Published online Feb 7, 2009. doi: 10.3748/wjg.15.633
Revised: December 11, 2008
Accepted: December 18, 2008
Published online: February 7, 2009
Pulmonary and cerebral lipiodol embolism after transcatheter arterial chemoembolization (TACE) of hepatocellular carcinoma is rare. To our knowledge, only 7 cases have been reported in the literature. We present a case of pulmonary and cerebral lipiodol embolism, and analyzed retrospectively the imaging and clinical data of the patient and conclude the most probable mechanism of pulmonary and cerebral lipiodol embolism, which is different from that of the cases reported previously.
- Citation: Wu JJ, Chao M, Zhang GQ, Li B, Dong F. Pulmonary and cerebral lipiodol embolism after transcatheter arterial hemoembolization in hepatocellular carcinoma. World J Gastroenterol 2009; 15(5): 633-635
- URL: https://www.wjgnet.com/1007-9327/full/v15/i5/633.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.633
Transcatheter arterial chemoembolization (TACE) has been widely used in the treatment of primary hepatocellular carcinoma (HCC). The reported rare or serious complications associated with TACE mainly include: acute hepatic failure, liver abscess, hepatic infarction, hepatic artery occlusion, spontaneous rupture of tumor, gallbladder infarction, perforation of duodenum, acute renal failure, gastrointestinal mucosal ulceration, etc[12]. Cerebral lipiodol embolism is a rare complication of TACE. To our knowledge, only 7 cases of cerebral lipiodol embolism after TACE have been reported so far[3–7]. We herein report a case of pulmonary and cerbral lipiodol embolism after TACE in HCC, and discussed the possible mechanism, which is different from the cases reported previously.
A 36-year-old man who complained of right upper abdominal pain for one week was admitted to our hospital. He had a history of hepatitis B for 10 years. Hepatic computed tomography (CT) revealed a massive HCC in the right liver and tumor thrombosis in the right branch of portal vein. The concentration of blood α-fetoprotein (AFP) was 2.5 ng/mL, while hepatic function was classified as A according to Child-Pugh classification. The surgical resection cannot be performed because of inadequate residual liver volume. So the patient underwent the first TACE.
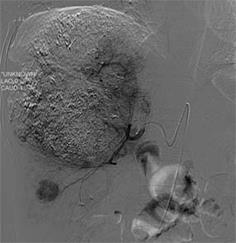
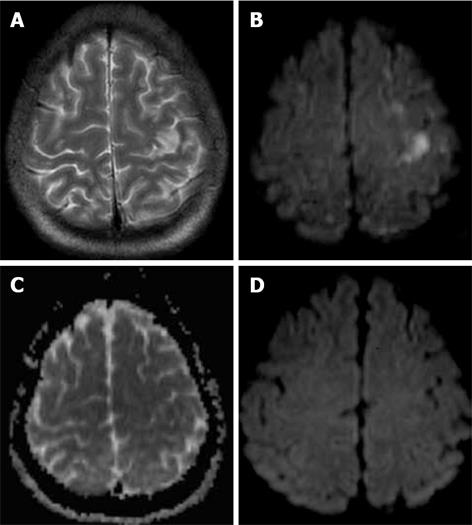
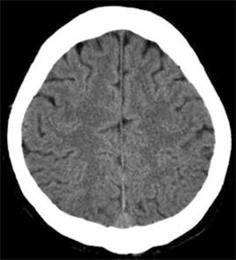
As revealed by angiography, a huge hypervascular tumor located in the right liver was only supplied by the right hepatic artery (RHA) without arteriovenous shunt. TACE was performed via the RHA using a mixture of 40 mg pirarubicin, 40 mL lipiodol, 20 mg hydroxycamptothecine and 150 mg Oxaliplatin. Gelatin sponge particles (560-710 &mgr;m) were used to reduce the flow of tumor feeding artery. After the operation, the patient had a sustained high fever in the afternoon with a maximum of 39.6°C for 10 d. A follow-up non-contrast hepatic CT showed incomplete lipiodol retained in the hepatic tumor and hyper-attenuating lipiodol deposition only in the right collapsed basal lung (Figure 1). The patient recovered and was discharged from hospital two weeks after TACE. Four weeks later, a follow-up hepatic CT demonstrated that incomplete lipiodol deposited in the tumor, so the second TACE was performed. During the second procedure, the hepatic artery angiography revealed that the residual tumor was supplied by RHA, but no arteriovenous shunt was found (Figure 2). A mixture of 40 mg pirarubicin, 40 mL lipiodol, 20 mg hydroxycamptothecine and 150 mg Oxaliplatin was infused the RHA. The embolism process was monitored with fluoroscope and no abnormal flow of the lipiodol was found. Postoperative abdominal X-ray plain film showed dense lipiodol deposition in the tumor. The patient felt transitory numbness in the right hand at the end of the procedure. Two hours after the 2nd TACE, the patient had a numbness and weakness in the right hand and the right fingers could not carry out fine motor activities (such as writing, holding chopsticks, finger’s diadochokinesia, etc.), no symptom of chest tightness and dyspnea occurred. A non-contrast head CT obtained in 53 h after the second TACE showed multiple high-attenuating spots and patch-like lesions in bilateral parietal and frontal cortex (Figure 3). At the same time, a non-contrasted thoracic CT demonstrated small doses of hyper-attenuating lipiodol deposition in the bilateral basal lungs. Cerebral magnetic resonance imaging (MRI) was performed 57 h after TACE by 1.5 T magnetic resonance imaging (Siemens), diffusion-weighted imaging (DWI) and T2WI demonstrated multiple high-signal lesions on the bilateral frontal and parietal lobe (Figure 4A and B); the corresponding lesions showed a low signal area on the apparent diffusion coefficient (ADC) map (Figure 4C). Pulmonary and cerebral lipiodol embolism with acute cerebral infarction after TACE was considered. After the intervention of positive dehydration, diuresis and nutrition of nerve for 10 d, the right hand resumed normal function. Four weeks later, a follow-up head CT showed no abnormality and the previously observed
lipiodol deposition had been cleared entirely (Figure 5). Follow-up MRI revealed no obvious abnormal signal on the DWI (Figure 4D). After the patient underwent TACE, the volume of the normal left liver had a marked compensatory hyperplasia, which was sufficient for safe resection. Surgical tumor resection was performed. During the procedure, the right hepatic massive tumors were seen invading into the diaphragm. Pathological diagnosis revealed primary HCC with large necrosis, surrounded by nodule hepatic cirrhosis. The patient is still living in good health.
Cerebral lipiodol embolism rarely occurs after TACE in HCC. There are only seven reported cases and its possible mechanism was analyzed in detail in three cases. Wu et al[5] thought the link between systemic vessels and pulmonary vessels may occur via the adhesive pleurae or tumor invasion into the thoracic cavity. The lipiodol injected via the inferior phrenic artery may enter the pulmonary circulation, and then entered the systemic circulation via these pathways, resulting in cerebral lipiodol embolism. Matsumoto et al[6] concluded that communication between tumor feeding artery and pulmonary vein might occur via adhesive pleural or tumor invasion into the diaphragm. Therefore, a small dose of lipiodol could enter the systemic circulation quickly and caused cerebral embolism. Choi et al[7] concluded that a large dose of lipiodol and communication between right inferior phrenic artery and pulmonary vessels were contributed to cerebral lipiodol embolism. In this report, we analyzed retrospectively the features of the case as follows. (1) The tumor is huge and was adhered to the diaphragm, suggesting the tumor invading into the diaphragm, which was confirmed during the surgery. (2) The repeated hepatic angiography did not reveal any arteriovenous shunt. (3) The pulmonary lipiodol embolism was found only in the right collapsed basal lung and no neurological signs or symptom of cerebral lipiodol embolism appeared after the first TACE, which suggested that the communication between the tumor feeding artery and the branch of the right pulmonary artery might occur and congenital intrapulmonary arteriovenous shunt did not exist in the field at that time. Given the communication between the tumor feeding artery and pulmonary vein, cerebral lipiodol embolism may occur directly and pulmonary lipiodol embolism in both lung fields. Due to the communication between the tumor feeding artery and hepatic vein, pulmonary lipiodol embolism might be found in both lung fields. So these two possibilities were excluded. (4) The symptom of cerebral lipiodol embolism appeared immediately after the second TACE. According to the features mentioned above, we conclude the most probable mechanism of pulmonary and cerebral lipiodol embolism as follows: Since the tumor invaded into the diaphragm, the communication between the tumor feeding artery and the branches of the right pulmonary artery were presented, and the lipiodol went into the branches of the right pulmonary artery through the communication, resulting in pulmonary lipiodol embolism during the first TACE. While there was no congenital intrapulmonary arteriovenous shunt, the cerebral lipiodol embolism did not form after the first TACE. However, the second intrapulmonary arteriovenous shunt appeared during the pulmonary lipiodol embolism because of increasing pulmonary artery pressure or hypoxia. Therefore, the cerebral lipiodol embolism occurred immediately after the second TACE.
In this case, the head CT revealed multiple hyper-attenuation spots and patch-like lesions in the bilateral frontal and parietal cortex, which suggested hyper-attenuating lipiodol deposition. Cerebral MRI demonstrated multiple ischemic lesions in the bilateral frontal and parietal lobe but not lipiodol deposition. In CT and MRI embolism is observed mainly in the gray matter and the pathological changes are predominant in the white matter[8]. Therefore, CT is considered useful to the diagnosis of cerebral lipiodol embolism, and DWI can help detect lesions and evaluate the therapeutic effect.
Pulmonary and cerebral lipiodol embolism is a rare and serious complication. In this case, pulmonary lipiodol embolism only occurred in the right lung, suggesting the communication between tumor feeding artery and branch of the right pulmonary artery. The risk of pulmonary and cerebral lipiodol embolism should be considered in the tumor treated with TACE again. To prevent the pulmonary and cerebral lipiodol embolism, it is important to consider an individualized therapeutic plan, including the dose of lipiodol and evaluation for the presence of shunt prior to TACE.
| 1. | Sakamoto I, Aso N, Nagaoki K, Matsuoka Y, Uetani M, Ashizawa K, Iwanaga S, Mori M, Morikawa M, Fukuda T. Complications associated with transcatheter arterial embolization for hepatic tumors. Radiographics. 1998;18:605-619. |
| 2. | Xia J, Ren Z, Ye S, Sharma D, Lin Z, Gan Y, Chen Y, Ge N, Ma Z, Wu Z. Study of severe and rare complications of transarterial chemoembolization (TACE) for liver cancer. Eur J Radiol. 2006;59:407-412. |
| 3. | Yoo KM, Yoo BG, Kim KS, Lee SU, Han BH. Cerebral lipiodol embolism during transcatheter arterial chemoembolization. Neurology. 2004;63:181-183. |
| 4. | Takao H, Makita K, Doi I, Watanabe T. Cerebral lipiodol embolism after transcatheter arterial chemoembolization of hepatocellular carcinoma. J Comput Assist Tomogr. 2005;29:680-682. |
| 5. | Wu RH, Tzeng WS, Chang CM. Iodized oil embolization to brain following transcatheter arterial embolization of liver. J Gastroenterol Hepatol. 2005;20:1465-1467. |
| 6. | Matsumoto K, Nojiri J, Takase Y, Egashira Y, Azama S, Kato A, Kitahara K, Miyazaki K, Kudo S. Cerebral lipiodol embolism: a complication of transcatheter arterial chemoembolization for hepatocellular carcinoma. Cardiovasc Intervent Radiol. 2007;30:512-514. |
| 7. | Choi CS, Kim KH, Seo GS, Cho EY, Oh HJ, Choi SC, Kim TH, Kim HC, Roh BS. Cerebral and pulmonary embolisms after transcatheter arterial chemoembolization for hepatocellular carcinoma. World J Gastroenterol. 2008;14:4834-4837. |