematology, and organ transplantation wards[10], as well as in patients with human immunodeficiency virus (HIV) infection[11]. These findings have prompted research aimed at improving host immunity in patients with CDAD relapse. Intravenous immunoglobulin (IVIG) has been used in the treatment of severe, refractory, or recurrent C. difficile infection[12,16]. A human monoclonal antibody against toxins A and B, MDX-1388, was shown to have efficacy in preventing relapse of C. difficile infection in hamsters[13]. A small study of a toxoid vaccine against C. difficile showed benefit in 3 patients with recurrent C. difficile, allowing the cessation of antibiotic treatment[14].
Our study had several limitations. Given the small patient size our study may have been underpowered to detect a difference in the prevalence of diverticulosis. This study was also done retrospectively and all patients originated from a single institution. Our results did not find an association between colonic diverticulosis and recurrent C. difficile infection at our institution, however further studies may be needed to verify these findings. The high prevalence of co-morbidities often associated with immune suppression in patients with recurrent C. difficile, however, is consistent with current data that suggest host immunity may play a significant role in CDAD relapse.
The incidence of Clostridium difficile (C. difficile) associated disease (CDAD) has reached epidemic proportions, increasing both in terms of frequency and severity. The exact etiology of CDAD relapse is incompletely understood, and previous research has suggested an association between CDAD relapse and colonic diverticulosis.
The increased incidence and virulence of C. difficile infection are felt to be caused by a new hypervirulent strain which produces significantly more toxins A and B. In addition to increasing morbidity and mortality, this hypervirulent strain has also led to an increase in relapse rates. In this study the authors did not find an association between colonic diverticulosis and CDAD relapse, but did find that a significant proportion of patients with CDAD relapse had co-morbidities associated with immune suppression.
Recent reports have suggested that host immunity may play a role in preventing future C. difficile relapse. This is the first paper to re-evaluate the association between CDAD relapse and colonic diverticulosis since the emergence of a new hypervirulent strain.
By showing a lack of association between colonic diverticulosis and CDAD relapse, this study could help guide future treatments. Previous treatments were originally aimed at treating dormant spores in diverticula with pulsed or tapering antibiotics. This study would suggest that therapy aimed at improving host immunity may be important in CDAD relapse.
C. difficile is a gram positive bacterium that may cause a colonic infection, typically after antibiotic use. This infection may become severe and may relapse, requiring multiple antibiotic treatments. Colonic diverticula are outpouchings of the colonic wall.
It is an interesting study that addresses a potentially important relationship between recurrence of C. difficile infection and diverticulosis.
Peer reviewer: Dr. Lodewijk Adriaan Anton Brosens, MD, PhD, Department of Pathology, University Medical Center Utrecht, Postbus 85500, 3508 GA Utrecht, The Netherlands
S- Editor Wang YR L- Editor O'Neill M E- Editor Tian L
| 1. | Pépin J, Valiquette L, Alary ME, Villemure P, Pelletier A, Forget K, Pépin K, Chouinard D. Clostridium difficile-associated diarrhea in a region of Quebec from 1991 to 2003: a changing pattern of disease severity. CMAJ. 2004;171:466-472. |
| 2. | APIC executive Summary National Prevalence Study of Clostridium difficile in U. S. Healthcare Facilities. Pages 1-5, Accessed: June 2 2009; Available from: http://www.apic.org/AM/CM/ContentDisplay.cfmContentFileID=11410. |
| 3. | Pepin J, Alary ME, Valiquette L, Raiche E, Ruel J, Fulop K, Godin D, Bourassa C. Increasing risk of relapse after treatment of Clostridium difficile colitis in Quebec, Canada. Clin Infect Dis. 2005;40:1591-1597. |
| 4. | Surawicz CM. Reining in recurrent Clostridium difficile infection--who's at risk. Gastroenterology. 2009;136:1152-1154. |
| 5. | Johnson S, Adelmann A, Clabots CR, Peterson LR, Gerding DN. Recurrences of Clostridium difficile diarrhea not caused by the original infecting organism. J Infect Dis. 1989;159:340-343. |
| 6. | Tedesco FJ, Gordon D, Fortson WC. Approach to patients with multiple relapses of antibiotic-associated pseudomembranous colitis. Am J Gastroenterol. 1985;80:867-868. |
| 7. | McFarland LV, Elmer GW, Surawicz CM. Breaking the cycle: treatment strategies for 163 cases of recurrent Clostridium difficile disease. Am J Gastroenterol. 2002;97:1769-1775. |
| 8. | Blot E, Escande MC, Besson D, Barbut F, Granpeix C, Asselain B, Falcou MC, Pouillart P. Outbreak of Clostridium difficile-related diarrhoea in an adult oncology unit: risk factors and microbiological characteristics. J Hosp Infect. 2003;53:187-192. |
| 9. | Anand A, Glatt AE. Clostridium difficile infection associated with antineoplastic chemotherapy: a review. Clin Infect Dis. 1993;17:109-113. |
| 10. | Svenungsson B, Burman LG, Jalakas-Pörnull K, Lagergren A, Struwe J, Akerlund T. Epidemiology and molecular characterization of Clostridium difficile strains from patients with diarrhea: low disease incidence and evidence of limited cross-infection in a Swedish teaching hospital. J Clin Microbiol. 2003;41:4031-4037. |
| 11. | Sanchez TH, Brooks JT, Sullivan PS, Juhasz M, Mintz E, Dworkin MS, Jones JL. Bacterial diarrhea in persons with HIV infection, United States, 1992-2002. Clin Infect Dis. 2005;41:1621-1627. |
| 12. | McPherson S, Rees CJ, Ellis R, Soo S, Panter SJ. Intravenous immunoglobulin for the treatment of severe, refractory, and recurrent Clostridium difficile diarrhea. Dis Colon Rectum. 2006;49:640-645. |
| 13. | Babcock GJ, Broering TJ, Hernandez HJ, Mandell RB, Donahue K, Boatright N, Stack AM, Lowy I, Graziano R, Molrine D. Human monoclonal antibodies directed against toxins A and B prevent Clostridium difficile-induced mortality in hamsters. Infect Immun. 2006;74:6339-6347. |
| 14. | Sougioultzis S, Kyne L, Drudy D, Keates S, Maroo S, Pothoulakis C, Giannasca PJ, Lee CK, Warny M, Monath TP. Clostridium difficile toxoid vaccine in recurrent C. difficile-associated diarrhea. Gastroenterology. 2005;128:764-770. |
| 15. | Kyne L, Warny M, Qamar A, Kelly C. Association between antibody response to toxin A and protection against recurrent diarrhoea. Lancet. 2001;357:189-193. |
| 16. | McFarland LV, Surawicz CM, Rubin M, Fekety R, Elmer GW, Greenberg RN. Recurrent Clostridium difficile disease: epidemiology and clinical characteristics. Infect Control Hosp Epidemiol. 1999;20:43-50. |
| 17. | Pépin J, Routhier S, Gagnon S, Brazeau I. Management and outcomes of a first recurrence of Clostridium difficile-associated disease in Quebec, Canada. Clin Infect Dis. 2006;42:758-764. |