Published online Nov 14, 2009. doi: 10.3748/wjg.15.5266
Revised: September 21, 2009
Accepted: September 28, 2009
Published online: November 14, 2009
AIM: To validate high definition endoscopes with Fujinon intelligent chromoendoscopy (FICE) in colonoscopy.
METHODS: The image quality of normal white light endoscopy (WLE), that of the 10 available FICE filters and that of a gold standard (0.2% indigo carmine dye) were compared.
RESULTS: FICE-filter 4 [red, green, and blue (RGB) wavelengths of 520, 500, and 405 nm, respectively] provided the best images for evaluating the vascular pattern compared to white light. The mucosal surface was best assessed using filter 4. However, the views obtained were not rated significantly better than those observed with white light. The “gold standard”, indigo carmine (IC) dye, was found to be superior to both white light and filter 4. Filter 6 (RGB wavelengths of 580, 520, and 460 nm, respectively) allowed for exploration of the IC-stained mucosa. When assessing mucosal polyps, both FICE with magnification, and magnification following dye spraying were superior to the same techniques without magnification and to white light imaging. In the presence of suboptimal bowel preparation, observation with the FICE mode was possible, and endoscopists considered it to be superior to observation with white light.
CONCLUSION: FICE-filter 4 with magnification improves the image quality of the colonic vascular patterns obtained with WLE.
- Citation: Parra-Blanco A, Jiménez A, Rembacken B, González N, Nicolás-Pérez D, Gimeno-García AZ, Carrillo-Palau M, Matsuda T, Quintero E. Validation of Fujinon intelligent chromoendoscopy with high definition endoscopes in colonoscopy. World J Gastroenterol 2009; 15(42): 5266-5273
- URL: https://www.wjgnet.com/1007-9327/full/v15/i42/5266.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.5266
| Blue (B) channel | Green (G) channel | Red (R) channel | |
| 0 | 500 | 445 | 415 |
| 1 | 500 | 470 | 420 |
| 2 | 550 | 500 | 470 |
| 3 | 540 | 490 | 420 |
| 4 | 520 | 500 | 405 |
| 5 | 500 | 480 | 420 |
| 6 | 580 | 520 | 460 |
| 7 | 520 | 450 | 400 |
| 8 | 540 | 415 | 415 |
| 9 | 550 | 500 | 400 |
| Type of endoscopy | Endoscopist 1 | Endoscopist 2 | ||||||
| Mucosal pattern | Vascular pattern | Sum score | n | Mucosal pattern | Vascular pattern | Sum score | n | |
| Without FICE | ||||||||
| Conv | 12 | 35 | 44 | 38 | 21 | 40 | 61 | 38 |
| Indigo | 59 | - | 59 | 20 | 59 | - | 59 | 20 |
| FICE | ||||||||
| 0 | 6 | 20 | 26 | 38 | 8 | 23 | 31 | 38 |
| 1 | 8 | 32 | 40 | 38 | 15 | 33 | 48 | 38 |
| 2 | 13 | 42 | 55 | 38 | 20 | 50 | 70 | 38 |
| 3 | 14 | 43 | 57 | 38 | 17 | 48 | 65 | 38 |
| 4 | 15 | 45 | 60 | 38 | 25 | 49 | 74 | 38 |
| 5 | 11 | 32 | 43 | 38 | 19 | 38 | 57 | 38 |
| 6 | 11 | 38 | 49 | 37 | 19 | 52 | 71 | 37 |
| 7 | 10 | 28 | 38 | 38 | 14 | 34 | 48 | 38 |
| 8 | 11 | 30 | 41 | 38 | 15 | 30 | 45 | 38 |
| 9 | 14 | 44 | 58 | 38 | 18 | 48 | 66 | 38 |
| Endoscopists | 1 (n = 19) | 2 (n = 19) | 3 (n = 19) | 4 (n = 19) | 5 (n = 19) | Global (n = 95) |
| Conv | 9 (47.4) | 13 (68.4) | 12 (63.1) | 10 (52.6) | 10 (52.6) | 54 (56.8) |
| Conv-M | 12 (63.1) | 12 (63.1) | 14 (73.7) | 6 (31.6) | 9 (47.4) | 53 (55.8) |
| FICE | 10 (52.6) | 11 (57.9) | 12 (63.1) | 13 (68.4) | 10 (52.6) | 56 (58.9) |
| FICE-M | 15 (78.9) | 14 (73.7) | 15 (78.9) | 11 (57.9) | 12 (63.1) | 67 (70.5) |
| Indigo | 15 (78.9) | 15 (78.9) | 15 (78.9) | 10 (52.6) | 12 (63.1) | 67 (70.5) |
| Indigo-M | 17 (89.4) | 16 (84.2) | 15 (78.9) | 13 (68.4) | 12 (63.1) | 73 (76.8) |
| Mean percentage | 77.9 | 85.3 | 87.3 | 66.3 | 68.4 |
| Endoscopists | Quality | |||
| FICE-6 + IC better (%) | FICE-6 + IC equal (%) | FICE-6 + IC worse (%) | P1 | |
| 1 | 53.8 | 46.2 | 0 | |
| 2 | 61.5 | 30.8 | 7.7 | |
| 3 | 30.8 | 69.2 | 0 | |
| 4 | 30.8 | 69.2 | 0 | |
| 5 | 69.2 | 30.8 | 0 | |
| Global mean | 49.2 | 0.37 | ||
Chromoendoscopy has been proven to be a valuable tool for the study of colorectal neoplasia. Indigo carmine (IC) can be used with conventional endoscopy[1] or with magnifying colonoscopy[2-5].
Endoscopy manufacturers have developed artificial image enhancements, including “virtual chromoendoscopy”, as a quicker and less messy alternative to dye spraying. The Olympus narrow band imaging (NBI) system employs a narrow band light to increase the contrast. This has been shown to enhance the views, and it provides similar diagnostic accuracy to chromoendoscopy[4-6]. Computed virtual chromoendoscopy (Fujinon intelligent chromoendoscopy, FICE) was subsequently developed[7]; with this technique, the wavelength does not change. Instead, the endoscopy processor reconstructs the image and displays what the mucosa would look like if illuminated using a certain wavelength. FICE has 10 pre-programmed settings, some of which have been tested in the upper gastrointestinal tract[7] and in Barrett’s mucosa[8]. In a third preliminary study, we used one of the FICE settings to compare detection of colonic polyps with white light endoscopy (WLE)[9]. However, this study did not compare the views obtained using different FICE settings and did not comment on the capabilities in the presence of suboptimal bowel cleansing or after the application of indigo carmine dye. Our study aimed to: (1) systematically compare the 10 pre-set FICE settings with normal white light and indigo carmine dye in terms of their ability to enhance views of normal mucosa and polyps, (2) assess FICE in the presence of suboptimal bowel preparation, (3) determine whether poor bowel preparation markedly degrades the capabilities of “virtual chromoendoscopy” systems[10].
High definition magnification colonoscopes (EC-590ZW/M), and the Fujinon EPX-4400 medical video endoscope system were used in the study.
In study one, 560 areas of normal colonic mucosa in 10 patients were observed in real time by two experienced endoscopists (Parra-Blanco A and González N), who assessed the quality of mucosal and vascular pattern views. The views were obtained with white light, 0.5% indigo carmine dye, and the different FICE settings (Table 1) both with and without magnification (× 100). The quality of the mucosal views was scored according to the following scale: 0 (poor), 1 (fair), 2 (good), and 3 (excellent). Each endoscopist was blinded to the other endoscopist’s assessments.
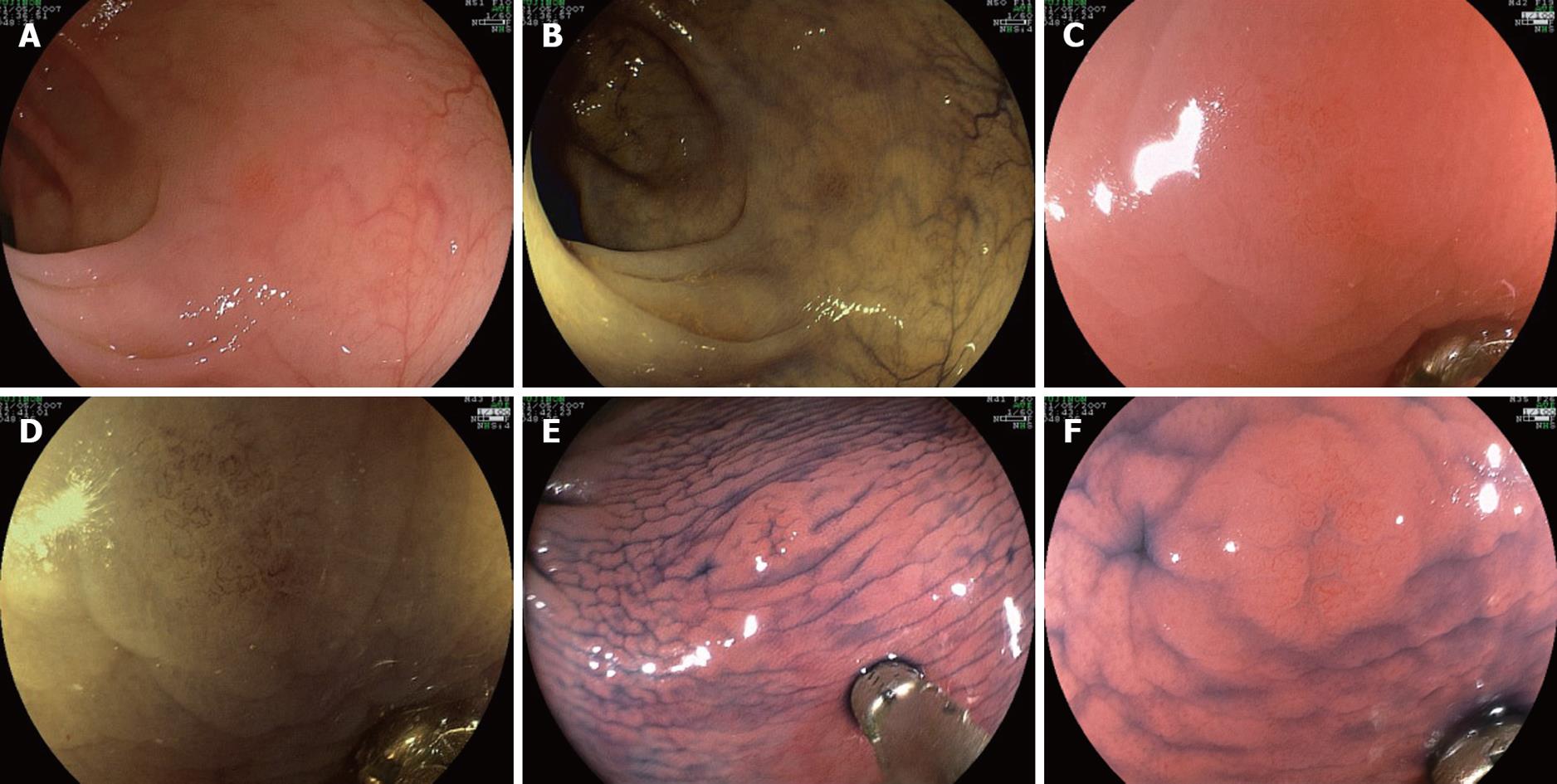
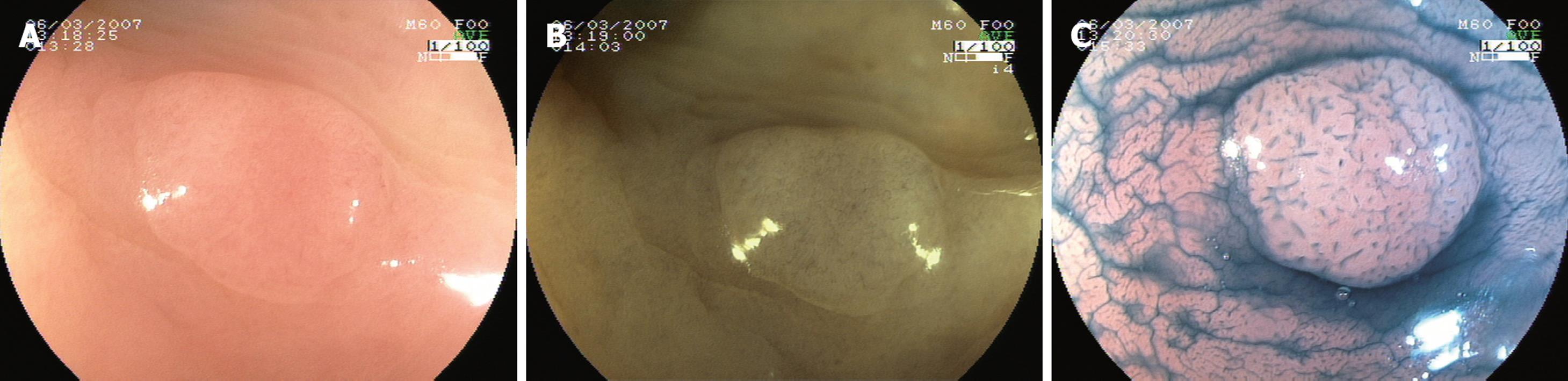
In study two, 114 pictures were taken of 19 mucosal polyps (14 tubular adenomas, 4 hyperplastic polyps, and 1 normal mucosa). The pictures were obtained with white light, 0.5% indigo carmine (IC) dye, and the highest rated FICE settings according to study one (FICE setting 4), both with and without magnification (× 100). Polyp size and shape were estimated by comparison with closed biopsy forceps (Radial Jaw 3, Boston Scientific Corporation). The mean size of the polyps was 2.8 mm (range 1-5 mm). Figure 1 illustrates the sequence of images corresponding to one of the cases.
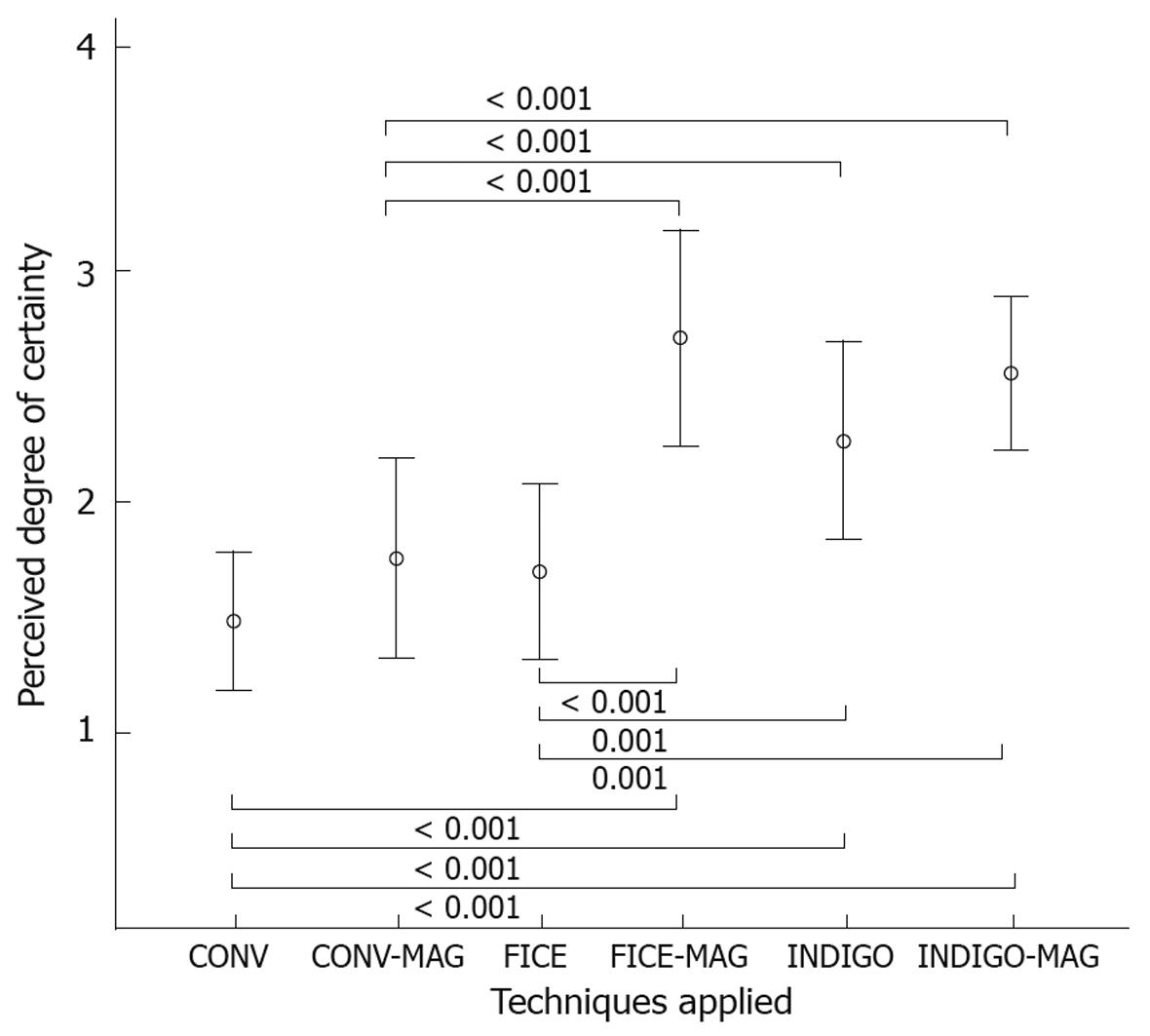
A panel of 5 fully trained endoscopists was asked to classify each lesion into one of the following categories: benign (for types I and II crypt patterns), neoplastic (types III and IV crypts), and invasive (type V pattern)[11]. For the assessment of the capillary pattern, Sano’s classification was used[10]. The panel members were asked to grade the degree of certainty in the prediction according to the following scale: (1) very uncertain, (2) uncertain, (3) reasonably certain, (4) absolutely certain.
In study three, the feasibility of FICE colonoscopy in the presence of suboptimal bowel preparation was evaluated. Images from 17 colonic areas with small or moderate amounts of liquid or solid stools were recorded, both with the conventional view and with FICE setting 4. The panel of endoscopists rated: (a) the image quality of FICE setting 4 as superior, equal, or inferior to that of WLE; (b) the ability of FICE-4 to trace the fecal contents as compared to WLE (superior, equal, or inferior).
In study four, the ability to trace the polyp margin and recognize the irregularities of the polyp surface was compared between FICE setting 4, conventional endoscopy, and IC. Ninety images corresponding to 15 polyps were obtained and presented to the panel. The panel rated the ability of FICE to trace the margin and surface as superior, equal, or inferior to that of the other techniques.
In study five, the feasibility of FICE colonoscopy in IC-stained mucosa was tested. In a preliminary phase, both endoscopists participating in study one had determined that colonoscopy with FICE setting 6 was the most adequate to observe the IC-stained mucosa, with a global image quality that was at least as good as with WLE. Then, 48 images corresponding to 12 polyps were taken, including views with IC and with IC plus FICE setting 6. The members of the panel were asked to rate the ability of FICE-6 plus IC to trace the margin and surface of the polyps as superior, equal, or inferior to the performance of IC.
The study was approved by the Research Ethics Committee of Hospital Universitario de Canarias, and a signed informed consent document was obtained from all participating patients.
No sample sizes were calculated, as this was a pilot study, and no data were available when the study was performed regarding colonoscopy with FICE.
Categorical variables are expressed with frequencies and percentages. Proportions were compared using the χ2 test or Fisher’s exact test whenever required. Means were compared with the unpaired Student’s t test, and means and standard deviations (SD) are reported.
For the same endoscopist, comparisons between techniques on quality of the images were carried out using the Wilcoxon test.
Calculated P < 0.05 values were considered to indicate statistical significance.
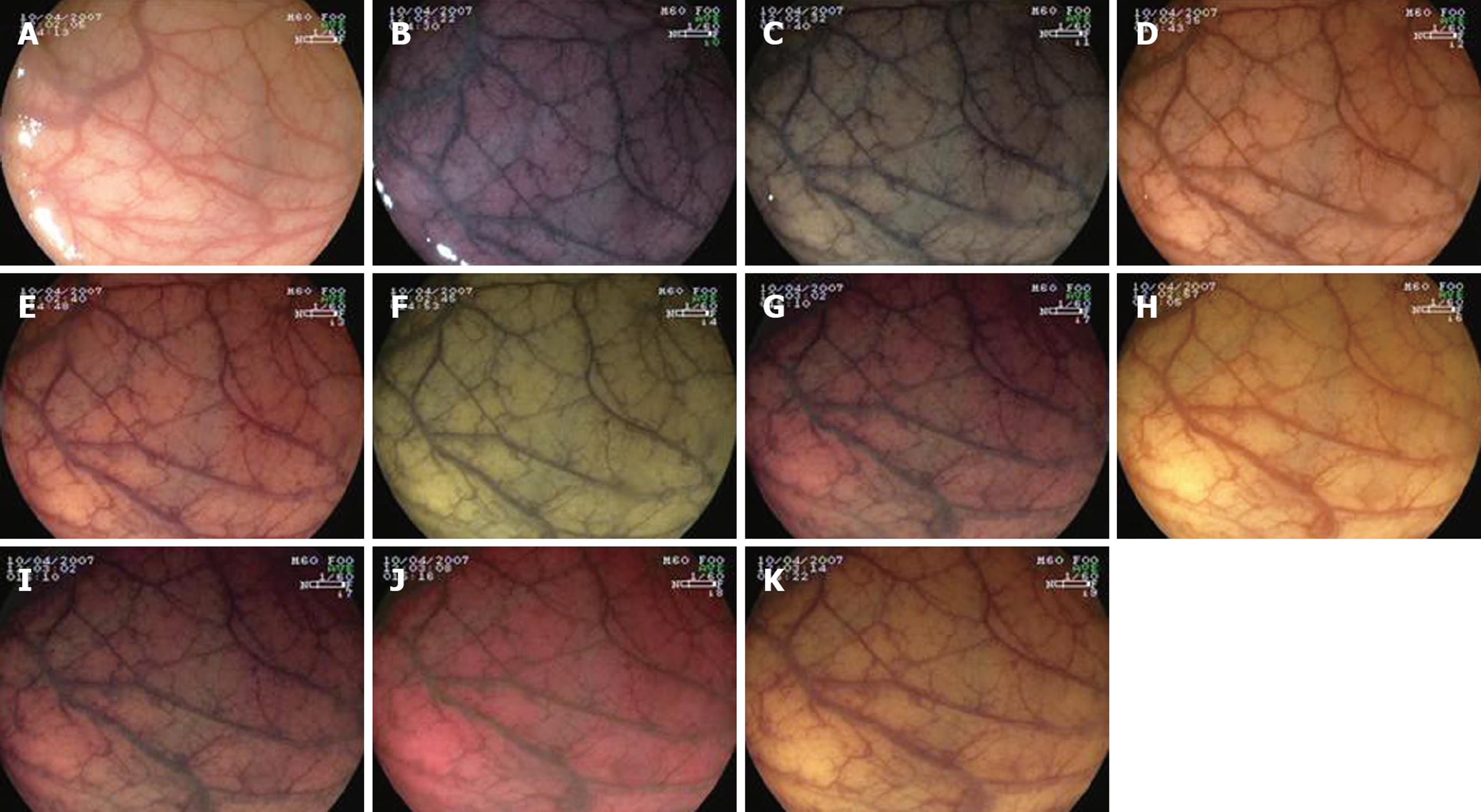
The assessment of FICE settings is shown in Figure 2. In evaluating the normal mucosa, only filter 4 was scored by both assessors as superior to conventional WLE (Table 2). The gold standard for mucosal observation, indigo carmine, was regarded as far superior to any FICE setting according to all assessors. In fact, the normal colonic innominate grooves could only be seen with the aid of dye spraying.
In evaluating the vascular pattern, FICE setting 4 (corresponding to RGB wavelengths 520, 500, and 405 nm, respectively) and FICE setting 2 were found to provide the best image quality. When mucosal and vascular pattern ratings were taken together, FICE setting 4 was considered the best by both assessors.
Study two (Figure 1): The histological predictions for the five participants are indicated in Table 3. In general, the diagnostic accuracy was related to the level of experience of the endoscopists in the panel. IC plus magnification, FICE setting 4 plus magnification, and IC without magnification were the most accurate techniques. The following differences among the techniques were statistically significant (Table 3): Conventional vs IC-Magnification: P = 0.002; Conventional-Magnification vs FICE-Magnification: P = 0.02; Conventional vs IC: P = 0.02; Conventional vs IC-M: P = 0.001; FICE vs FICE-Magnification: P = 0.048; FICE vs IC: P = 0.048; FICE vs IC-Magnification: P = 0.004.
The following differences among endoscopists were statistically significant (Table 3): Endoscopist 2 vs 4: P = 0.003; Endoscopist 2 vs 5: P = 0.006; Endoscopist 3 vs 4: P < 0.001; Endoscopist 3 vs 5: P = 0.002.
The endoscopists’ level of confidence in the endoscopic diagnosis was increased with these techniques compared to making the diagnosis with white light only (Figure 3).
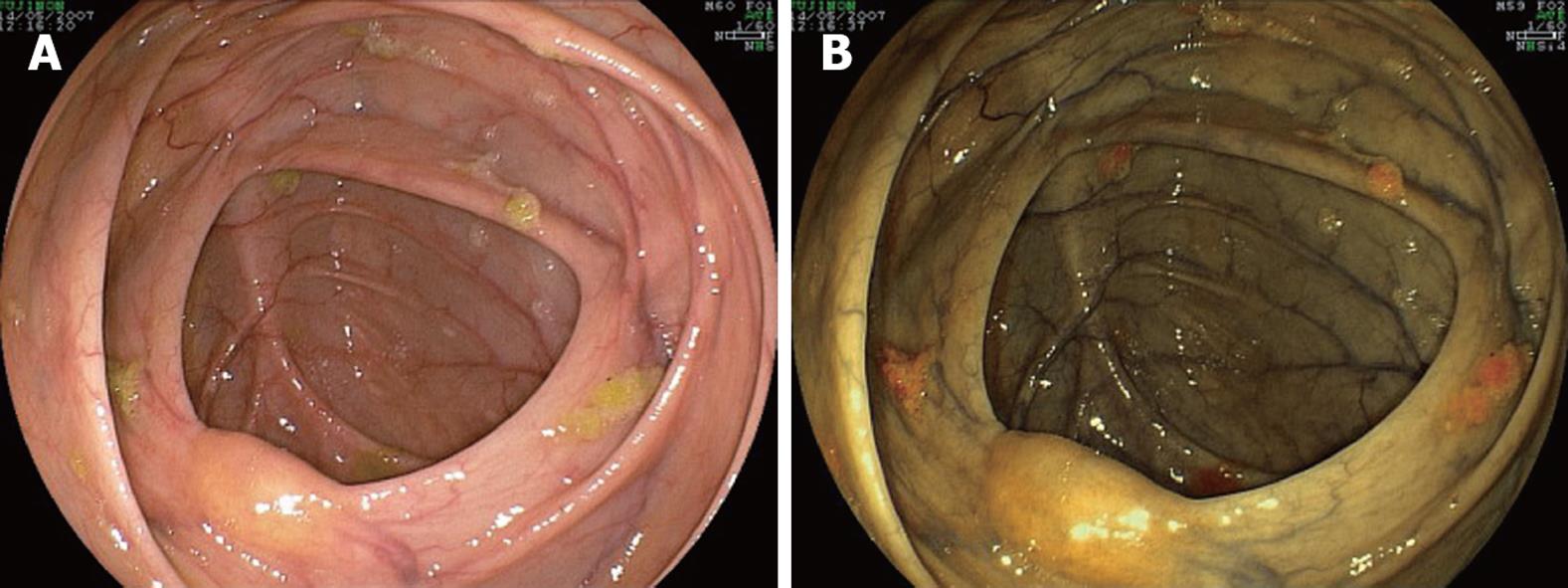
In study three, FICE was particularly useful in evaluating the mucosa in the presence of suboptimal bowel preparation, and the panel found that in that situation, the view was generally better with FICE setting 4 than with WLE (Table 4). Small solid feces showed up as a vivid yellow color and transparent liquid as a darker yellow color; its distinction from colonic mucosa could be clearly seen (Figure 4).
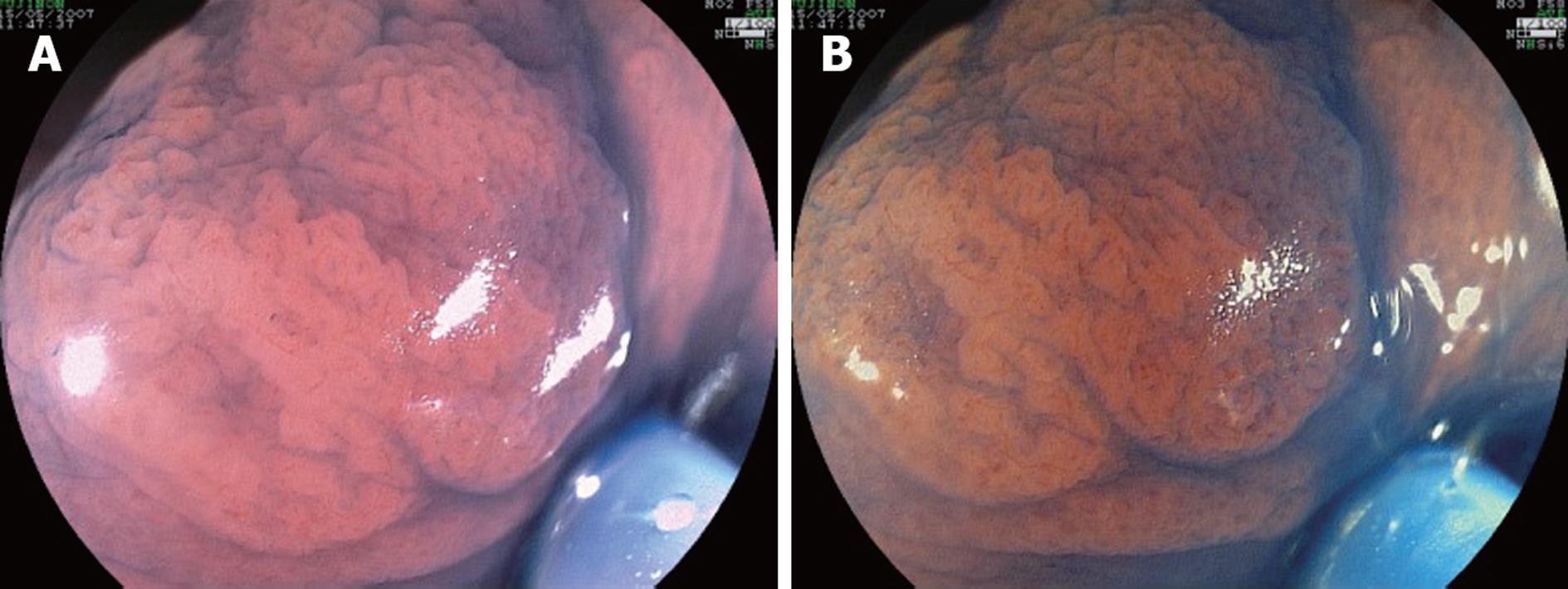
In study four, FICE setting 4 was found to be better than conventional endoscopy for tracing the margin of the polyps and observing the surface irregularities, and IC was found to be better than FICE setting 4 (Tables 5 and 6, Figure 5).
In study five, when the polyps were observed under IC plus FICE setting 6, the view was not considered inferior to that of IC alone (Table 7, Figure 6). Therefore, it can be concluded that colonoscopy with FICE setting 6 in the IC-stained mucosa is feasible.
Virtual chromoendoscopy has been developed by endoscope manufacturers to reduce the need for dye spraying. FICE comes with 10 pre-installed settings, which have not previously been evaluated and compared to normal dye spraying techniques and WLE.
In our study, setting 4 was found to be best when assessing mucosal and vascular architecture. Teixeira et al[12] have reported on the effectiveness of FICE with magnification endoscopes in the differential diagnosis of neoplastic and non-neoplastic lesions. The FICE setting employed was R 500 nm, G 520 nm, and B 405 nm, as we felt that it provided the best imaging of the capillary vessels, after having compared multiple filter settings. However, those comparisons were not probably performed in a structured fashion, as no specific data about the comparisons is available in the study.
We described the settings as provided by the manufacturer. Because it is possible to personalize the filter settings and rename them, care should be taken not to misinterpret the filters used in different studies. Paradoxically, we found that the FICE settings that most closely correlated with the Olympus NBI mode provided the worst mucosal views. NBI and FICE are indeed different technologies, and the results obtained with one of them cannot be extrapolated to the other.
FICE was generally better at assessing vascular architecture than the mucosal surface. Moreover, indigo carmine dye spraying was significantly superior to any FICE setting. In particular, the innominate grooves, important features when recognizing flat lesions, were perfectly outlined by indigo carmine dye.
Magnification appears to be as effective with FICE as with IC, whereas IC would be superior to FICE in the absence of magnification. Because this is a pilot study, these results should be confirmed in larger studies. The endoscopists participating in image interpretation were far more familiar with IC than with FICE. A learning curve in diagnostic interpretation of FICE may exist. Another possible explanation for the superiority of IC over FICE in our study could be that the former seems to provide a better mucosal contrast, and in the absence of magnification, this might lead to significant differences. In the only study available regarding FICE for the diagnosis of colonic polyps, Pohl et al[9] also found that IC and FICE were superior to WLE both with and without magnification. However, no difference was found when IC and FICE were compared. Because the mean size of polyps in their study was 7 mm, and lesions up to 20 mm in size were included, their results cannot be directly compared to those from our study, as our polyps were significantly smaller. Although they performed a sub-analysis on the subgroup of lesions ≤ 5 mm in size, no information was provided about possible differences between IC and FICE. Moreover, images were evaluated for diagnostic performance by one single endoscopist, whereas five endoscopists were involved in our study.
The diagnostic accuracy with the different techniques in our study was lower than in some other series[2,5,13-16]. Possible explanations for such differences are that some series included larger polyps, which are probably easier to diagnose[5,13-15], or that diagnosis was estimated with a live video-endoscopy image and not with stored pictures[2,13], which could enable a more exact diagnosis. Some series used absorptive stains, which can be more accurate[13,14]. Moreover, endoscopists with varying degrees of experience in magnifying colonoscopy participated in our study, and there were significant differences in diagnostic accuracy among them. In a recent study, East et al[16] reported a diagnostic accuracy of 69%-72% for magnification with methylene blue and 72%-84% for magnification plus NBI, which is similar to our findings. Further larger studies should compare FICE with IC without magnification in order to ascertain possible differences between the techniques.
The perceived degree of certainty in the diagnosis given with the different techniques applied was also evaluated. We believe that this issue deserves consideration when test performance is evaluated, as it could have an influence on the therapeutic strategy chosen by the endoscopist. We found that IC (with and without magnification) and FICE plus magnification - the techniques with a higher diagnostic accuracy - were associated with a greater perception of accurate diagnosis, and in fact they were more accurate.
Virtual chromoendoscopy techniques are expected to increase mucosal contrast. In fact, they should probably do so if they are to replace endoscopic stains. In our study, FICE was superior in highlighting the contour of lesions compared with WLE. However, IC remains the gold standard as it was found to be superior to FICE. Machida et al[4] came to a similar conclusion when comparing NBI with dye staining. One very important issue that will have to be explored in future studies is whether FICE or NBI can aid in the recognition of depressed lesions (Paris type 0-IIc). These lesions are frequently small but frequently harbour high grade dysplasia or early invasive cancer[11,17].
Adequate bowel cleansing is a prerequisite for the application of chromoendoscopy, as the mixture of stains and remaining fecal content worsens endoscopic observation[18]. It appears important to determine whether FICE can be applied when there is some fecal content remaining, because in most colonoscopies, at least some liquid material persists. when the NBI technology is used, suboptimal bowel preparation appears to negatively affect the endoscopic view. According to our initial impression and the endoscopists’ subjective opinion measured in the study, FICE setting 4 was better than WLE for adequately observing the colonic mucosa when bowel content was present and for localizing and individualizing small fecal particles. Liquid and especially small fecal particles showed up as a vivid yellow color. This property of FICE might be useful to differentiate more accurately between small polyps and feces, allowing for targeted washing when small particles are detected.
Finally, it is important to know the effect of IC on FICE observation. It is possible that both techniques could be applied in combination for certain indications, as FICE allows for better observation of the vascular pattern and IC more clearly highlights the lesion edge and surface shape. FICE 6 did not interfere with endoscopic observation. The effect of IC on NBI observation has not been described, but in our experience, the endoscopic view is worsened, resulting in a greenish color.
It is noteworthy that in all cases, FICE was applied with magnifying high definition endoscopes (1 300 000 pixels). When we tried conventional endoscopes (resolution 410 000 pixels), we felt that the image quality was greatly worsened when any FICE filter was applied. Therefore, the results of our study apply only to high resolution endoscopes.
Our study has several limitations: first, the determination of the image quality provided by the different filters is unavoidably a subjective issue. However, we used a scale, a method similar to that used in previous studies[4], and each endoscopist was blinded to the assessments of the other endoscopists. Moreover, although filter 4 had the highest scores, other filters also seemed to provide clear endoscopic images, but they were not evaluated in the current study. The effect of these filters in the colon could represent a field of future research. A second limitation is that our pilot study on polyps only included small lesions, and none of the lesions was invasive; therefore, the usefulness of FICE for the prediction of invasiveness was not assessed. Finally, one investigator selected the endoscopic images and also participated in the prediction of histopathological diagnosis. However, he was unaware of the diagnosis, and in fact, he did not review any of the histopathological reports for any endoscopic procedure during the study period. When this investigator’s assessments were excluded, there were no changes in the statistical results for the diagnostic accuracy of the techniques.
In conclusion, FICE setting 4 seems to be the most suitable for the observation of the colonic mucosa with high definition endoscopes. Its performance in the diagnosis of small polyps appears similar to IC when magnification is applied; however, in our pilot study, IC was superior to FICE in the absence of magnification. FICE seems to depict the polyp shape better than WLE but less clearly than IC. The presence of small amounts of liquid or solid feces or IC does not appear to interfere with endoscopic observation when FICE is applied. This is an initial description, and future studies should clarify the role of FICE in colonoscopic diagnosis.
Fujinon intelligent chromoendoscopy (FICE) provides virtual chromoendoscopy, without the need for endoscopic stains. However, knowledge about the most adequate FICE settings in colonoscopy, and how it compares with conventional chromoendoscopy is still limited.
Many issues regarding colonoscopic imaging with FICE have to be explored, including comparison with other virtual chromoendoscopy technologies, traditional chromoendoscopy with stains, and even the influence of the quality of colonic cleansing.
In this study a structured methodology was applied in order to determine which one among the multiple FICE-filters available provides a better observation of the vascular and mucosal patterns. After the most adequate filter was selected, it was applied for the examination of colonic polyps. In previous studies such a methodology to choose the best FICE-filter was not applied or described in detail. Additionally, in this study certain features of FICE imaging are explored, such as the possibility of applying it to observe indigo carmine-stained mucosa, or whether the existence of fecal contents has an influence on FICE imaging.
Our results suggest that FICE is adequate for the observation of the vascular pattern, that indigo carmine is better for examining the fine mucosal surface and the margin and shape of the lesion, and that endoscopic stains (like indigo carmine) can be applied in combination with FICE-6. As opposed to narrow band imaging, indigo carmine or colonic fecal contents do not seem to interfere with FICE imaging. In fact, FICE-4 could clarify whether small mucosal irregularities are really mucosal lesions or adherent particles, and this could have an application in screening colonoscopy.
Virtual chromoendoscopy: The contrast of mucosal and vascular patterns is enhanced without the need of any endoscopic stain, by just pressing a button in the endoscope. FICE: Virtual chromoendoscopy is obtained by means of spectral estimation technology, i.e. computerized image reconstruction by the endoscopic processor. FICE filters or settings: there are 10 pre-programmed filters which are switched on the keyboard, each of which has different settings for estimated R, G, and B wavelengths.
This is a prospective study to validate high definition endoscopes with FICE in colonoscopy. This paper is quite interesting.
Peer reviewer: Giovanni D De Palma, Professor, Department of Surgery and Advanced Technologies, University of Naples Federico II, School of Medicine, Naples 80131, Italy
S- Editor Tian L L- Editor Webster JR E- Editor Lin YP
| 1. | Sonwalkar S, Rotimi O, Rembacken BJ. Characterization of colonic polyps at conventional (nonmagnifying) colonoscopy after spraying with 0.2 % indigo carmine dye. Endoscopy. 2006;38:1218-1223. |
| 2. | Fu KI, Sano Y, Kato S, Fujii T, Nagashima F, Yoshino T, Okuno T, Yoshida S, Fujimori T. Chromoendoscopy using indigo carmine dye spraying with magnifying observation is the most reliable method for differential diagnosis between non-neoplastic and neoplastic colorectal lesions: a prospective study. Endoscopy. 2004;36:1089-1093. |
| 3. | Konishi K, Kaneko K, Kurahashi T, Yamamoto T, Kushima M, Kanda A, Tajiri H, Mitamura K. A comparison of magnifying and nonmagnifying colonoscopy for diagnosis of colorectal polyps: A prospective study. Gastrointest Endosc. 2003;57:48-53. |
| 4. | Machida H, Sano Y, Hamamoto Y, Muto M, Kozu T, Tajiri H, Yoshida S. Narrow-band imaging in the diagnosis of colorectal mucosal lesions: a pilot study. Endoscopy. 2004;36:1094-1098. |
| 5. | Chiu HM, Chang CY, Chen CC, Lee YC, Wu MS, Lin JT, Shun CT, Wang HP. A prospective comparative study of narrow-band imaging, chromoendoscopy, and conventional colonoscopy in the diagnosis of colorectal neoplasia. Gut. 2007;56:373-379. |
| 6. | Gono K, Obi T, Yamaguchi M, Ohyama N, Machida H, Sano Y, Yoshida S, Hamamoto Y, Endo T. Appearance of enhanced tissue features in narrow-band endoscopic imaging. J Biomed Opt. 2004;9:568-577. |
| 7. | Pohl J, May A, Rabenstein T, Pech O, Ell C. Computed virtual chromoendoscopy: a new tool for enhancing tissue surface structures. Endoscopy. 2007;39:80-83. |
| 8. | Pohl J, May A, Rabenstein T, Pech O, Nguyen-Tat M, Fissler-Eckhoff A, Ell C. Comparison of computed virtual chromoendoscopy and conventional chromoendoscopy with acetic acid for detection of neoplasia in Barrett's esophagus. Endoscopy. 2007;39:594-598. |
| 9. | Pohl J, Nguyen-Tat M, Pech O, May A, Rabenstein T, Ell C. Computed virtual chromoendoscopy for classification of small colorectal lesions: a prospective comparative study. Am J Gastroenterol. 2008;103:562-569. |
| 10. | Sano Y, Yoshida S. Optical chromoendoscopy using NBI during screening colonoscopy: Its usefulness and application. Advanced Digestive Endoscopy: Comprehensive Atlas of high resolution endoscopy and Narrowband Imaging. Oxford: Blackwell Publishing 2007; 123-148. |
| 11. | Kudo S, Kashida H, Tamura T, Kogure E, Imai Y, Yamano H, Hart AR. Colonoscopic diagnosis and management of nonpolypoid early colorectal cancer. World J Surg. 2000;24:1081-1090. |
| 12. | Teixeira CR, Torresini RS, Canali C, Figueiredo LF, Mucenic M, Pereira Lima JC, Carballo MT, Saul C, Toneloto EB. Endoscopic classification of the capillary-vessel pattern of colorectal lesions by spectral estimation technology and magnifying zoom imaging. Gastrointest Endosc. 2009;69:750-756. |
| 13. | Kato S, Fujii T, Koba I, Sano Y, Fu KI, Parra-Blanco A, Tajiri H, Yoshida S, Rembacken B. Assessment of colorectal lesions using magnifying colonoscopy and mucosal dye spraying: can significant lesions be distinguished? Endoscopy. 2001;33:306-310. |
| 14. | Hurlstone DP, Cross SS, Adam I, Shorthouse AJ, Brown S, Sanders DS, Lobo AJ. Efficacy of high magnification chromoscopic colonoscopy for the diagnosis of neoplasia in flat and depressed lesions of the colorectum: a prospective analysis. Gut. 2004;53:284-290. |
| 15. | Hirata M, Tanaka S, Oka S, Kaneko I, Yoshida S, Yoshihara M, Chayama K. Magnifying endoscopy with narrow band imaging for diagnosis of colorectal tumors. Gastrointest Endosc. 2007;65:988-995. |
| 16. | East JE, Suzuki N, Saunders BP. Comparison of magnified pit pattern interpretation with narrow band imaging versus chromoendoscopy for diminutive colonic polyps: a pilot study. Gastrointest Endosc. 2007;66:310-316. |
| 17. | Parra-Blanco A, Nicolás-Pérez D, Gimeno-García AZ, Fu KI, Hernández N, Quintero E. An early flat depressed lesion in the cecum progressing to an advanced cancer in 20 months. Gastrointest Endosc. 2007;66:859-861. |