Published online Jul 14, 2009. doi: 10.3748/wjg.15.3309
Revised: June 9, 2009
Accepted: June 16, 2009
Published online: July 14, 2009
Echinococcosis is a cyclozoonosis characterized by cystic lesions usually situated inside or outside the liver. We discuss the case of a 77-year-old woman with a recurrent hydatidosis with a cyst arising from the liver, growing through the lateral right abdomen wall, and reaching the subcutaneous tissue of the lumbar region. In the literature, rare subcutaneous or muscular localizations of hydatid cysts are described, however, there is no mention of a cyst growing over the abdominal wall muscles, shaped like an hourglass, partially in the liver and partially in the subcutaneous tissue, as in our case. We have not found any pathogenetic explanation for this growth pattern which is not typical of the biological behaviour of a hydatid cyst.
- Citation: Di Cataldo A, Latino R, Cocuzza A, Li Destri G. Unexplainable development of a hydatid cyst. World J Gastroenterol 2009; 15(26): 3309-3311
- URL: https://www.wjgnet.com/1007-9327/full/v15/i26/3309.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.3309
Hydatid disease is a cyclozoonosis caused by Echinococcus granulosus or Echinococcus multilocularis, and is characterized by cystic lesions usually situated in the liver. These lesions can be asymptomatic for a long time, or cause an ache, however, there are no specific local or general symptoms and signs are related to size, location or complications of the cyst. The case of recurrent hydatidosis in a 77-year-old woman is discussed where the cyst, probably arising from the liver, grew through the lateral right abdomen wall and reached the subcutaneous tissue of the lumbar region.
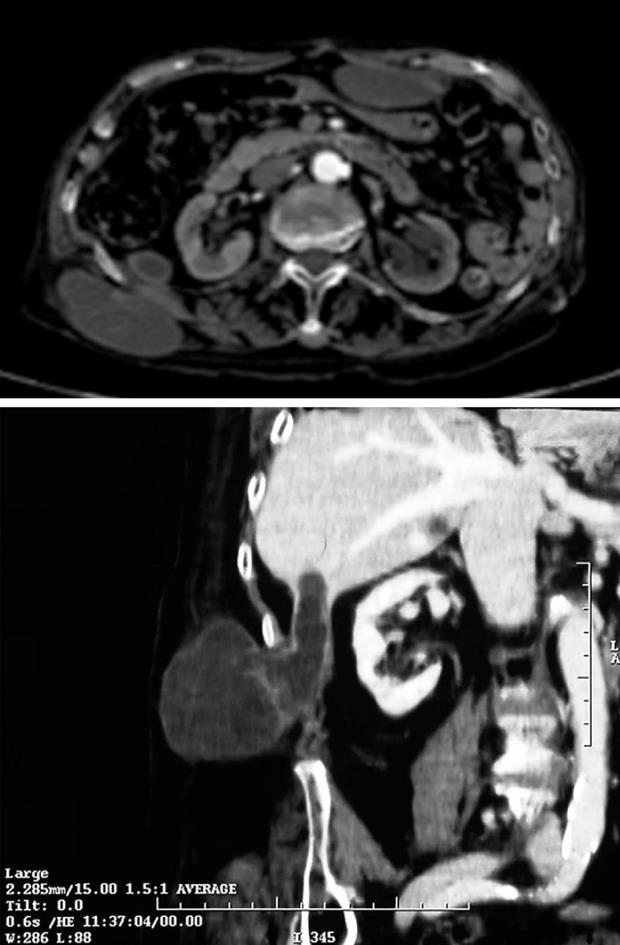
A 77-year-old woman was evaluated due to of the growth of an aching mass in the right lumbar region. Three years previously surgery was performed for hydatidosis of the mesentery. Objective examination revealed a painful swelling mass in the right lumbar region about 7-8 cm in diameter and mobile with respect to the upper and lower layers, which had distinct margins and a smooth surface (Figure 1). On palpating the abdomen the patient had pain in the right upper abdominal quadrant. CT of the abdomen showed a voluminous low-density mass (74 cm × 58 mm) in the low-external side of the VI liver segment. The mass was pedunculated, growing over the right posterior abdominal wall muscles and reaching the subcutaneous tissues (Figure 2).
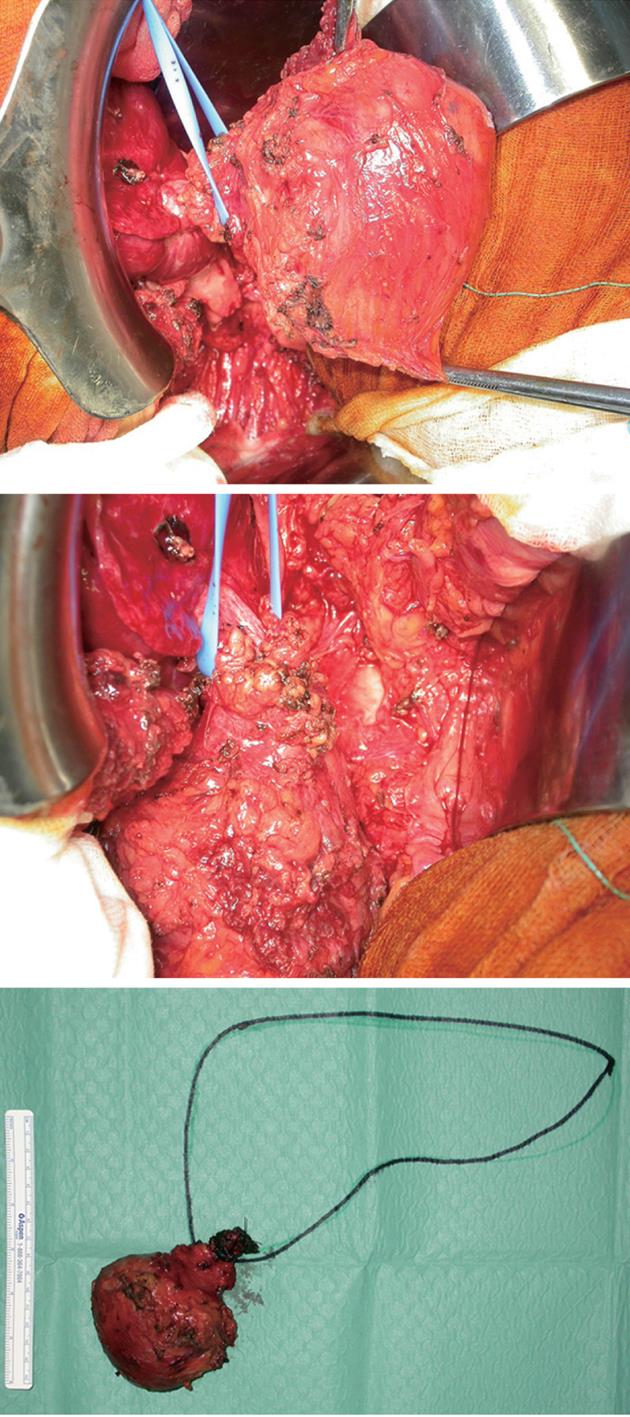
Surgical treatment confirmed that the voluminous cyst was connected to the VI liver segment by a peduncle. Growing sideways and then behind, this mass reached the muscular layer arriving at the subcutaneous tissue of the right lumbar region. The mass was removed from the perihepatic side of the peduncle, 2-3 cm inside the liver, and from the abdominal external oblique muscle and the latissimus dorsi up to the subcutaneous tissue of the lumbar region (Figure 3). The post-operative period was problem-free, and the patient was discharged after 1 wk on anti-helminthic therapy. Histology confirmed the suspicion of hydatid cyst.
Hydatid disease is caused by Echinococcus granulosus, an endemic infection in several mediterranean countries, or by Echinococcus multilocularis. Hydatid cysts can be observed in all parts of the body, but are more frequent in the liver (50%-70%), lung (20%), and spleen (5%-8%)[1], while rare localizations are the kidneys, adrenal glands[2], spleen, soft tissues and brain[3].
Echinococcosis may be asymptomatic, detected only when imaging scans of the liver are carried out for different reasons, but it may cause pain or lead to complications. Cysts can rupture into the peritoneum, resulting in anaphylaxis or peritonitis[4], or into the biliary tract, causing cholangitis or cholestasis, and into the bronchi, causing bronchial fistula, or the cysts may become infected and form liver abscesses. Compression of the bile duct, portal vein, and hepatic veins can cause cholestasis, portal hypertension, and Budd-Chiari syndrome, respectively[5].
The diagnosis of hydatid cysts relies on epidemiologic data (geographical location and profession) clinical manifestations, serologic tests and radiologic imaging.
The treatment of choice is surgery. Chemotherapy (albendazole and mebendazole) is currently indicated in patients who cannot undergo major operations or for the prevention of secondary echinococcosis after surgery[6], but is contraindicated for large, superficially situated, or infected cysts, which are prone to rupture[78].
Our case shows some particular features that deserve closer examination. Usually the hydatid cyst grows in the liver in every direction, both inside the hepatic parenchyma and outside towards the peritoneal cavity. In our case, the cyst was connected to the liver by a peduncle 3-4 cm inside the liver. The surgeon who operated on our patient three years previously informed us of two hydatid cysts (diameter 9 cm and 12 cm) located in the mesocolon, which were connected by a peduncle, making it easy to remove them without spreading the disease. The hypothesis that the cyst we treated could have been a secondary echinococcosis due to spillage of cystic fluid and seeding during the first operation[5] has been denied. In the literature, rare subcutaneous or muscular localizations of hydatid cysts have been described[9], however, a cyst growing over the abdominal wall muscles, shaped like an hourglass, partially in the liver and partially in the subcutaneous tissue, as in our case has never been described. This growth pattern is not typical of the biological behaviour of a “benign tumor” such as a hydatid cyst, and seems to be more similar to the behaviour of an infiltrating malignant neoplasm. The only plausible explanation is that it could be related to seeding during the first surgery through drainage, however, the only drainage after the first surgery was located in the right lower abdominal quadrant, far away from the lumbar localization of the cyst we treated.
In the literature, Parmar et al[10] reported a case showing some similarities to our patient: a hepatic hydatid cyst which had ruptured into the subcutaneous tissue of the anterior abdominal wall. While the superficial and subcutaneous localization of the mass was similar, its connection with the right lobe of the liver was different. In Parmar’s case the right lobe of the liver was almost entirely occupied by the cyst, in our case the cyst was connected only by a peduncle. Parmar did not suggest any pathogenetic explanation, but just describes the kind of rupture that can involve a hydatid cyst.
In conclusion, we have not found any evidence in the literature for a pathogenetic explanation for the growth of the hydatid cyst over the abdominal wall muscles, shaped like an hourglass, partially in the liver and partially in the subcutaneous tissue. A similar growth pattern may occur in cysts found in the liver cupola where they can damage the diaphragm through inflammatory processes. The cysts then grow towards the pleural opening to the bronchial tubes, resulting in an uncommon and severe complication, a hydatid bronchobiliary fistula. In this situation the pathogenetic mechanism is clearly caused by the infective process resulting in adhesions in the diaphragm. In our case no infective process was present, the cyst was connected to the liver by a peduncle which was easily removed from the transverse colon and from the muscles.
| 1. | Iuliano L, Gurgo A, Polettini E, Gualdi G, De Marzio P. Musculoskeletal and adipose tissue hydatidosis based on the iatrogenic spreading of cystic fluid during surgery: report of a case. Surg Today. 2000;30:947-949. |
| 2. | Di Cataldo A, Trombatore G, Greco R, Lanteri R, Li Destri G, Licata A. Hydatid disease in a very unusual location: the adrenal gland. A case report. Chir Ital. 2003;55:275-278. |
| 3. | Cöl C, Cöl M, Lafçi H. Unusual localizations of hydatid disease. Acta Med Austriaca. 2003;30:61-64. |
| 4. | Di Cataldo A, Lanteri R, Caniglia S, Santangelo M, Occhipinti R, Li Destri G. A rare complication of the hepatic hydatid cyst: intraperitoneal perforation without anaphylaxis. Int Surg. 2005;90:42-44. |
| 5. | Gourgiotis S, Stratopoulos C, Moustafellos P, Dimopoulos N, Papaxoinis G, Vougas V, Hadjiyannakis E. Surgical techniques and treatment for hepatic hydatid cysts. Surg Today. 2007;37:389-395. |
| 6. | Filippou D, Tselepis D, Filippou G, Papadopoulos V. Advances in liver echinococcosis: diagnosis and treatment. Clin Gastroenterol Hepatol. 2007;5:152-159. |
| 7. | Bekhti A, Schaaps JP, Capron M, Dessaint JP, Santoro F, Capron A. Treatment of hepatic hydatid disease with mebedazole: preliminary results in four cases. Br Med J. 1977;2:1047-1051. |
| 9. | Latino R, Costa S, Barbagallo E, Virzì A, Vagnoni G. [Primary localization of a hydatid cyst in the major dorsal muscle: report of a case]. Ann Ital Chir. 1999;70:123-126; discussion 126-127. |
| 10. | Parmar H, Nagarajan G, Supe A. Subcutaneous rupture of hepatic hydatid cyst. Scand J Infect Dis. 2001;33:870-872. |