Published online Dec 21, 2009. doi: 10.3748/wjg.15.6007
Revised: September 9, 2009
Accepted: September 16, 2009
Published online: December 21, 2009
Aortoesophageal fistula (AEF) is a rare and fatal disorder. It is also a life-threatening cause of massive upper gastrointestinal hemorrhage. Thoracic aortic aneurysm is the most common cause of AEF. Management of a patient with this disorder requires rapid diagnosis and immediate intervention, which is considered the best way to save the patient’s life. We report a case of AEF misdiagnosed as esophageal polyp.
- Citation: Jiao Y, Zong Y, Yu ZL, Yu YZ, Zhang ST. Aortoesophageal fistula: A case misdiagnosed as esophageal polyp. World J Gastroenterol 2009; 15(47): 6007-6009
- URL: https://www.wjgnet.com/1007-9327/full/v15/i47/6007.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.6007
Aortoesophageal fistula (AEF) is a rare and fatal disorder, although it was first described by Dubrueil in 1818. It is also a life-threatening cause of massive upper gastrointestinal hemorrhage. Thoracic aortic aneurysm is the most common cause of AEF. Prompt diagnosis and emergent intervention are substantial to improve the survival of the patients. We report a case of an AEF due to a descending aorta pseudoaneurysm presenting as an esophageal polyp.
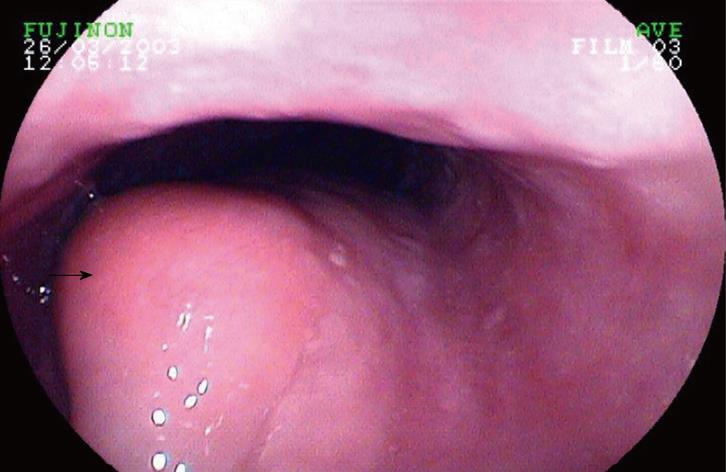
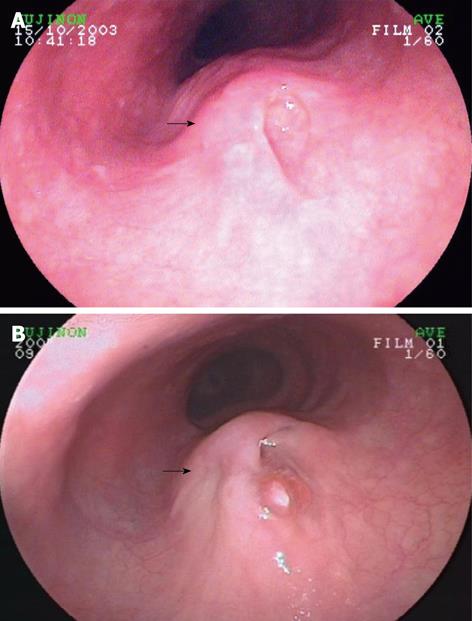
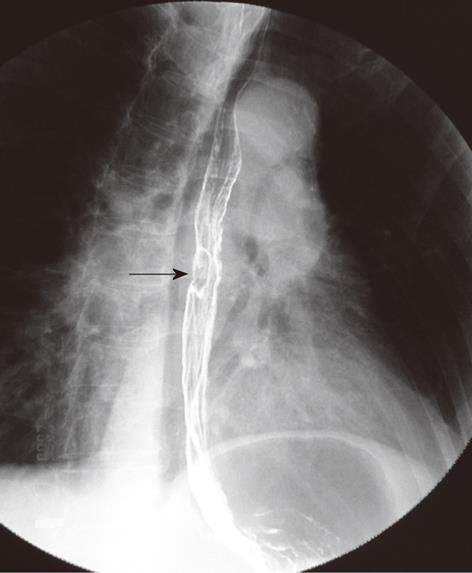
A 62-year-old female patient was admitted to our emergency department for an episode of vomiting bright red blood, with melena and dizziness. Her initial fatal sign was normal when she was in emergency. She had a history of intermittent slight chest pain for 2 years. A gastroscopy was performed which revealed a 4 cm fusiform polyp in the mid-esophagus (Figure 1). It was also diagnosed as esophageal polyp with endoscopic ultrasound. The patient was advised to take further examinations, but she refused. During the following 2 years, she received gastroscopy twice (Figure 2) which showed an orifice-like lesion on the top surface of the polyp. Barium radiography reported a 2cm filling defect in the same location (Figure 3). This patient had a history of rib fracture 20 years ago, but no hypertension or diabetes.
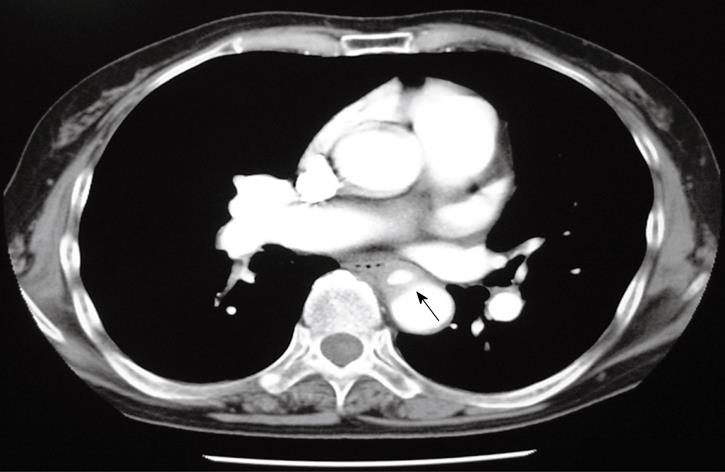
A subsequent enhanced computed tomography (CT) documented a descending aortic pseudoaneurysm that compressed the mid-esophagus (Figure 4). The gastroscopy taken after hospitalization documented the same result as before, without fresh blood or clot on the orifice. Twelve days later, she suddenly experienced a shock for her second hematemesis. Blood pressure dropped down to zero. Angiography was performed until her hemodynamic status was stabilized after blood transfusion and hemostasis. The contrast extravasated from the descending aorta rupture with a diameter of about 0.5 cm (Figure 5), which established a diagnosis as descending aortic pseudoaneurysm. A covered endovascular stent grafting was placed immediately. After confirmed to be in good condition by CT, she was discharged on the 10th postoperative day and has remained healthy since then.
AEF, which constitutes approximately 10% of aortoenteric fistulas, is associated with a high morbidity and mortality. Thoracic aortic aneurysm is the most common cause of AEF, other causes include carcinoma, trauma (including iatrogenic trauma), foreign body ingestion and tuberculous aortitis. Prompt diagnosis and emergent intervention are substantial to improve the survival of the patients. Its classical symptoms, named Chiari’s triad, include dysphagia, mid-thoracic pain and sentinel minor hematemesis followed by exsanguination, as did our patient. Mid-thoracic pain may be caused by distension and dissection of the aortic wall, esophageal perforation, or tumor invasion. Spontaneous cessation of the sentinel minor hemorrhage may be caused by temporary occlusion of the fistula due to spasm of the arterial wall and/or periaortic hematoma, which is later digested by infection or gastrointestinal contents. Fifty-nine percent of the AEF patients had mid-thoracic pain, 45% experienced dysphagia, 65% had sentinel minor hematemesis, and 45% showed Chiari’s triad[1]. Thus, intensive inquiry of patient’s history and careful physical examination are necessary if AEF is suspected.
Early diagnosis is the key point to decrease the mortality from AEF. Endoscopy is always the first examination to be chosen. Endoscopy usually reveals esophageal compression in the mid-upper esophagus or a submucosal hematoma with bluish grey mucosa indicating the aorta wall. A pulsating mass covered with blood clots or a fistula opening is seldom seen. In our case, one of the causes for misdiagnosis is that gastroscopy showed a polyp with an orifice, without bluish grey mucosa or blood clot. However, whether gastroscopy is safe enough to AEF is still controversial. In our opinion, gastroscopy can be performed carefully for upper gastrointestinal hemorrhage, except the definitive AEF is confirmed by CT or aortography[2,3].
Subsequent CT or computed tomographic angiography, which is an accurate and non-invasive method for diagnosing AEF, can demonstrate the location of an aneurysm and its surrounding structures, especially esophagus. Barium radiography may display thoracic aortic aneurysm as an extrinsic compression[3]. Aortography is used for diagnosing the aneurysm, but rarely shows a fistula itself because of lacking blood. Moreover, aortography may provide more opportunities for endovascular aortic stenting in patients who are not actively bleeding[4,5].
After definitive diagnosis, immediate repair is mandatory as surgical repairs offer the only chance to cure the patients with aneurysm and esophageal erosion. Surgery includes thoracic aorta replacement with a synthetic graft, use of cryopreserved arterial allografts and extra-anatomic bypass. Dacron graft is the most commonly used one. Primary repair and esophageal resection should also be done to avoid the complications of infection. In recent years, endovascular stent grafting has been used as an alternative to surgical treatment, but it has some limitations such as AEF remaining as it is, insufficient debridement or drain of mediastinum. Therefore, some authors suggested that an endovascular stent graft should only be used in patients with a high risk of open surgery[2,6]. Since 2005, Pirard et al[7,8] have attempted to combine endovascular with open surgical approach, which brings more hope to decrease the mortality of AEF.
In conclusion, AEF is an uncommon and life-threatening cause of upper gastrointestinal bleeding. The classical clinical triad, such as mid-thoracic pain or dysphagia, a sentinel minor hematemesis followed by exsanguinations and gastroscopy will give a hint to suspected AEF, and thoracic CT scan or aortography can confirm this diagnosis. Surgery or endovascular stent grafting should be chosen individually. However, rapid diagnosis and immediate intervention are considered the best ways to save the patient’s life.
Peer reviewer: James D Luketich, MD, Professor and Chief, Division of Thoracic and Foregut Surgery University of Pittsburgh Medical Center Pittsburgh, PA 15213, United States
S- Editor Tian L L- Editor Ma JY E- Editor Zheng XM
| 1. | Hollander JE, Quick G. Aortoesophageal fistula: a comprehensive review of the literature. Am J Med. 1991;91:279-287. |
| 2. | Prokakis C, Koletsis E, Apostolakis E, Dedeilias P, Dougenis D. Aortoesophageal fistulas due to thoracic aorta aneurysm: surgical versus endovascular repair. Is there a role for combined aortic management? Med Sci Monit. 2008;14:RA48-RA54. |
| 3. | Flores J, Shiiya N, Kunihara T, Yoshimoto K, Yasuda K. Aortoesophageal fistula: alternatives of treatment case report and literature review. Ann Thorac Cardiovasc Surg. 2004;10:241-246. |
| 4. | Amin S, Luketich J, Wald A. Aortoesophageal fistula: case report and review of the literature. Dig Dis Sci. 1998;43:1665-1671. |
| 5. | Lin CS, Tung CF, Yeh HZ, Chang CS, Lin CW. Aortoesophageal fistula with a history of graft treatment for thoracic aortic aneurysm. J Chin Med Assoc. 2008;71:100-102. |
| 6. | Burks JA Jr, Faries PL, Gravereaux EC, Hollier LH, Marin ML. Endovascular repair of bleeding aortoenteric fistulas: a 5-year experience. J Vasc Surg. 2001;34:1055-1059. |
| 7. | Pirard L, Creemers E, Van Damme H, Laurent S, Honoré P, Limet R. In situ aortic allograft insertion to repair a primary aortoesophageal fistula due to thoracic aortic aneurysm. J Vasc Surg. 2005;42:1213-1217. |