Published online Feb 28, 2009. doi: 10.3748/wjg.15.1007
Revised: January 20, 2009
Accepted: January 27, 2009
Published online: February 28, 2009
In this paper, we report an extremely rare case of an abscess that developed in the inguinal hernial sac after surgery for peritonitis. A 60-year-old man underwent laparoscopic low anterior resection for rectal cancer. One day after this operation, peritoneal drainage and ileostomy were performed for rectal anastomotic leakage. Five days after the second operation, computed tomography revealed an abscess in the left inguinal hernial sac. Subsequently, hernioplasty and resection of the inflamed sac were performed.
- Citation: Ikeda S, Takeda H, Yoshimitsu M, Hinoi T, Yoshida M, Sumitani D, Takakura Y, Kawaguchi Y, Shimomura M, Tokunaga M, Kawahori K, Ohdan H, Okajima M. Abscess in the inguinal hernial sac after peritonitis surgery: A case report. World J Gastroenterol 2009; 15(8): 1007-1009
- URL: https://www.wjgnet.com/1007-9327/full/v15/i8/1007.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.1007
Collections of infected ascites can remain in recesses of the peritoneal cavity after peritonitis. This may lead to inflammation and the formation of an abscess in the hernial sac. The condition of hernial abscess secondary to peritonitis was first reported by Cronin et al[1], and since then, a few other cases have been reported. Although neither peritonitis nor hernia is a rare disease, surgeons do not sufficiently consider the possibility of hernial sac abscess. Here, we present a case in which an inguinal hernial abscess developed following surgery for peritonitis caused by rectal anastomotic leakage.
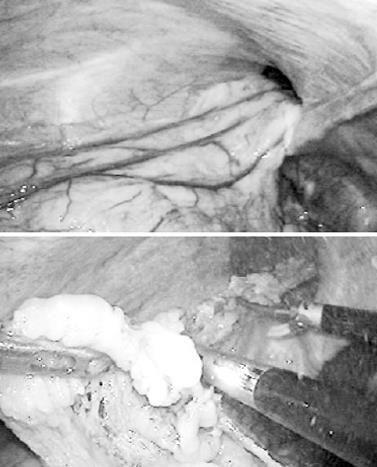
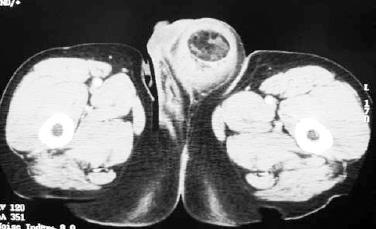
A 60-year-old man underwent laparoscopic low anterior resection for rectal cancer. The intraoperative laparoscopic examination revealed that the patient had a left inguinal hernia, and that a tip of the omentum had extended into the left hernial sac through the deep inguinal ring (Figure 1). The omentum was removed from the hernial sac by using ultrasonic coagulating shears. However, the inguinal hernia was not repaired during the operation. Anastomotic leakage and peritonitis were observed 1 d after the first operation. The patient underwent emergency peritoneal drainage and ileostomy. On day 6 after the first operation (i.e. day 5 after the second operation), the patient noticed a tender mass in the left groin lesion and developed fever. The results of a blood examination revealed elevated C-reactive protein and a high white blood cell count. A computed tomography (CT) scan showed a mass with a diameter of 10 cm, accompanied by inflammation, in the left groin lesion (Figure 2). The mass was suspected to contain liquid and fat, but not bowel tissue. It was diagnosed as an abscess in the inguinal hernial sac, and resection of the sac and iliopubic tract repair were preformed. The wall of the hernial sac had thickened and extended into the left scrotal sac through the posterior region of the inguinal ligament. Infected ascites and inflamed necrotic fat tissue, suspected to be remnants of the omentum, were observed in the hernial sac (Figure 3).
Inguinal hernia and peritonitis with various underlying etiologies are not rare conditions. However, hernial sac abscess associated with peritonitis is very rare. In this paper, we report a case in which an abscess developed in the left inguinal hernial sac following peritonitis caused by rectal anastomotic leakage.
Several cases of abscess in the hernial sac caused by acute appendicitis or by strangulation and perforation of the intestines in the hernial sac have been reported[23]. The protrusion of a vermiform appendix into the inguinal hernial sac, termed an Amyand hernia, and into the femoral hernial sac is termed a De Garengeot hernia[45]. When acute appendicitis occurs in the hernial sac, it may lead to the development of a hernial sac abscess[3]. However, our review of the literature revealed that, after cases of abscess in the hernial sac secondary to peritonitis were reported by Cronin and Ellis in 1959 and Chary in 1977[16], few other such cases have been reported. Sakata et al[7] have reviewed eight reports that describe cases of hernial abscesses secondary to peritonitis, and have classified these conditions into two groups: immediate and delayed hernial abscesses. Immediate hernial abscesses occur during the acute phase of peritonitis, and surgery for the abscesses and peritonitis are often performed simultaneously. On the other hand, delayed abscesses develop after surgery for peritonitis. According to this system of classification, the case reported here is a delayed hernial abscess because it was first noted 5 d after surgery for peritonitis. In several previously reported cases, the sac abscess was noticed without a certain diagnosis of peritonitis before operation[8–11]. This may have been caused by the lack of efficient diagnostic modalities, such as CT, in the past. However, presently, definitive preoperative diagnosis of peritonitis can be assured, as a result of techniques such as CT and abdominal ultrasonography that are easy to perform and provide images of not only the hernial sac but also the abdominal cavity.
In our patient, infected ascites accumulated in the inguinal hernial sac because of rectal anastomotic leakage may have remained after surgery for peritonitis. Further, it is possible that the proliferation of bacteria in the sac may have led to the development of the abscess; however, this possibility was not examined because we did not perform culture of the contents of the hernia abscess. In addition, the omentum, which was partially and insufficiently removed during the operation for rectal cancer, may have played an important role in triggering the inflammation in the sac. Examination of the resected hernial sac revealed that the remnant omentum developed necrosis, possibly because the blood supply to this tissue was intercepted during the operation. The presence of the necrotic omentum in the sac may have rendered the environment conducive to bacterial proliferation in the sac, thus resulting in inflammation and the development of an abscess.
The most important issue is that of whether surgeons should perform an additional operation for hernia detected during surgery. In the present case, we had two opportunities to perform an operation for the inguinal hernia; the first during the operation for rectal cancer and the second during the operation for peritonitis caused by anastomotic leakage. However, we did not perform the operation for hernia on either of these occasions. Hernioplasty with a prosthetic mesh should not be performed during an operation for rectal cancer because the surgical site is not sterile, and this leads to bacterial contamination of the prosthetic mesh. Further, it is obvious that the use of a prosthetic mesh in an operation for peritonitis should be avoided. A more appropriate alternative would be to perform extra-peritoneal laparoscopic hernia repair or tension-free open hernia repair during surgery for rectal cancer and to perform hernioplasty separately. Although we can not definitively state the best method for managing hernia detected during peritonitis surgery, we believe that it is important to adequately wash the hernial sac, as well as the peritoneal cavity with saline, and to administer appropriate antibiotics after the operation[7]. Furthermore, we believe that careful observation of the groin lesion after peritonitis surgery is important in patients with a hernial sac.
In conclusion, we have presented a rare case in which an inguinal hernial sac abscess developed after peritonitis. It is necessary for surgeons to carefully consider the possibility of detecting a hernial sac abscess during surgery for peritonitis and during postoperative follow-up.
| 1. | Cronin K, Ellis H. Pus collections in hernial sacs; an unusual complication of general peritonitis. Br J Surg. 1959;46:364-367. |
| 2. | Kueper MA, Kirschniak A, Ladurner R, Granderath FA, Konigsrainer A. Incarcerated recurrent inguinal hernia with covered and perforated appendicitis and periappendicular abscess: case report and review of the literature. Hernia. 2007;11:189-191. |
| 3. | Meinke AK. Review article: appendicitis in groin hernias. J Gastrointest Surg. 2007;11:1368-1372. |
| 4. | Gillion JF, Bornet G, Hamrouni A, Julles MC, Convard JP. Amyand and de Garengeot' hernias. Hernia. 2007;11:289-290. |
| 5. | Sharma H, Jha PK, Shekhawat NS, Memon B, Memon MA. De Garengeot hernia: an analysis of our experience. Hernia. 2007;11:235-238. |
| 6. | Chary S. Delayed abscess of hernial sac secondary to peritonitis. J R Coll Surg Edinb. 1977;22:282-284. |
| 7. | Sakata A, Kato T, Kume M, Ishikawa K, Shibata S, Sato T, Yamamoto Y. Delayed abscess in a femoral hernial sac secondary to diffuse peritonitis: report of a case. Akita J Med. 2006;33:229-231. |
| 8. | Sellu DP. Pus in groin hernial sacs: a complication of non-generalised peritonitis. Br J Clin Pract. 1987;41:759-760. |
| 9. | Cameron BH. Two cases of primary bacterial peritonitis presenting with a tender hernia. Aust N Z J Surg. 1991;61:794-796. |