Published online Apr 21, 2010. doi: 10.3748/wjg.v16.i15.1867
Revised: November 27, 2009
Accepted: December 4, 2009
Published online: April 21, 2010
AIM: To evaluate the incidence and risk factors for the development of anemia after Roux-en-Y gastric bypass (RYGB).
METHODS: A retrospective analysis of patients undergoing RYGB from January 2003 to November 2007 was performed. All patients had a preoperative body mass index > 40 kg/m2. A total of 206 patients were evaluated. All patients were given daily supplements of ferrous sulfate tablets for 2 wk following their operation. Hematological and metabolic indices were routinely evaluated following surgery. Patients were followed for a minimum of 86 wk.
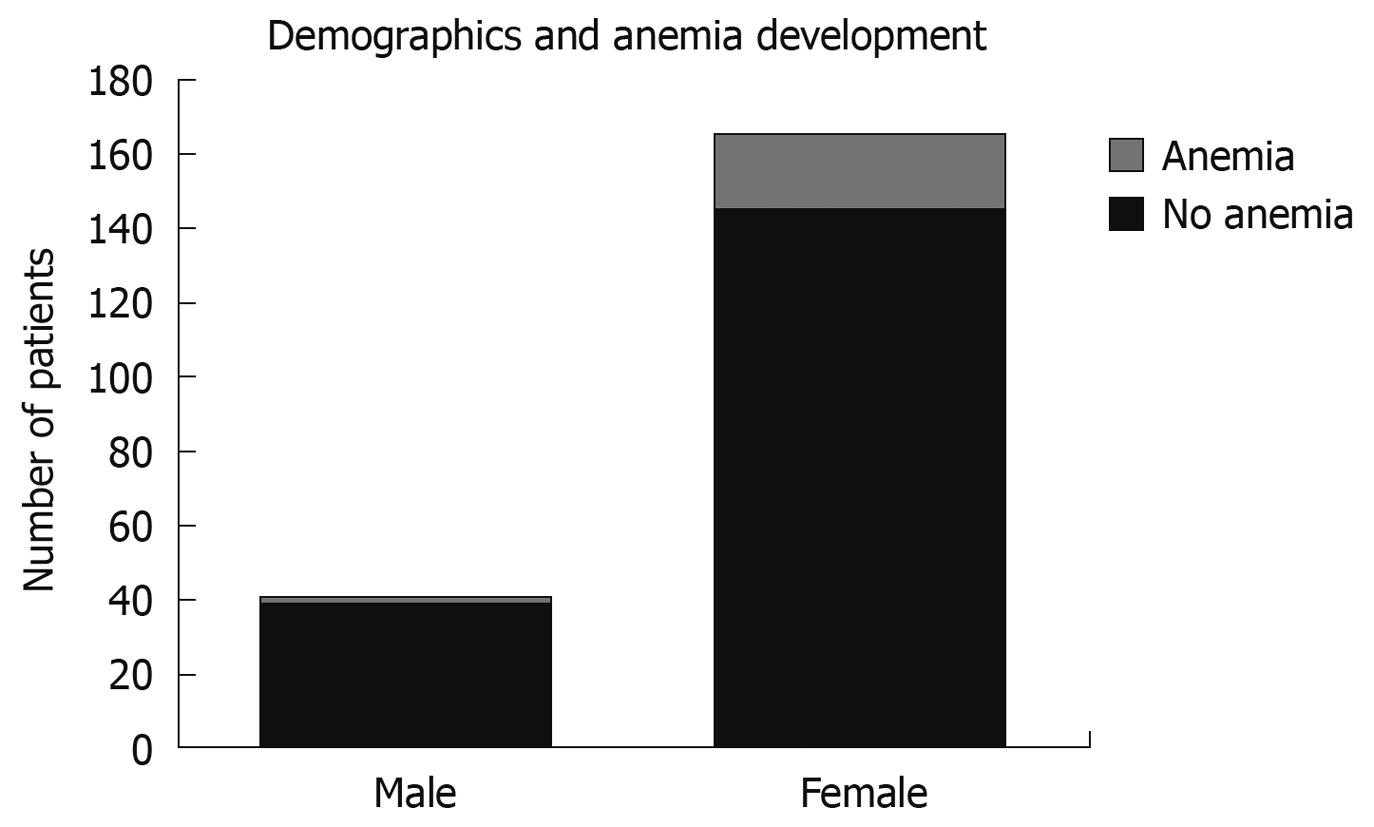
RESULTS: There were 41 males and 165 females with an average age of 40.8 years. 21 patients (10.2%) developed post-operative anemia and 185 patients (89.8%) did not. Anemia was due to iron deficiency in all cases. The groups had similar demographics, surgical procedure and co-morbidities. Menstruation (P = 0.02) and peptic ulcer disease (P = 0.01) were risk factors for the development of post-operative anemia.
CONCLUSION: Iron deficiency anemia is frequent. RYGB surgery compounds occult blood loss. Increased ferrous sulfate supplementation may prevent iron depletion in populations at increased risk.
- Citation: Avgerinos DV, Llaguna OH, Seigerman M, Lefkowitz AJ, Leitman IM. Incidence and risk factors for the development of anemia following gastric bypass surgery. World J Gastroenterol 2010; 16(15): 1867-1870
- URL: https://www.wjgnet.com/1007-9327/full/v16/i15/1867.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i15.1867
Morbid obesity is one of the most common causes of morbidity and mortality in Western countries, and its incidence is rising with unpredictable consequences. It has been estimated that in the next 20 years, 40% of the population in the United States will be morbidly obese with a body mass index (BMI) greater than 30 kg/m2[1].
Roux-en-Y gastric bypass (RYGB) has become a common procedure for achieving short- and long-term weight loss. It has gained great popularity among surgeons and patients in recent years. Long-term complications are still being discovered, and a variety of nutritional problems have been reported[2]. Because of the altered anatomy, absorption of iron from the proximal gastrointestinal tract is impaired. Anemia develops in some patients with inadequate oral supplementation or chronic occult blood loss. The purpose of this study is to identify the incidence and risk factors of anemia in morbidly obese patients who underwent RYGB.
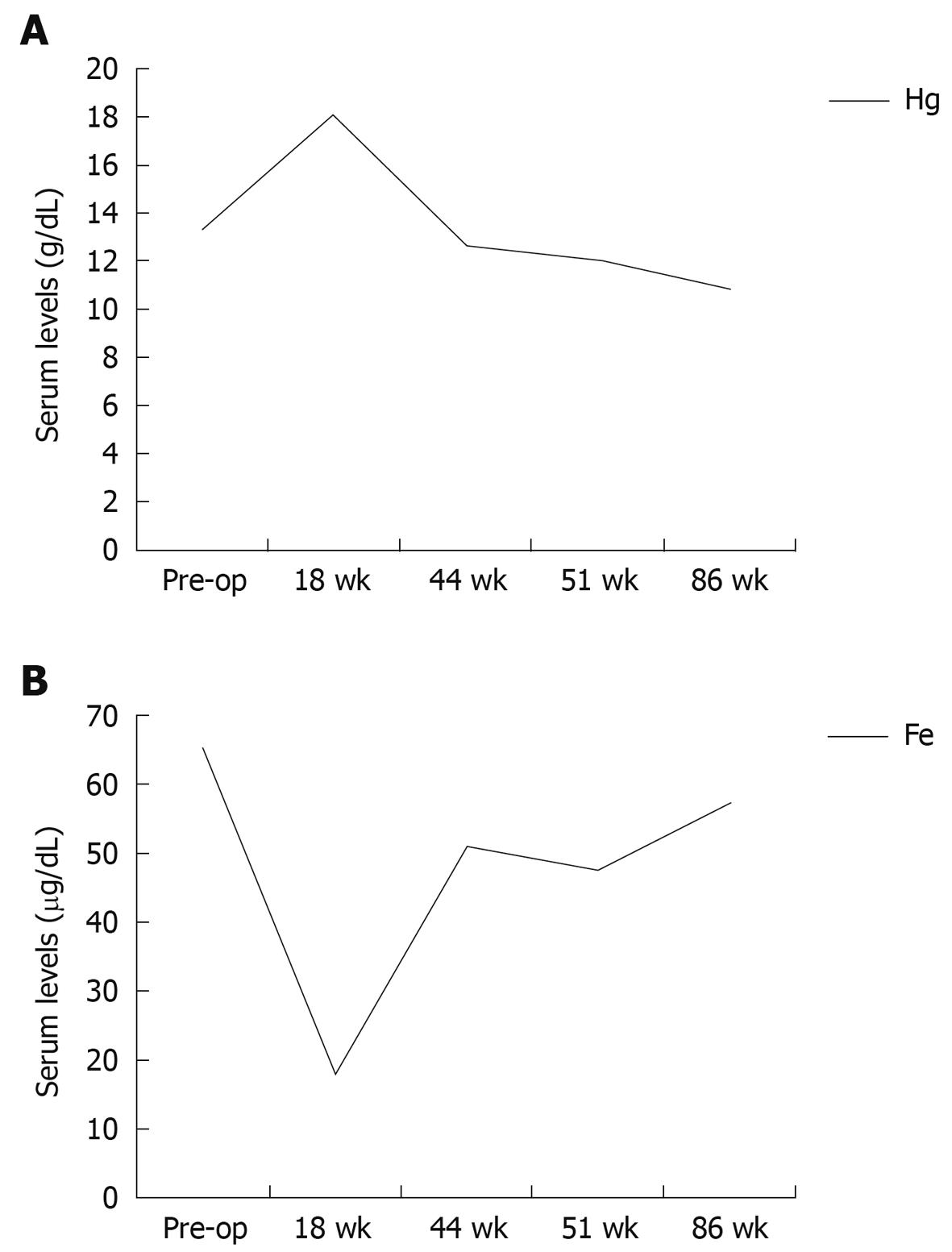
After approval by the Institutional Review Board of Beth Israel Medical Center, a retrospective review of 206 medical records of patients who had undergone RYGB for the treatment of morbid obesity from January 2003 to November 2007 was conducted. Information gathered included demographic characteristics (age, gender, and ethnicity); BMI; past medical and surgical history; relevant laboratory values (pre- and post-operative levels of serum hemoglobin (Hg), hematocrit, mean corpuscular volume, iron, ferritin, and total iron binding capacity); length of bypass; and degree of weight loss after surgery.
One surgeon (IML) performed all gastric bypass operations using the same operative technique. All patients included in the study underwent standard RYGB surgery with the biliopancreatic limb measured to be 70 + BMI (in cm). The alimentary limb was 75 cm in length. Post-operatively, all patients were given a standard chewable multivitamin (Centrum Chewable, Wyeth Consumer Health Care) and ferrous sulfate tablets, 320 mg daily, starting on the 12th d after the operation. All patients were followed closely by a team of dietitians, bariatric surgeons, and psychologists, both before and after the operation. Laboratory data for hematologic and metabolic indices were obtained at frequent intervals post-operatively. Anemia was defined as serum Hg < 11 g/dL in men, and < 10 g/dL in women. Patients with epigastric pain and/or anemia underwent diagnostic upper gastrointestinal endoscopy. Marginal ulcer was treated with sucralfate slurry and oral proton pump inhibitors for a minimum of 2 wk and patients were reexamined endoscopically 6 wk later.
Statistical analysis using the Student t-test was used to compare pre- and post-operative serum levels of Hg, iron, and total iron binding capacity, and the χ2 test was utilized to compare categorical data. The level of statistical significance was set at P≤ 0.05.
Of 206 patients analyzed, 41 (19.9%) were men and 165 (80.1%) women, with a mean age of 40.8 years (range: 18-60 years). A total of twenty-one (10.2%) patients developed anemia at some point during the post-operative period (Figure 1). Following statistical analysis, patients with the greatest risk for anemia were menstruating females (P = 0.02) and patients found to have marginal ulcer on endoscopy (P = 0.01). In all cases the anemia was due to iron deficiency (low serum ferritin, elevated total iron binding capacity, and low mean corpuscular volume). Table 1 shows the associated co-morbidities in the patients. The mean values of serum Hg and iron pre- and post-operatively (at 18, 44, 51, and 86 wk after the operation) for all patients are shown in Figure 2A and B. In the immediate post-operative period, serum Hg increased compared to the pre-operative state, and then decreased slowly over time. In contrast, serum iron dropped significantly in the immediate post-operative period, and then rose gradually with oral supplementation.
| Co-morbidity | % of patients without anemia | % of patients with anemia | P |
| Hypertension | 81.1 | 79.5 | 0.72 |
| Diabetes mellitus | 24.2 | 21.0 | 0.71 |
| Asthma | 29.5 | 19.8 | 0.89 |
| Smoking | 49.0 | 44.1 | 0.86 |
| Menstruation | 67.7 | 84.2 | 0.02 |
| Peptic ulcer disease | 6.0 | 22.0 | 0.01 |
| Coronary artery disease | 7.9 | 14.2 | 0.75 |
| Thyroid disease | 13.2 | 5.6 | 0.19 |
Nutritional deficiencies following RYGB have been previously reported. Vitamin deficiencies[3], disorders of calcium[4] and copper homeostasis[5] have been reported elsewhere. Iron deficiency anemia presents a special clinical challenge. Disturbing behaviors such as pica (eating of non-food substances) and pagophagia (excessive ice-eating) have been observed in patients with anemia following gastric bypass surgery[6,7]. Severe iron deficiency anemia may require parenteral injection of iron or even packed red blood cell transfusion[8].
Anemia after RYGB may be multi-factorial; resulting from impaired absorption due to the surgically altered gastrointestinal tract, inadequate oral intake, or due to occult blood loss. Anemia may result from bleeding due to the operation itself, such as oozing from the staple or suture lines, marginal ulcers, gastritis, and anastomotic bleeding or due to malabsorption of compounds important for the metabolism of Hg, such as iron, folate, thiamine, vitamin B12, niacin, riboflavin, vitamin C, zinc, and copper[1,9]. Diminished intake of red meats (a major natural source of iron) after gastric bypass surgery may further contribute to iron deficiency in these patients[10]. The most prevalent type of anemia is iron deficiency, since iron is absorbed by the duodenum, and this type of anemia results from direct malabsorption due to exclusion of the duodenum from orally ingested nutrients. In addition, the food bolus does not encounter normal amounts of gastric acid secreted by the distal stomach which results in impaired conversion of ingested ferric iron to absorbable ferrous iron[9]. Although prophylactic multivitamin supplements are routinely prescribed for RYGB patients, there are limited data in the medical and surgical literature demonstrating the efficacy of these supplements in the prevention of anemia after gastric bypass surgery[11].
Symptoms of iron deficiency anemia may be nonspecific but include fatigue and muscle weakness, dyspnea, and chest discomfort[12]. Typical laboratory findings include low serum ferritin, elevated total iron binding capacity, low mean corpuscular volume, and decreased intracellular Hg concentration. As such, iron deficiency anemia is typically hypochromic and microcytic[13].
The results of the present study show that 10.2% of our patients developed iron deficiency anemia after RYGB, which is lower than the published data[14]. It has been reported that anemia correlated best with serum transferrin saturation[15]. Coupaye et al[8] also reported an incidence of anemia in 10% of patients. The present study demonstrates that risk factors for the development of iron deficiency anemia following RYGB are menstruation (P = 0.02) and peptic ulcer disease (P = 0.01). It is important to note that these patients developed anemia at some point during the post-operative period, despite being on standard iron supplementation. This may indicate that the current iron supplementation regimens used may not be adequate to prevent the development of iron deficiency anemia in certain patients after RYGB surgery. Love and Billett[16] suggested that the risk of anemia following bariatric surgical procedures continues for life. The incidence of anemia does not appear to be greater following duodenal switch operations[17].
Brolin et al[11] found that multivitamin supplements lowered the incidence of folate deficiency, but did not prevent iron or vitamin B12 deficiency. However, the authors did not suggest the prophylactic supplementation of vitamin B12, simply because the patients did not develop clinically important deficiency of this vitamin post-operatively. On the other hand, they found that iron deficiency is very resistant to oral iron supplementation, especially in menstruating women, leading them to prescribe prophylactic high doses of oral iron (50 mg or more)[11]. Varma et al[18] found that menstruating females were more likely to require parenteral iron therapy after bariatric surgery. Other authors have suggested the addition of vitamin C to oral iron supplementation, but without great success[19]. Previous reports suggest early parenteral iron replacement therapy in patients who do not respond to oral iron therapy in order to prevent anemia-related complications and to maintain patients’ quality of life[2,17]. In a prospective, double-blind, randomized study, Brolin et al[20] found that prophylactic oral supplementation of 320 mg iron twice daily consistently prevented iron deficiency in menstruating women after RYGB.
In conclusion, it is characteristic that iron deficiency anemia secondary to malabsorption may not start until 2-3 mo after RYGB and can be present up to 2 years later[1] as well as refractory to oral supplementation[20]. As a result, it is of utmost importance that a protocol of long-term follow-up and close biologic and metabolic monitoring of patients after RYGB and the need for a more aggressive therapeutic approach when anemia has been diagnosed is established. Increased ferrous supplementation may be necessary to prevent iron depletion in populations at increased risk of developing iron deficiency anemia after RYGB surgery, such as menstruating women and patients with peptic ulcer disease.
With the wide application of bariatric surgery in young patients, long-term follow-up is necessary. Iron deficiency and other causes of anemia are prevalent in a large percentage of patients.
Females of childbearing age and patients with peptic ulcer disease are at the greatest risk for anemia following gastric bypass surgery.
Routine blood work with regular complete blood counts and serum iron levels are required to prevent severe anemia, which may become refractory to oral supplementation.
Patients with anemia should have endoscopic evaluation to determine possible peptic ulcer disease or other etiologies. Women with heavy menstrual flow should be counseled about the need for routine supplementation.
Bariatric surgery is performed for patients with morbid obesity (body mass index greater than 40 kg/m2 or greater than 35 kg/m2 for patients with weight-related morbidities) hypertension, non-insulin diabetes or obstructive sleep apnea.
This paper looked for the anemia commonly encountered problem after bariatric surgery.
Peer reviewer: Ekmel Tezel, MD, PhD, Associate Professor, Department of General Surgery, Gazi University, Faculty of Medicine, Besevler, Ankara 06500, Turkey
S- Editor Wang YR L- Editor Webster JR E- Editor Zheng XM
| 1. | Frezza EE, Moreland A. Anemia after gastric bypass: still a risky business? South Med J. 2008;101:983-984. |
| 2. | Mizón C, Ruz M, Csendes A, Carrasco F, Rebolledo A, Codoceo J, Inostroza J, Papapietro K, Pizarro F, Olivares M. Persistent anemia after Roux-en-Y gastric bypass. Nutrition. 2007;23:277-280. |
| 3. | Alvarez-Leite JI. Nutrient deficiencies secondary to bariatric surgery. Curr Opin Clin Nutr Metab Care. 2004;7:569-575. |
| 4. | Avgerinos DV, Leitman IM, Martínez RE, Liao EP. Evaluation of markers for calcium homeostasis in a population of obese adults undergoing gastric bypass operations. J Am Coll Surg. 2007;205:294-297. |
| 5. | Griffith DP, Liff DA, Ziegler TR, Esper GJ, Winton EF. Acquired copper deficiency: a potentially serious and preventable complication following gastric bypass surgery. Obesity (Silver Spring). 2009;17:827-831. |
| 6. | Kushner RF, Gleason B, Shanta-Retelny V. Reemergence of pica following gastric bypass surgery for obesity: a new presentation of an old problem. J Am Diet Assoc. 2004;104:1393-1397. |
| 7. | Kushner RF, Shanta Retelny V. Emergence of pica (ingestion of non-food substances) accompanying iron deficiency anemia after gastric bypass surgery. Obes Surg. 2005;15:1491-1495. |
| 8. | Coupaye M, Puchaux K, Bogard C, Msika S, Jouet P, Clerici C, Larger E, Ledoux S. Nutritional consequences of adjustable gastric banding and gastric bypass: a 1-year prospective study. Obes Surg. 2009;19:56-65. |
| 9. | Marinella MA. Anemia following Roux-en-Y surgery for morbid obesity: a review. South Med J. 2008;101:1024-1031. |
| 10. | Muñoz M, Botella-Romero F, Gómez-Ramírez S, Campos A, García-Erce JA. Iron deficiency and anaemia in bariatric surgical patients: causes, diagnosis and proper management. Nutr Hosp. 2009;24:640-654. |
| 11. | Brolin RE, Gorman JH, Gorman RC, Petschenik AJ, Bradley LJ, Kenler HA, Cody RP. Are vitamin B12 and folate deficiency clinically important after roux-en-Y gastric bypass? J Gastrointest Surg. 1998;2:436-442. |
| 12. | Marinella MA. "Tomatophagia" and iron-deficiency anemia. N Engl J Med. 1999;341:60-61. |
| 13. | Avinoah E, Ovnat A, Charuzi I. Nutritional status seven years after Roux-en-Y gastric bypass surgery. Surgery. 1992;111:137-142. |
| 14. | Vargas-Ruiz AG, Hernández-Rivera G, Herrera MF. Prevalence of iron, folate, and vitamin B12 deficiency anemia after laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2008;18:288-293. |
| 15. | Rhode BM, Shustik C, Christou NV, MacLean LD. Iron absorption and therapy after gastric bypass. Obes Surg. 1999;9:17-21. |
| 16. | Love AL, Billett HH. Obesity, bariatric surgery, and iron deficiency: true, true, true and related. Am J Hematol. 2008;83:403-409. |
| 17. | Marceau P, Biron S, Hould FS, Lebel S, Marceau S, Lescelleur O, Biertho L, Simard S. Duodenal switch: long-term results. Obes Surg. 2007;17:1421-1430. |
| 18. | Varma S, Baz W, Badine E, Nakhl F, McMullen H, Nicastro J, Forte F, Terjanian T, Dai Q. Need for parenteral iron therapy after bariatric surgery. Surg Obes Relat Dis. 2008;4:715-719. |
| 19. | Topart P. Iron deficiency and anemia after bariatric surgery. Surg Obes Relat Dis. 2008;4:719-720. |