Published online May 21, 2010. doi: 10.3748/wjg.v16.i19.2443
Revised: February 14, 2010
Accepted: February 21, 2010
Published online: May 21, 2010
Filiform polyposis is a rare condition of uncertain pathogenesis that is usually found in association with Crohn’s disease, ulcerative colitis, intestinal tuberculosis or histiocytosis X. We report seven interesting cases of polyposis with various pathologic components, mainly located in the left side of the colon with no associated inflammatory bowel disease, intestinal tuberculosis or histiocytosis X. Multiple finger-like polypoid lesions with the appearance of stalactites were noted on the left side of the colon, especially in the sigmoid area, at the time of colonoscopy. The polyps had a variety of sizes and shapes and were shown to have various histopathologic components among the different patients. Although filiform polyposis localized in the sigmoid colon appears not to have high oncogenic potential, periodic follow-up seems to be needed.
- Citation: Lee CG, Lim YJ, Choi JS, Lee JH. Filiform polyposis in the sigmoid colon: A case series. World J Gastroenterol 2010; 16(19): 2443-2447
- URL: https://www.wjgnet.com/1007-9327/full/v16/i19/2443.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i19.2443
Filiform polyposis is a rare form of pseudopolyposis associated with ulcerative colitis, Crohn’s disease, or granulomatous disease, which is formed by non-specific mucosal and submucosal reactions to previous severe inflammation[1-5]. The transverse and descending colon are the most common locations, although the polyps can be seen in any portion of the large bowel[3-6]. However, reports regarding filiform polyposis confined to the sigmoid colon, and the natural history or management of incidentally detected filiform polyposis in patients without the definite history of ulcerative colitis, Crohn’s disease, or intestinal tuberculosis are inadequate[7,8].
We report seven interesting cases of filiform polyposis with mixed histologic components, including mainly inflammatory and hyperplastic or adenomatous components, located in the sigmoid area, without a definite history of severe inflammation such as inflammatory bowel disease (IBD) or intestinal tuberculosis.
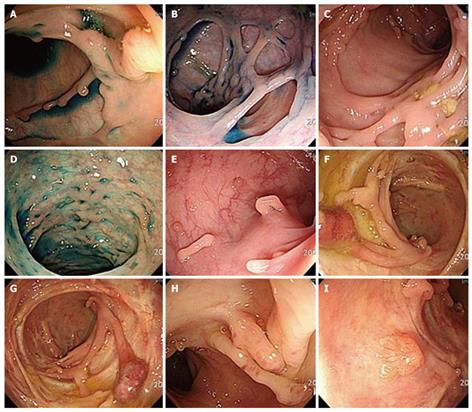
A 38-year-old male patient had sudden onset abdominal pain, diarrhea, and hematochezia for 2 d and had been diagnosed as having infectious colitis. He did not have a medical history of tuberculosis, IBD, or infectious colitis. Colonoscopic examination showed multiple, variable-sized polyps that were found in the sigmoid colon (Figure 1A). These polyps were histopathologically proven to be inflammatory and hyperplastic. Up to 44 mo later, there was no evidence of malignant change in the polyposis on follow-up colonoscopy examination.
A 64-year-old healthy male patient had no medical history of IBD or lower gastrointestinal symptoms. Colonoscopy was performed for screening purposes. On the colonoscopic examination, multiple long worm-like polyps were noted at the sigmoid colon (Figure 1B). These growths were histopathologically proven to be inflammatory polyps. Two large polyps were also found in the ascending colon and snare polypectomy was performed. These polyps were adenomas by pathologic evaluation.
On the follow-up colonoscopic examination 6 mo later, multiple finger-like polypoid lesions with the appearance of stalactites persisted on the left side of the colon, especially in the sigmoid area (Figure 1C). Large polyps with a hyperemic mucosa were removed by snare. These polyps were hyperplastic, tubular adenomas and filiform polyps with lymphoid hyperplasia. Up to 43 mo later, there was no evidence of malignant change in the polyposis on follow-up colonoscopy examination.
A 37-year-old male patient had frequent intermittent diarrhea after abdominal pain and was diagnosed as having irritable bowel syndrome. Colonoscopy was performed and multiple polyps were seen, which were densely packed, forming a roof in the sigmoid colon (Figure 1D). A representative polyp was removed by snare and shown to be a filiform or hyperplastic polyp on pathologic assessment. Up to 46 mo later, there was no evidence of malignant change in the polyposis on follow-up colonoscopy examination.
A 67-year-old asymptomatic male patient stated that colonofiberscopy had been performed at another hospital 2 years previously and the colonoscopic findings were lesions suspicious for intestinal tuberculosis. Colonofiberscopy was conducted again and multiple polypoid lesions with variable shape and size were found at the sigmoid colon (Figure 1E). To establish the exact pathologic diagnosis, snare polypectomy was performed. The pathologic results revealed that the polyps were mainly filiform and hyperplastic. Up to 46 mo later, there was no evidence of malignant change in the polyposis on follow-up colonoscopy examination.
A 77-year-old male patient generally had no lower gastrointestinal symptoms. The colonoscopic findings showed multiple polyps forming a densely packed bridge in the sigmoid colon (Figure 1F). These polyps were pathologically diagnosed as being mainly filiform and hyperplastic. Up to 34 mo later, there was no evidence of malignant change in the polyposis on follow-up colonoscopy examination.
An 81-year-old female patient was referred to our hospital for evaluation of sigmoid polyposis. Colonoscopy was performed and worm-like polyps located in the sigmoid colon were shown (Figure 1G). In addition, one polyp was reported as chronic non-specific inflammation with crypt cell hyperplasia and another was a hyperplastic polyp with focal atypical glands, favoring a reactive hyperplasia. Up to 38 mo later, there was no evidence of malignant change in the polyposis on follow-up colonoscopy examination.
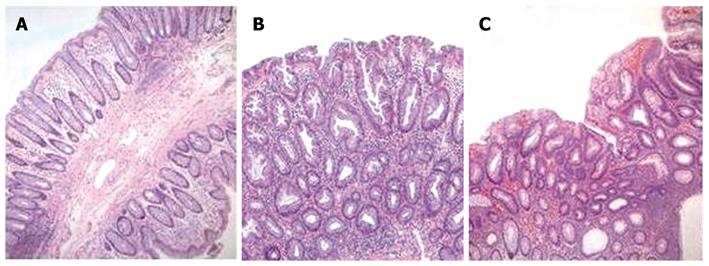
A 63-year-old female had a history of diarrhea, abdominal pain, and weight loss for several months. The patient was referred to our hospital for further evaluation of multiple colon polyps. On colonoscopy, multiple variable polyps were noted in the cecum, ascending colon, and mainly in the sigmoid colon. Multiple finger- or worm-like polypoid lesions were noted in the sigmoid colon (Figure 1H and I). The polyps were of various size and shape. The tips of the polyps adhered to other parts of the mucosa, forming loops or bridges between opposing walls. Large polyps were removed by snare. All these polyps, except one, were shown to be hyperplastic or filiform (inflammatory) based on pathologic evaluation (Figure 2A and B). Only one polyp was shown to be a villous adenoma (Figure 2C). Up to 36 mo later, there was no evidence of malignant change in the polyposis on follow-up colonoscopy examination. We recommended periodic colonoscopy for cancer surveillance.
We report here seven cases of previously undiscovered polyposis in the sigmoid colon without a definite history of severe chronic inflammation including IBD or intestinal tuberculosis. This report is intended to characterize the clinical and pathologic features of filiform polyposis mainly located in the sigmoid colon. The clinicopathologic characteristics of filiform polyposis in the sigmoid colon of all the seven cases are shown in Table 1.
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | |
| Age (yr) | 38 | 64 | 37 | 67 | 77 | 81 | 63 |
| Sex | M | M | M | M | M | F | F |
| Location | Sigmoid colon | Sigmoid colon | Sigmoid colon | Sigmoid colon | Sigmoid colon | Sigmoid colon | Sigmoid colon |
| Tuberculosis history | None | None | None | None | None | None | None |
| IBD | None | None | None | None | None | None | None |
| Chest PA | None | Normal | Normal | Normal | Normal | Normal | Normal |
| Pinch biopsy pathologic findings | Inflammatory | Inflammatory | Hyperplastic | Inflammatory | Inflammatory | Inflammatory | Inflammatory |
| Hyperplastic | Hyperplastic | ||||||
| Tubular adenoma | Hyperplastic | Hyperplastic | Hyperplastic | Hyperplastic | |||
| Polypectomy pathologic findings | Filiform | Filiform | Filiform | Filiform | Filiform | Filiform | Filiform |
| Hyperplastic | |||||||
| Hyperplastic | Villotubular adenoma | Hyperplastic | Hyperplastic | Hyperplastic | Hyperplastic | Villous adenoma | |
| Diarrhea | Yes | None | Yes | None | None | Yes | Yes |
| Hematochezia | Yes | None | None | None | None | None | Yes |
| Abdominal pain | Yes | None | Yes | None | None | Yes | Yes |
| Weight loss | None | None | None | None | None | Yes | Yes |
| Follow-up period (mo) | 44 | 43 | 46 | 46 | 34 | 38 | 36 |
Filiform polyposis is an uncommon entity that is most often encountered in the colon of patients with a history of IBD[2]. Filiform polyposis is characterized by a large number of worm-like polyps lined by histologically normal colonic mucosa[5,8]. Filiform polyps usually have a thin, straight shape resembling the stalks of polyps without the heads[4]. The polyps can range in size from 1.5-3.0 cm in length and up to 0.5 cm in diameter[2,3]. The projections can occur as solitary polyps or as diffuse polyposis distributed over large areas of the colonic mucosa[8]. Long-term inflammation of the colonic mucosa during chronic IBD with alternating periods of ulceration and healing may lead to the formation of finger-like projections, these so-called filiform polyps[2-4]. Only rare cases without a history or evidence of IBD have been reported[3]. Additionally, in rare cases, several filiform polyps form large tumor masses, termed giant filiform polyposis[5]. Histologically, the polyps are filiform, with a central core, containing vessels and smooth muscle fibers[6]. Clinicopathologic and immunophenotypic studies regarding filiform polyposis without IBD demonstrate that there is generalized polyposis, generally considered to be an asymptomatic sequela of ulcerative colitis[2]. Generally, there is no definite evidence that filiform polyposis itself represents a pre-cancerous condition[2]. Filiform polyposis may resemble villous adenomas on colonoscopy[4]. Therefore, biopsy should be recommended in all cases of filiform polyposis if it is necessary[3,8,9]. Filiform polyposis alone is not an indication for surgical resection, but complications, such as acute massive hemorrhage or intestinal obstruction, may necessitate surgical intervention[10,11].
In our case series it cannot be completely excluded that filiform polyps may have emerged as asymptomatic sequelae of intestinal tuberculosis, IBD, other infectious colitis, ischemic colitis, or histiocytosis X.
Sporadic hyperplastic polyps are generally thought to be non-malignant and malignant transformation into adenocarcinoma has been rarely reported[12]. However, contrary to single sporadic hyperplastic polyps, hyperplastic polyposis is considered to be a pre-cancerous lesion[12-17]. Our case series is distinct from hyperplastic polyposis syndrome. The diagnostic criteria for hyperplastic polyposis generally include the presence of (1) at least 5 histologically diagnosed hyperplastic polyps proximal to the sigmoid colon, of which two are > 10 mm in diameter, or (2) any number of hyperplastic polyps proximal to the sigmoid colon in an individual who has a first degree relative with hyperplastic polyposis, or (3) > 30 hyperplastic polyps of any size that are distributed throughout the colon[12-15]. Our case series did not satisfy these diagnostic criteria.
Diffuse colonic mucosal ulceration is a possible finding in histiocytosis X[18]. Histiocytosis X may have gastrointestinal symptoms such as diarrhea, malabsorption, or gastrointestinal bleeding[18]. However, these gastrointestinal symptoms are rare[18]. Diagnosis of histiocytosis X is based on mucosal biopsy and immunopathologic findings which demonstrate the presence of a disseminated proliferation of histiocytes[18]. Our case series did not satisfy this pathologic finding.
We report seven patients with filiform polyposis mainly localized in the sigmoid colon. Although none of our cases showed progression into adenocarcinoma, various pathologic findings, including mainly filiform polyps, hyperplastic polyps or adenomas, were found. None of the patients had a definite history of IBD, intestinal tuberculosis, infectious or ischemic colitis, but the filiform polyposis seemed to be a sequela of asymptomatic chronic colonic inflammation. Although definite evidence is insufficient, filiform polyposis localized in the sigmoid colon appears not to have high oncogenic potential. However, periodic follow-up seems to be necessary because large polyps were intermittently proven to be adenoma in our case series.
We have reported seven cases of filiform polyposis involving the sigmoid colon in Koreans who had no definite history of IBD or intestinal tuberculosis. Up to the present, studies regarding filiform polyposis syndrome located in the left side of the colon are insufficient. Continuous close follow-up of these seven patients and collection of large numbers of cases should be performed in order to understand the natural history and observe the possibility of progression into cancer.
Peer reviewers: Dr. Benjamin Perakath, Professor, Department of Surgery Unit 5, Christian Medical College, Vellore 632004, Tamil Nadu, India; Catherine Walter, MD, Department of Surgery, Cheltenham General Hospital, Sandford Road, Cheltenham, GL51 7AN, United Kingdom
S- Editor Wang JL L- Editor Logan S E- Editor Zheng XM
| 1. | Srivastava A, Redston M, Farraye FA, Yantiss RK, Odze RD. Hyperplastic/serrated polyposis in inflammatory bowel disease: a case series of a previously undescribed entity. Am J Surg Pathol. 2008;32:296-303. [Cited in This Article: ] |
| 2. | Rozenbajgier C, Ruck P, Jenss H, Kaiserling E. Filiform polyposis: a case report describing clinical, morphological, and immunohistochemical findings. Clin Investig. 1992;70:520-528. [Cited in This Article: ] |
| 3. | Cheng EH, Brugge WR. Filiform polyposis in a patient without history of inflammatory bowel disease. J Clin Gastroenterol. 1989;11:479-481. [Cited in This Article: ] |
| 4. | Oakley GJ 3rd, Schraut WH, Peel R, Krasinskas A. Diffuse filiform polyposis with unique histology mimicking familial adenomatous polyposis in a patient without inflammatory bowel disease. Arch Pathol Lab Med. 2007;131:1821-1824. [Cited in This Article: ] |
| 5. | Tajiri T, Tate G, Mitsuya T, Endo Y, Inoue K, Yoshiba M, Kunimura T, Morohoshi T. Localized giant inflammatory polyposis (filiform polyposis) with diverticula in ulcerative colitis. J Gastroenterol. 2003;38:912-914. [Cited in This Article: ] |
| 6. | Hirasaki S, Matsubara M, Ikeda F, Taniguchi H, Suzuki S. Inflammatory fibroid polyp occurring in the transverse colon diagnosed by endoscopic biopsy. World J Gastroenterol. 2007;13:3765-3766. [Cited in This Article: ] |
| 7. | Vainer B, Jess T, Andersen PS. Rapid tumour-like growth of giant filiform polyposis in a patient without a history of chronic bowel inflammation. APMIS. 2007;115:1306-1310. [Cited in This Article: ] |
| 8. | Yantiss RK, Oh KY, Chen YT, Redston M, Odze RD. Filiform serrated adenomas: a clinicopathologic and immunophenotypic study of 18 cases. Am J Surg Pathol. 2007;31:1238-1245. [Cited in This Article: ] |
| 9. | Chen SC, Rex DK. Variable detection of nonadenomatous polyps by individual endoscopists at colonoscopy and correlation with adenoma detection. J Clin Gastroenterol. 2008;42:704-707. [Cited in This Article: ] |
| 10. | Park YB, Cheung DY, Kim JI, Park SH, Cho SH, Han JY, Kim JK, Choi KY. A large inflammatory fibroid polyp in the sigmoid colon treated by endoscopic resection. Intern Med. 2007;46:1647-1649. [Cited in This Article: ] |
| 11. | Macaigne G, Boivin JF, Cheaib S, Auriault ML, Deplus R. [Single filiform polyp revealed by severe haemorrhage in a patient with normal colon. Report of a case and review of the literature]. Gastroenterol Clin Biol. 2006;30:913-915. [Cited in This Article: ] |
| 12. | Hyman NH, Anderson P, Blasyk H. Hyperplastic polyposis and the risk of colorectal cancer. Dis Colon Rectum. 2004;47:2101-2104. [Cited in This Article: ] |
| 13. | Renaut AJ, Douglas PR, Newstead GL. Hyperplastic polyposis of the colon and rectum. Colorectal Dis. 2002;4:213-215. [Cited in This Article: ] |
| 14. | Hawkins NJ, Gorman P, Tomlinson IP, Bullpitt P, Ward RL. Colorectal carcinomas arising in the hyperplastic polyposis syndrome progress through the chromosomal instability pathway. Am J Pathol. 2000;157:385-392. [Cited in This Article: ] |
| 15. | Kurobe M, Abe K, Kinoshita N, Anami M, Tokai H, Ryu Y, Wen CY, Kanematsu T, Hayashi T. Hyperplastic polyposis associated with two asynchronous colon cancers. World J Gastroenterol. 2007;13:3255-3258. [Cited in This Article: ] |
| 16. | Liljegren A, Lindblom A, Rotstein S, Nilsson B, Rubio C, Jaramillo E. Prevalence and incidence of hyperplastic polyps and adenomas in familial colorectal cancer: correlation between the two types of colon polyps. Gut. 2003;52:1140-1147. [Cited in This Article: ] |
| 17. | Yano T, Sano Y, Iwasaki J, Fu KI, Yoshino T, Kato S, Mera K, Ochiai A, Fujii T, Yoshida S. Distribution and prevalence of colorectal hyperplastic polyps using magnifying pan-mucosal chromoendoscopy and its relationship with synchronous colorectal cancer: prospective study. J Gastroenterol Hepatol. 2005;20:1572-1577. [Cited in This Article: ] |