INTRODUCTION
Ectopic pancreas is not an extremely rare pathological condition[1–3]. It is defined as the presence of pancreatic tissue lacking anatomical and vascular continuity with the pancreas[1]. It occurs most commonly in the stomach, duodenum, and jejunum and has been reported in other locations, including the ileum, Meckel’s diverticulum, colon, gall bladder, umbilicus, fallopian tube, mediastinum, spleen, and liver[2]. The majority of the cases have been found incidentally at laparotomy performed for other abdominal diseases. When an ectopic pancreas is found incidentally during surgery for other abdominal conditions, resection should be considered because of the risk of late clinical problems. This disease occasionally develops symptoms such as bleeding, vomiting or abdominal pain due to pancreatitis[23]. Even if symptoms are present, the preoperative diagnosis of ectopic pancreas in the small bowel appears to be difficult. Malignant transformation can occur in the ectopic pancreas tissue as well as in the tissue of a normally located pancreas. However, the incidence of malignant change in the ectopic pancreas has been estimated to be less than that of the normal pancreas itself[3]. Ectopic pancreas rarely occurs as intestinal invagination leading to ileus in adults[4]. Here, we describe a rare case of small jejunal ectopic pancreas that led to jejunojejunal intussusception and ileus.
CASE REPORT
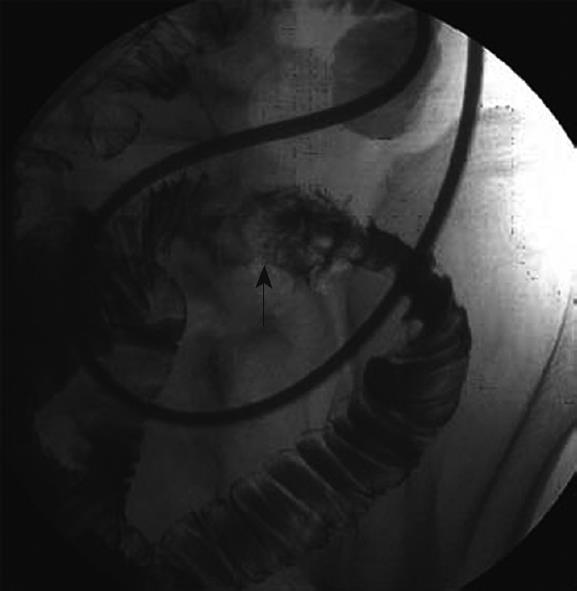
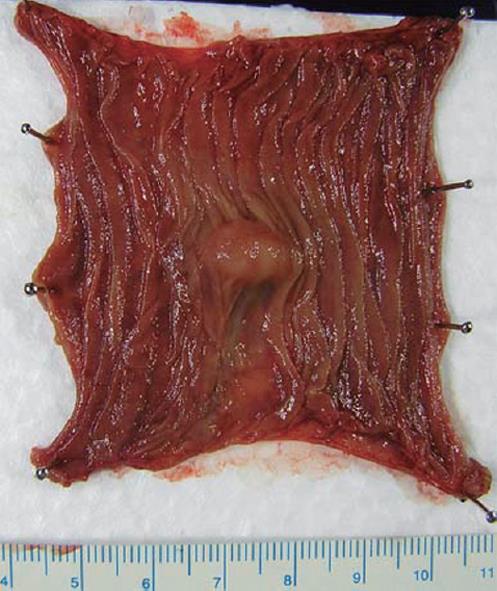
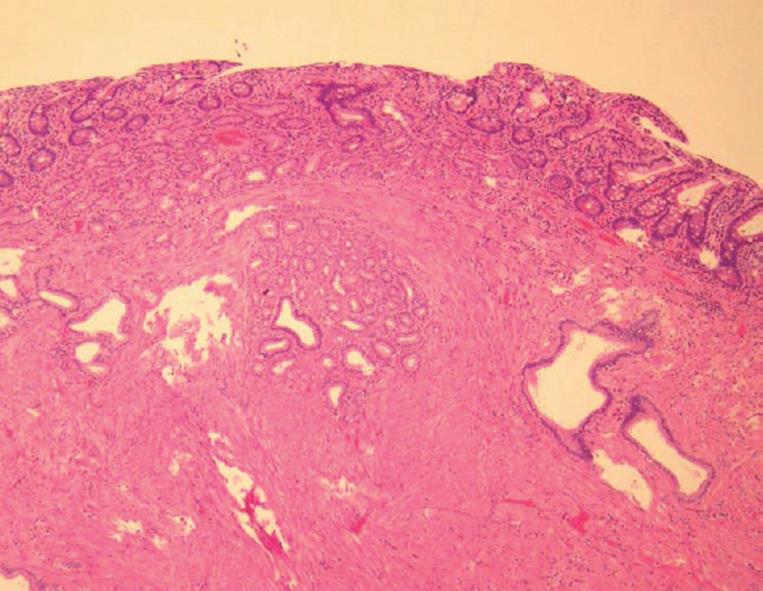
The patient was a 62-year-old Japanese man. He was admitted to our hospital complaining of intermittent abdominal pain of several months’ duration that was increasing in both magnitude and frequency. He had not had previous abdominal surgery and had been in good health. No specific family history was identified. His body temperature was 36.8°C, blood pressure was 132/76 mmHg, and radial pulse rate was 62 beats/min and regular. He had neither anemia nor jaundice. A neurological examination revealed no abnormal findings. Laboratory tests showed hemoglobin concentration of 14.6 g/dL, a red blood cell count of 441 × 104/μL, a white blood cell count of 10 300/μL (normal range: 4000-8000/μL), and a platelet count of 19.5 × 104/μL. Biochemical tests were within normal limits. Plain abdominal radiography showed some intestinal gas and fluid levels. Abdominal CT scan demonstrated a target sign suggesting bowel intussusception and dilated small bowel. Subsequent jejunography using a naso-jejunal tube showed an oval-shaped mass 15 mm in diameter with a smooth surface in the jejunum, which suggested a submucosal tumor (SMT), and edematous mucosa around the mass (Figure 1). Based on these findings, the patient was diagnosed with intussusception due to intestinal SMT. The patient underwent a laparotomy. At laparotomy, a small solid tumor that was 60 cm distal to the Treitz’s ligament was palpable and the small bowel around the tumor was edematous. Liver and spleen were normal. There was no evidence of mesenteric or retroperitoneal lymphadenopathy, ascites or peritoneal disease. The resection of jejunum with 2 cm margins and an end-to-end anastomosis was performed. The resected oval shaped tumor, 14 mm × 11 mm in size, was covered with normal jejunal mucosa and no ulcer or erosion was seen on the mucosal surface (Figure 2). Opening of the rudimentary pancreatic duct was not detected. Histologically, the mass was distributed from submucosa to smooth muscle layer and was composed of proliferating ducts and proliferation of smooth muscle bundles without mitotic figures (Figure 3). However, both exocrine acini and endocrine elements were lacking. Based on the above findings, this tumor was diagnosed as jejunal ectopic pancreas (type III ectopic pancreas according to the classification proposed by von Heinrich[5]). The postoperative course was uneventful. As a result of this treatment, the patient’s abdominal pain resolved postoperatively.
Figure 1 Jejunography using a naso-jejunal tube showed an oval-shaped mass in the jejunum (arrow) and edematous mucosa around the mass.
Figure 2 Macroscopic findings of the tumor.
A 14 mm × 11 mm oval-shaped submucosal tumor covered with normal mucosa was observed.
Figure 3 Histological findings of the tumor.
The localized tumor was composed of proliferating ducts and proliferation of smooth muscle bundles without mitotic figures. However, both exocrine acini and endocrine elements were lacking (HE, × 100).
DISCUSSION
Ectopic pancreas is defined as the presence of pancreatic tissue lacking anatomical and vascular continuity with the pancreas[1]. It occurs most commonly in the stomach, duodenum, and jejunum and has been reported in other locations, including the ileum, Meckel’s diverticulum, colon, gall bladder, umbilicus, fallopian tube, mediastinum, spleen, and liver[2]. Ectopic pancreas occurs in 0.25%-13.7% of patients based on both autopsy and surgical series; approximately 70% of all such tissues are found in the stomach, duodenum, and jejunum[2]. When an ectopic pancreas is found coincidentally during surgery for other abdominal conditions, resection should be considered because of the risk of late clinical problems. Although this disease occasionally develops symptoms such as bleeding, vomiting or abdominal pain due to pancreatitis[2367], intestinal obstruction or intussusception is rare[489]. No invagination case caused by ectopic pancreas had been observed in a series of 53 invaginations, reported by Ong et al[10]. Ectopic pancreas in the small intestine may rarely be fatal: however, Hitosugi et al[11] reported a sudden death case (11-year-old Japanese female) caused by intestinal obstruction due to jejunal ectopic pancreas (about 4 cm in diameter). Adult intussusception represents 5% of all cases of intussusception and accounts for only 1%-5% of intestinal obstructions in adults[12]. In contrast with intussusception in children, nearly all adult cases have primary causes such as a polyp, an SMT or a malignant tumor that needs to be resected[1314]. In the present case, the small SMT (ectopic pancreas) in the jejunum caused ileus due to intussusception.
The preoperative diagnosis of ectopic pancreas in the small bowel appears to be difficult. However, there are some recent reports describing ectopic pancreas in the small bowel discovered by double-balloon enteroscopy or capsule endoscopy[15–17]. In spite of using double-balloon enteroscopy, endoscopic diagnosis is rarely conclusive on endoscopic biopsies because the lesion locates mainly in the submucosal layer and the biopsy is often not deep enough to reach the submucosal tumor tissue. In the present case, the diagnosis could not be confirmed preoperatively although we knew that bowel intussusception due to small SMT might cause ileus. Because of the suspicion of ileus due to jejunal tumor, the patient underwent laparotomy; thus, double-balloon enteroscopy was not performed in the present case.
This disease is treated in principle by surgical resection if bowel intussusception or ileus occurs[4]. Moreover, physicians should be aware that ectopic pancreas in the small bowel may associate with endocrine tumor or carcinoma[18–21]. However, ectopic pancreas in the small intestine is usually benign. Ectopic pancreas in the small intestine is rarely fatal and patients remain asymptomatic in their daily lives, except for when bleeding, bowel intussusception, obstruction or pancreatitis occurs. Therefore, it is likely that there are patients with latent small bowel ectopic pancreas which may be incidentally discovered in the future, as a result of advances in diagnostic imaging, such as improved CT, MRI, capsule endoscopy and double-balloon enteroscopy.
In conclusion, we have reported a very rare case of jejunal ectopic pancreas that led to jejunojejunal intussusception. Thus, it is necessary to be aware that a jejunal ectopic pancreas may cause jejunojejunal intussusception even though the likelihood is small. This etiology should be suspected in a patient with chronic atypical abdominal pain.