INTRODUCTION
Magnetic resonance cholangiopancreatography (MRCP) is a relatively new imaging technique developed for the diagnosis of patients with pancreaticobiliary disease. The signal of structures filled with static or slowly moving fluid, such as the bile and pancreatic ducts, is greatly increased on T2-weighted images, resulting in an increased duct-to-background contrast. Recent studies have shown that MRCP is as useful as endoscopic retrograde cholangiopancreatography (ERCP) regarding the diagnosis of extrahepatic bile duct and pancreatic duct abnormalities such as common bile duct stones[1–4], malignant obstruction of the bile and pancreatic ducts[125], congenital anomalies[167], and chronic pancreatitis[8–10]. In some institutions, MRCP is becoming the first-choice technique for imaging the biliary system, with ERCP being reserved for therapeutic indications. In recent studies, MRCP showed extremely high performance in visualizing bile duct stones with both a sensitivity and a specificity of 90% or higher in most cases[11–17]. In the false negative cases, all stones were as small as 3-5 mm and were present near the duodenal papilla. Thus, MRCP is very useful for the diagnosis of bile duct stones and the determination of a therapeutic strategy. Since ERCP involves the risk of complications such as acute pancreatitis[18–21], it should be performed only when absolutely necessary. In some patients clinically suspected of choledocholithiasis, ERCP shows a cleavage at the duodenal papilla, but does not detect the stones in the common bile duct. These findings suggested that stones in the common bile duct had probably passed spontaneously. In fact, it was reported that three-fourths of common bile duct stones passed spontaneously before cholecystectomy[22], indicating that many patients with bile duct stones may not need ERCP. There are reports on the clinical course of patients suspected of spontaneous passage of bile duct stones after MRCP alone[2324]. However, since ERCP was not performed, it was not clear whether the stones were actually present. Presence of bile duct stones could cause acute cholangitis, which, if aggravated, may be fatal. Consequently, we investigated the usefulness of MRCP and the need for diagnostic ERCP in patients suspected of spontaneous passage of stones.
MATERIALS AND METHODS
From April 2007 to January 2009, 36 patients suspected of spontaneous passage of bile duct stones were prospectively evaluated. There were 26 men and 10 women and the mean age of the patients was 62.1 years (range: 33-82 years). The mean observation period was 6.7 mo (1-9 mo). After blood sampling the patients were subjected to ultrasound examination (Power Vision 6000; TOSHIBA Tochigi Japan) to assess the presence of stones in the gallbladder and common bile duct. The patients had gallbladder stones and were clinically suspected of spontaneous passage because they presented with clinical symptoms that included abdominal pain and fever, and showed signs of inflammatory reaction as well as a marked rise of hepatobiliary enzymes. These symptoms resolved and patients showed normalized values of blood biochemical parameters after conservative treatment, without evidence of stones in the common bile duct on MRCP. Patients who had originally had intrahepatic cholestasis were considered as “improved” if the level of hepatobiliary enzymes had normalized. The US, MRCP and ERCP images of typical cases are shown in Figures 1,2,3, respectively.
Figure 1 A 56-year-old man.
Several gallbladder stones measuring about 5-10 mm were detected by abdominal ultrasonography.
Figure 2 No translucency indicative of stones in the bile duct was shown by magnetic resonance cholangiopancreatography.
Figure 3 No translucency indicative of stones in the bile duct was shown by endoscopic retrograde cholangiopancreatography (A).
After withdrawal of the fiber, the posture was changed and the bile duct was imaged again. However, no translucency was observed (B).
In this study, the need for urgent drainage was assessed first. Accordingly, blood was collected from the patients on arrival at the hospital for the assessment of acute cholangitis. Patients with moderate to severe acute cholangitis[25] that did not respond to the initial medical treatment, were excluded from this study and were subjected to emergency ERCP with biliary drainage. When a patient presented symptoms of acute cholangitis during follow-up, ERCP was conducted provided the patient had given his/her informed consent prior to the examination. Patients with symptoms of acute pancreatitis were excluded from this study. Even if a marked increase in hepatobiliary enzymes was detected before arrival at the hospital, we waited for an improvement in clinical symptoms and blood test values if cholangitis was mild, before performing MRCP followed by ERCP.
MRCP was performed using a 1.5T GE CV/I scanner and a phased-array torso coil (General Electric Medical Systems, Milwaukee, WI). The radiographic conditions were as follows: thin-section MRCP images were obtained in the coronal plane using half Fourier single-shot fast spin echo (SSFSE) imaging at a slice thickness of 4.0 mm, 34FOV, 256 × 256 matrix, and a TE of 180. Thick-slab SSFSE MRCP images were obtained in the plane using a matrix of 256X256 and a maximum TE. Imaging in the coronal and axial planes was done using a fast 3D spoiled gradient echo sequence with a TR of 3.9 TE minutes, 2.4 mm slice thickness (interpolated to 1.2 mm), and a 256 × 192 matrix. Images were reviewed on an Advantage Windows workstation (General Electric Medical Systems) that allowed 3D reconstruction. MRCP images were read after evaluating clinical symptoms and hematological findings to examine the common bile duct for the presence of stones. First, a radiologist with more than 20 years of experience examined the MRCP images and if there were no bile duct stones, the same MRCP images were subsequently examined by a gastroenterologist with more than 15 years of experience. Only after the absence of stones was confirmed by these 2 specialists, was the case defined as spontaneous passage of stones. MRCP was conducted after the clinical symptoms and blood test findings had sufficiently improved. ERCP was conducted within 4 d of MRCP to check for the presence of stones. ERCP images were read only by the gastroenterologist who had examined the MRCP images. As a measure against complications, the duration of ERCP was strictly limited to within 15 min. This prospective study was conducted after obtaining informed consent from the patients. Furthermore, the protocol of this study was discussed and approved by the Institutional Review Board of Funabashi Central Hospital.
RESULTS
ERCP was successfully conducted in all 36 patients after MRCP confirmed the absence of stones in each of them. The ERCP procedure was completed within 15 min in all these cases. Mild acute pancreatitis, assessed according to Cotton’s criteria[21], occurred as a complication after ERCP in 1 (2.8%) of the 36 patients. Cannulation was difficult in this patient and pancreatitis was assumed to be caused by pancreatography, which was performed 3 times during ERCP. However, remission was attained after conservative treatment. No other complications occurred. Both the radiologist and the gastroenterologist who read MRCP images ruled out the presence of bile duct stones in the 36 patients (K = 1.0) (Figures 2 and 3).
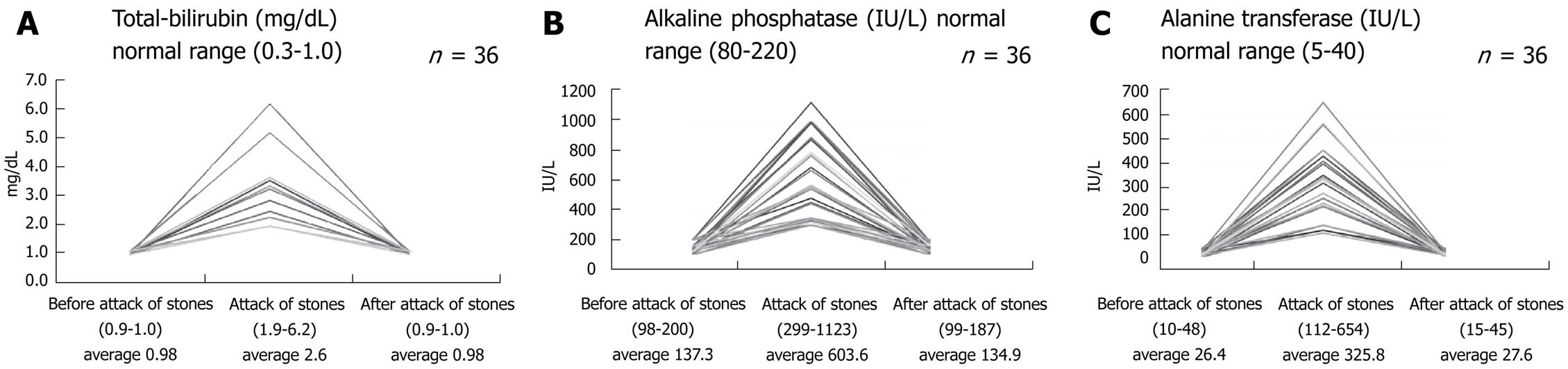
MRCP showed the bile duct had a mean diameter of 6.6 mm (range, 4.8-8.3 mm). Biochemical average (and range) data were total bilirubin 2.6 (1.9-6.2) mg/dL (Figure 4A), alkaline phosphatase (ALP) 603.6 (299-1123) IU/L (Figure 4B), and alanine transferase (ALT) 325.8 (112-654) IU/L (Figure 4C) at the time of common bile duct obstruction while the normal range values were total bilirubin 0.3-1.0 g/dL; ALP 80-220 IU/L and ALT 5-40 IU/L. Subsequently, 6 patients underwent cholecystectomy. During the observation period, none of the 36 patients experienced a second spontaneous passage of stones. At the time of registration for this study, the clinical symptoms of 6 patients suspected of spontaneous passage of stones were already showing a tendency towards remission. Yet these patients were not registered for the study because they had moderate cholangitis. Accordingly, urgent ERCP was conducted without MRCP. The result indicated no bile duct stone in any of the 6 cases.
Figure 4 Changes in serum.
A: Total-bilirubin; B: Alkaline phosphatase; C: Alanine transferase.
DISCUSSION
MRCP can detect bile duct stones with a high rate of accuracy and sensitivity. In the present study, ERCP detected no stones in any of the patients suspected of spontaneous passage of stones and confirmed by the MRCP conducted after the clinical symptoms had improved and blood test values had normalized or returned to baseline levels. Nevertheless, the possible presence of small stones undetectable by ERCP cannot be denied. Intraductal ultrasonography (IDUS), which can be used following ERCP, is a valuable tool for the imaging of tiny stones. IDUS is likely to detect very small bile duct stones more accurately than ERCP alone[26]. Bile duct stones have, however, been reported to pass spontaneously in most cases[22]. Although the aggressive use of IDUS may increase the detection of bile duct stones, prolonged ERCP practice may result in accidental events. Thus, this procedure was not included in the study design.
The presence or absence of small stones is a matter of controversy. However, it is basically reasonable to assume a spontaneous passage of stones if MRCP has detected no stones in the patients whose clinical symptoms improved and whose blood test values normalized or returned to the baseline levels. Today, most reports conclude that MRCP is comparable to ERCP in the diagnosis of biliary stones. Institutions with high-magnetic-field MRI make it a rule not to perform diagnostic ERCP in patients who have no stones identified by MRCP. The possibility that the present study would be useful in considering indications for use of ERCP was suggested. The results of this study indicate the feasibility of diagnosis of spontaneous passage of stones in the common bile duct based on clinical symptoms, blood biochemistry, US, and MRCP without exposure to X-ray, thus reducing such exposure for medical personnel responsible for conducting ERCP[27], and avoiding the potential complications of ERCP.
US is a simple examination tool for imaging bile duct stones but is less satisfactory for the detection of stones[26]. However, it provides information on the gallbladder and important information on the diameter of the bile duct considering the presence of bile duct stones and thus it is a very useful examination. Given the higher performance of MRCP, diagnosis employing US or MRCP rather than diagnostic imaging will become more common when bile duct stones are suspected. However, the patients with spontaneous passage of stones included in this study presented with mild cholangitis. In patients with moderate or severe cholangitis, drainage of the biliary tract that allows the detection of stones more rapidly than MRCP, may prove very useful[25]. When clinical symptoms improve, blood biochemical parameters have normalized, and MRCP shows there are no stones in the common bile duct, it can be considered that the stone has spontaneously passed and thus ERCP would not be necessary.
COMMENTS
Background
Magnetic resonance cholangiopancreatography (MRCP) is a relatively new imaging technique developed for the diagnosis of patients with pancreaticobiliary disease. Recent studies have shown that MRCP is as useful as endoscopic retrograde cholangiopancreatography (ERCP) for the diagnosis of extrahepatic bile duct and pancreatic duct abnormalities such as common bile duct stones.
Innovations and breakthroughs
When clinical symptoms improve, blood biochemical parameters have normalized, and MRCP shows there are no stones in the common bile duct, it can be considered the stone has spontaneously passed and thus ERCP would not be necessary.
Peer review
This is a prospective, non-controlled study from a single center. The observation is made that ERCP is not helpful when a passed stone is suspected and MRCP is negative.
Peer reviewer: Peter L Moses, MD, FACG, AGAF, Professor, University of Vermont College of Medicine Section of Gastroenterology & Hepatology, 111 Colchester Avenue, Smith 237B, MCHV, Burlington, VT 05401, United States
S- Editor Tian L L- Editor O’Neill M E- Editor Yin DH