Published online Jan 14, 2009. doi: 10.3748/wjg.15.144
Revised: November 18, 2008
Accepted: November 25, 2008
Published online: January 14, 2009
The role of the oesophago-gastric junction (OGJ) in gastro-oesophageal reflux disease is still not completely understood, and there is no clinically used method to assess the OGJ function in patients. Only indirect methods such as pH studies are carried out. The OGJ acts a valve controlling the flow of solids, liquids and gases between the oesophagus and the stomach. Manometry can determine if a sphincter is toned or relaxed; but, it cannot confirm that the sphincter region is actually open. Distension is a new technique for measuring function in the OGJ. By measuring the cross-sectional area through the narrow region in the junction during distension of a catheter mounted bag, much more information on the opening and closing patterns of the junction can be determined. This technique has already been demonstrated to show changes in the OGJ after surgical treatments for reflux disease. New measurement ideas around the concept of distending the OGJ offer new hope that a clinically useable test for compliance at the junction can be developed and could potentially help in determining appropriate therapy.
- Citation: McMahon BP, Jobe BA, Pandolfino JE, Gregersen H. Do we really understand the role of the oesophagogastric junction in disease? World J Gastroenterol 2009; 15(2): 144-150
- URL: https://www.wjgnet.com/1007-9327/full/v15/i2/144.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.144
If you ask many clinicians, even those specialising in gastroenterology, what is the mechanism between the oesophagus and stomach which prevents the backflow of stomach contents into the oesophagus? Their instinctive reply will be the lower oesophageal sphincter (LOS). While the LOS certainly contributes to the mechanism it is not the sole effecter. Many common definitions of the mechanism have not even been updated. Medlineplus© defines gastroesophageal reflux disease as “backward flow of the gastric contents into the oesophagus due to improper functioning of a sphincter at the lower end of the oesophagus and resulting especially in heartburn[1]”. The more clinical definition agreed at the Montreal Consensus does not make any mention of the relevance of the LES; “GORD is a condition which develops when reflux of stomach contents causes troublesome symptoms and/or complications”. A definition very much based on effect rather than cause[2].
Of course with a little reading, most of us will know that the barrier at the oesophago-gastric junction (OGJ) is rather complex with a number of mechanisms impinging on it. Mittal and Balaban’s New England Journal of Medicine article from 1997 highlights the fact that the lower end of the oesophagus is guarded by an intrinsic smooth muscle called the lower oesophageal sphincter, an extrinsic skeletal muscle called the crural diaphragm, the intra-abdominal location of the LOS, integrity of the phrenoesophageal ligament, and maintenance of the acute angle of His promoting a “flap valve” function[3–5]. It has also been concluded that this structure is very sophisticated in the neurophysiologic control of opening, and its anatomical configuration, and with respect to dynamic changes in forces from active and passive muscle structures in this region of the body.
Gastro-oesophageal reflux disease (GORD) is one of the most common diseases in Western Civilisation. GORD can progress to severe complications if untreated. It is a highly prevalent disorder and affects 10%-20% of Western populations[6]. GORD originates from a disturbance in the structure and function of the LOS barrier. Anatomical or structural abnormalities occur often in the presence of a hiatal hernia and physiological predispositions from abnormal motor function of the LOS and oesophageal body. Dysfunctional oesophageal motility coupled with a weak LOS can cause uncoordinated propulsion of food, regurgitation of food and acid into the oesophagus, particularly after meals, and in the horizontal position, an inadequate acid/bile clearance from the oesophagus.
Achalasia is a motor disorder of the oesophagus characterized by loss of oesophageal peristalsis and failure of the LOS to relax completely upon deglutition. There is a poor correlation between higher sphincter pressures, oesophageal emptying and achalasia symptoms in general[7]. The origin of achalasia is still poorly understood. There is evidence to implicate familial, autoimmune, infectious or environmental causes. Currently, it is not possible to determine how the OGJ or the sphincter function changes as the disease develops.
By far the most common OGJ disorder is GORD. For most people, GORD is diagnosed by symptoms usually at a visit to their general physician or community doctor. However, for many people, pharmaceutical treatment of GORD does not completely eradicate their symptoms, and they must be referred to a gastroenterologist for further evaluation and treatment. Usually, the first test a gastroenterologist will carry out is an upper gastrointestinal endoscopy. This visual test will quickly identify the presence of any erosive disease in the region of the OGJ, and if there are visible signs of this erosion or Barrett’s metaplasia.
These referrals may also undergo other tests if endoscopy is negative. Traditionally, this involved oesophageal manometry to evaluate peristalsis and to confirm sphincter position and activity. This is followed by a 24 h pH study using a catheter based system that can incorporate impedance monitoring or a catheter-free telemetry-type system. Intraluminal impedance is increasingly being used to determine whether non-acid reflux may play a role in patients with PPI-resistant reflux symptoms, chronic unexplained cough, excessive belching, and rumination[8].
Despite the important role the OGJ plays in reflux disease, apart from standard manometry[9], techniques have not focused on objectively measuring its function.
Even with a number of new tests for reflux disease, it is still difficult to determine the actual role of the OGJ in this disease. Of course, the only test which directly measures some aspects of the junction is manometry, and this has been shown, for some time now, not to be a reliable predictor of GERD on its own[10]. There has been little emphasis on assessing the mechanical properties of OGJ opening, and little is known about the dynamics of retrograde flow across the OGJ. Thus, it is time to revisit this and look at new evidence.
If the OGJ has a role in digestive disease, and if none of the parameters we use to determine the severity of a patient’s reflux disease relate to any direct objective and quantitative parameter or parameters, do we really have the complete picture? Should more research not be carried out into methods to determine the role of the OGJ in disease? If pH studies determine that there is too much acid refluxing into the oesophagus, can we always be confident that this is due to dysfunction of the LOS? Could it be some other mechanism in the process of digestion, such as peristaltic dysfunction and poor oesophageal acid clearance which is malfunctioning and causing the disease?
If we accept that the main action or combined actions at the OGJ is to narrow and close the junction between the stomach and the oesophagus, then we must accept that it works in a similar way to a valve. The medical dictionary defines a valve as “a bodily structure that closes temporarily a passage or orifice or permits movement of fluid in one direction only” (Merriam-Webster Online Dictionary copyright© 2005 by Merriam-Webster, Incorporated). In the context of the OGJ, this definition is quite limiting, and I prefer the more general web definition of “A valve is a device that regulates the flow of substances (either gases, fluidized solids, slurries, or liquids) by opening, closing, or partially obstructing various passageways[11]”. The OGJ function is probably better described in this way. It is as much a control valve as an “on” and “off” valve. While food boluses and liquids travel antegrade, air and on occasion small amounts of stomach contents must travel retrograde back up the oesophagus for venting purposes.
This, in effect, can be a difficult question. In engineering, we can easily measure the performance of an on/off valve by checking it visually. If the open valve condition is created, it is usually possible to observe flow through the valve. In the closed valve condition, it can normally be inspected for leaks or other forms of dysfunction. If the valve controls flow rather than shutting off completely, then normally there will be a device included to determine the flow.
Obviously the situation is much different in the OGJ. Much of the anatomical structure in the region is soft tissue. This does not image well radiologically, although historically barium studies have given a good, but subjective indication of flow during swallowing. The OGJ tends to be very dynamic, and so does not image well using magnetic resonance. In addition, the image resolution of current MR technology and CT is of insufficient quality to be satisfactory.
Historically, the LOS has been evaluated using manometry which uses pressures measured at precise points on a luminal catheter to determine the forces applied by the squeezing or pushing of the sphincteric regions in luminal organs. Manometry has evolved into a very sophisticated procedure for determining pressure changes in luminal organs during motility, but it is no longer recommended for the diagnosis of reflux disease[10].
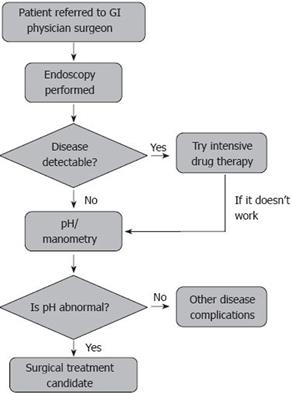
The flow diagram in Figure 1 outlines the pathway for a patient with gastro-oesophageal reflux disease. In up to 20% of cases, there can be a negative or non-optimal response to drug therapies such as PPIs or H2 blockers. These patients are usually referred to a gastroenterologist or in some cases directly to a GI surgeon where the severity of their condition is evaluated.
Referred patients will most often undergo an upper GI endoscopy so that erosive signs of the disease or Barrett’s metaplasia can be excluded. However, up to 80% of patients will have a normal endoscopy, and will be referred for oesophageal function testing[12]. Most of these patients will undergo pH and manometry studies. Manometry can be utilized to document landmarks for placement of the pH electrode. The older manometry method is to perform a catheter pull-through study which will identify the respiratory inversion point and establish the high pressure zone at the LOS. This would also then indicate the position of the z-line and determine the position of the 24 h pH catheter, usually 6 cm above the z-line or 5 cm above the proximal margin of the LOS. The 24 h pH study is then used to determine the total time the pH < 4 or a composite score of oesophageal acid exposure. The DeMeester score uses 6 parameters (supine reflux, upright reflux, total reflux, number of episodes, number of episodes longer than 5 min, and the longest episode) to calculate a score which indicates the severity of reflux.
Newer methods for determining oesophageal function include high-resolution manometry (HRM), intraluminal impedance and wireless pH measurement. HRM is a method which uses sensors at 12 radial orientations and 36 longitudinal positions (1 cm intervals). In effect, this sophisticated probe can monitor the dynamic activity throughout the oesophagus from above the upper oesophageal sphincter to below the LES. Recent clinical evaluation has shown two major strengths of pressure topography plots compared with conventional manometric recordings. These strengths are the ability to (1) delineate the spatial limits, vigor, and integrity of individual contractile segments along the oesophagus and (2) to distinguish between loci of compartmentalized intra-oesophageal pressurization and rapidly propagated contractions[13].
In terms of reflux monitoring, the main advantage of the wireless pH system is the ability to attach a capsule to the inner mucosal surface of the oesophagus, thus negating the need to run an uncomfortable catheter through the patient’s nasal passage[14].
The recent development of intra-luminal impedance as a measurement technique has added another option to the clinician’s diagnostic armoury. This technique has been shown by numerous studies to be a sensitive and reliable means of detecting fluid or gas movement within the oesophagus. Hence it is a useful tool for determining the presence and extent of acid and non-acid gastro-oesophageal reflux, but not the quantity[15–17]. Despite these sophisticated tests none can measure the objective role of the valvular effect at the OGJ in oesophageal disease.
Since the work of Ingelfinger, Code and Fyke in the 1950s, most of the evidence which identifies the OGJ as the prime suspect in reflux disease has been based on manometric studies[1819].
From the basic pull-through techniques to the development of the sleeve sensor, manometry has been used to describe sphincteric action at the junction. However, all the evidence in recent years suggests that it is not the ideal measurement technique. Recently, the AGA has advised that manometry should not be used to verify the presence of reflux disease. Yet, it is often still used as a technique in research studies[1020–22].
A manometer is actually an instrument designed for measuring gas pressure. We should also remember from physics that pressure is a measure of force per unit area. Oesophageal manometry is often incorrectly defined as the degree of pressure exerted by the muscles of the oesophageal wall. The less specific definition of manometry as a method of recording pressures within the oesophagus is probably more appropriate. Strictly speaking muscles do not exert a pressure, they exert a force or rather forces in several directions. It could be argued that a manometric system cannot measure these forces; however, what it can do is use pressure as a rough proxy.
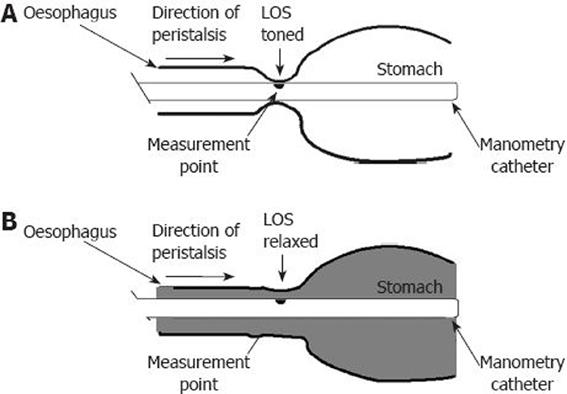
Consider the case of a manometry sensor on a catheter type probe suitable for inserting into luminal organs such as the oesophagus. Whether it is a water perfusion 4 port catheter or a state-of-the-art 36 position, 12 radial sensor measuring high resolution manometry catheter, the sensing principle is the same. Figure 2 indicates how this concept of measuring pressure may be limiting. In Figure 2A, we can see the manometry catheter with the black dot on the catheter indicating the measurement point. This point represents a sensor on any manometry catheter. When a normal LOS is toned or competent, it exerts a squeeze or force on the sensor causing it to be engulfed or occluded by the sphincter. Hence, the pressure measured provides a reasonable representation of the force in the tightened sphincter. However, if the sphincter is relaxed, as demonstrated in Figure 2B, then rather than the lack of squeeze or force present being represented by no or low pressure at the sensor, the pressure here is more indicative of the state of the chamber created by the lumen opening up between the oesophagus and swallowing. Hence, the pressure observed at the measurement point is the force over a large area indicated by the shading in the diagram. We can conclude from this, when making manometric measurements in the LOS, that when the sphincter is in the toned state, we are actually measuring under a different set of parameters than when it is relaxed or not exerting a force on the pressure measuring sensor point. The measurement being made during swallowing is also altered by the peristaltic wavefront creating a bolus pressure that is pushing through the relaxed OGJ- highlighted bolus flow pressure and elastic properties of the OGJ.
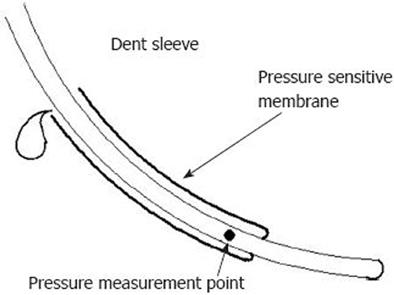
One of the biggest developments in manometry was the introduction of the sleeve sensor in 1976[23]. Difficulties with reliable monitoring of maximal sphincter pressure with perfused side holes led to development of the Dent sleeve (Figure 3). The Dent sleeve recognized that, because of continuous movement within the lumen of the recording catheter and the narrowness of the region in the sphincter at peak pressure, it is impossible to guarantee that you are measuring the peak pressure continuously with a normal point measurement catheter. The sensing function of the sleeve ensures that it records maximal sphincter pressure, regardless of where the sphincter is positioned along the sleeve length. These unique recording properties make the sleeve the only sensor that can monitor sphincter pressure reliably using a static probe. However, new high-resolution manometry catheters are not limited by this movement artifact. The pressure drop measured by the Dent sleeve or high-resolution manometry is sometimes mistakenly assumed to be correlated with sphincter opening.
Recently, a number of groups have been looking at the concept of distending the junction as a better measure of its performance. This suggestion is not a new idea. In fact as early as the 1960’s, Harris and Pope identified that sphincters do not necessarily need to squeeze or contract tightly to be competent and, therefore, resistance to distension by measurement of radial force should be the prime determinant of sphincteric strength[24]. Studies on yield pressure in the stomach were probably an early distension method[2526]. This involved filling air into the stomach and monitoring the pressure reading when the OGJ was forced to open to allow air to travel up into the oesophagus.
In 2002, Pandolfino and coworkers demonstrated that the OGJ of patients with hiatal hernias was more distensible and shorter than normal subjects[27]. This was done using manometry, fluoroscopy and stepwise, controlled barostatic distension of the OGJ. Then by controlling the pressure, the OGJ diameter and length were measured during deglutitive relaxation. In reality, it is difficult to control pressure in a bag located at the distal end of a narrow diameter catheter.
Shaker et al[28], demonstrated that under different conditions, the effects of muscle action and passive elastic tissue on the distensibility of the junction could be determined. The investigators used a barostat bag, cylindrical in shape, placed across the OGJ and recorded pressure, volume and distensibility as changes in pressure related to changes in volume. These changes were only a rough proxy for distensibility changes in the digestive lumen at the oesophago-gastric junction, since changes in the bag volume could be attributed to all forces on the bag, and not just those relating to valvular or sphincter action. Nevertheless Shaker et al[28] went on to show how this technique could indicate an increase in pressure at stepped bag volumes, and implied that this was related to a reduction in the distensibility of the OGJ. This work clearly demonstrates that a distensibility test may be useful in evaluating the effects of the different components on OGJ function.
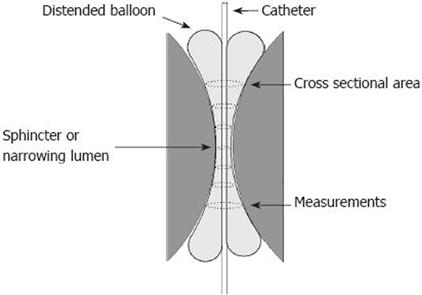
The functional lumen imaging probe (FLIP) takes distensibility testing to a higher level. FLIP allows a cylindrical shaped bag mounted on the distal end of a catheter to measure multiple cross-sectional areas (CSAs) at fixed intervals along the catheter. These CSAs can be used to build a dynamic three dimensional representation of the luminal geometric changes in the OGJ as the bag is distended on the catheter (Figure 4). In this way, luminal changes in the OGJ can be visually represented instantaneously, and with high spatial and temporal resolution[2930]. This technique has been shown to demonstrate differences in patients undergoing endoluminal therapy for reflux[31].
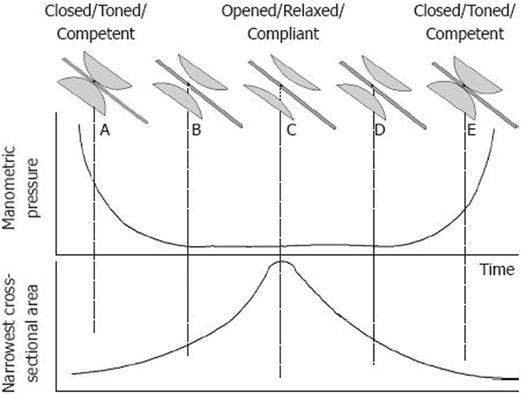
So what is the difference between measuring contraction or squeezing with manometry, and measuring opening or relaxation patterns using a distensibility technique? At the top of Figure 5 a simple series of drawings demonstrates the pattern of the sphincter part of the OGJ, and how it changes from being toned, compliant or competent to being relaxed or incompetent and then as it moves through the cycle back to being toned again. It can be seen how this cycle is measured using a manometry catheter or a distensibility probe such as FLIP, which can measure the narrowest CSA in the OGJ region. At the time point, represented by the dashed line A, the sphincter is contracted or squeezed, manometry will indicate by pressure that the force on the catheter is relatively high. Moving in time to the point at line B, it is evident that the sphincter has started to relax; the manometric pressure has dropped significantly since the sphincter no longer obscures or squeezes the pressure measuring point. Then, at time point C the sphincter is fully relaxed or open; there is no significant change in the manometric pressure reading from time point B. However, the CSA value continues to increase to a maximum value. In practice, pressure can tell us the difference between a toned and a relaxed sphincter. CSA can tell us the difference between an open and closed sphincter. It can, in effect, tell us the amount of opening. As the sphincter starts to close and is no longer relaxed, it can be observed that manometry is very insensitive to this action at time point D, whereas CSA has detected the narrowing pattern. Then, eventually, at time point E, manometry has detected the squeezing effect of the toned sphincter, and the CSA has reduced to the smallest measurable value.
The most significant difference between manometry and distensibility is in the type of measurement. Manometry measures pressure which is a proxy of the combined active and passive forces during squeezing. Ideally, it does not interfere with the measurement. In reality, you cannot measure a toned sphincteric region using a pressure point on a catheter which is running through the sphincter without interfering with its function. Distensibility, on the other hand is more of a challenge test. By inflating the liquid filled bag as it straddles the OGJ, we are able to measure its response to ramped or stepped distension.
There are no available objective tests for testing OGJ function in routine clinical practice. Current gold standard tests for GORD or achalasia tell us very little about the role of the OGJ in disease. Much of the evidence for the role of the OGJ is related to manometric studies carried out more than 20 years ago. The experts advise us that manometric measurements should not be used to confirm GORD. Yet, most practitioners accept that there is a strong relationship between OGJ dysfunction and reflux disease. It is clear that manometry, while being a great tool for assessing motility, does not provide optimal information for OGJ evaluation.
A distensibility test using a bag catheter probe such as FLIP may provide better information on the opening and closing dynamics of the OGJ, rather than just relying on the sphincter tonic state as measured by manometry. New measurement ideas around the concept of distending the OGJ offer new hope that a clinically useable test for compliance at the junction can be developed and could potentially help in determining appropriate therapy.
| 1. | Medlineplus - A service of the U.S. National Library of Medical and National Institutes for Health.. Available from: URL: http://www.nlm.nih.gov/medlineplus/gerd.html. |
| 2. | Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900-1920; quiz 1943. |
| 3. | Mittal RK, Balaban DH. The esophagogastric junction. N Engl J Med. 1997;336:924-932. |
| 4. | Adler RH, Firme CN, Lanigan JM. A valve mechanism to prevent gastroesophageal reflux and esophagitis. Surgery. 1958;44:63-76. |
| 5. | Jobe BA, Kahrilas PJ, Vernon AH, Sandone C, Gopal DV, Swanstrom LL, Aye RW, Hill LD, Hunter JG. Endoscopic appraisal of the gastroesophageal valve after antireflux surgery. Am J Gastroenterol. 2004;99:233-243. |
| 6. | Bonatti H, Achem SR, Hinder RA. Impact of changing epidemiology of gastroesophageal reflux disease on its diagnosis and treatment. J Gastrointest Surg. 2008;12:373-381. |
| 7. | Meshkinpour H, Kaye L, Elias A, Glick ME. Manometric and radiologic correlations in achalasia. Am J Gastroenterol. 1992;87:1567-1570. |
| 8. | Bredenoord AJ, Tutuian R, Smout AJ, Castell DO. Technology review: Esophageal impedance monitoring. Am J Gastroenterol. 2007;102:187-194. |
| 9. | Richter JE. New investigational therapies for gastroesophageal reflux disease. Thorac Surg Clin. 2005;15:377-384. |
| 10. | Pandolfino JE, Kahrilas PJ. AGA technical review on the clinical use of esophageal manometry. Gastroenterology. 2005;128:209-224. |
| 11. | Wikipedia. Free Software Foundation.. Available from: http://www.en.wikipedia.org/wiki/Valve (Oct, 2008). |
| 12. | Modlin IM, Malfertheiner P, Hunt RH, Armstrong D, Holtmann G, Quigley EM, Spechler SJ. GERD evaluation: time for a new paradigm? J Clin Gastroenterol. 2007;41:237-241. |
| 13. | Kahrilas PJ, Ghosh SK, Pandolfino JE. Challenging the limits of esophageal manometry. Gastroenterology. 2008;134:16-18. |
| 14. | Pandolfino JE, Kwiatek MA. Use and utility of the Bravo pH capsule. J Clin Gastroenterol. 2008;42:571-578. |
| 15. | Tutuian R, Castell DO. Multichannel intraluminal impedance: general principles and technical issues. Gastrointest Endosc Clin N Am. 2005;15:257-264. |
| 16. | Wilson JA, Mainie I, Tutuian R, Agrawal A, Castell DO. Multichannel intraluminal impedance and esophageal manometry data for unrestricted swallowing: establishing normal values. Dis Esophagus. 2008;21:51-56. |
| 17. | Conchillo JM, Schwartz MP, Selimah M, Samsom M, Sifrim D, Smout AJ. Acid and non-acid reflux patterns in patients with erosive esophagitis and non-erosive reflux disease (NERD): a study using intraluminal impedance monitoring. Dig Dis Sci. 2008;53:1506-1512. |
| 18. | Ingelfinger FJ, Kramer P, Sanchez GC. The gastroesophageal vestibule, its normal function and its role in cardiospasm and gastroesophageal reflux. Am J Med Sci. 1954;228:417-425. |
| 19. | Code CF, Fyke FE, Jr , Schlegel JF. The gastroesophageal sphincter in healthy human beings. Gastroenterologia. 1956;86:135-150. |
| 20. | DeVault KR, Castell DO. Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. Am J Gastroenterol. 2005;100:190-200. |
| 21. | Katz PO, Menin RA, Gideon RM. Utility and standards in esophageal manometry. J Clin Gastroenterol. 2008;42:620-626. |
| 22. | Sabate JM, Jouet P, Merrouche M, Pouzoulet J, Maillard D, Harnois F, Msika S, Coffin B. Gastroesophageal reflux in patients with morbid obesity: a role of obstructive sleep apnea syndrome? Obes Surg. 2008;18:1479-1484. |
| 23. | Dent J. A new technique for continuous sphincter pressure measurement. Gastroenterology. 1976;71:263-267. |
| 24. | Harris LD, Pope CE 2nd. "Squeeze" vs resistance: an evaluation of the mechanism of sphincter competence. J Clin Invest. 1964;43:2272-2278. |
| 25. | Ismail T, Bancewicz J, Barlow J. Yield pressure: a new concept in the evaluation of GERD? Am J Gastroenterol. 1996;91:616-617. |
| 26. | McGouran RC, Galloway JM, Wells FC, Hendrie OR. Is yield pressure at the cardia increased by effective fundoplication? Gut. 1989;30:1309-1312. |
| 27. | Pandolfino JE, Shi G, Curry J, Joehl RJ, Brasseur JG, Kahrilas PJ. Esophagogastric junction distensibility: a factor contributing to sphincter incompetence. Am J Physiol Gastrointest Liver Physiol. 2002;282:G1052-G1058. |
| 28. | Shaker R, Bardan E, Gu C, Massey BT, Sanders T, Kern MK, Hoffmann RG, Hogan WJ. Effect of lower esophageal sphincter tone and crural diaphragm contraction on distensibility of the gastroesophageal junction in humans. Am J Physiol Gastrointest Liver Physiol. 2004;287:G815-G821. |
| 29. | McMahon BP, Frokjaer JB, Drewes AM, Gregersen H. A new measurement of oesophago-gastric junction competence. Neurogastroenterol Motil. 2004;16:543-546. |
| 30. | McMahon BP, Frokjaer JB, Kunwald P, Liao D, Funch-Jensen P, Drewes AM, Gregersen H. The functional lumen imaging probe (FLIP) for evaluation of the esophagogastric junction. Am J Physiol Gastrointest Liver Physiol. 2007;292:G377-G384. |
| 31. | Jobe BA, Kock GH, Kraemer SJ, McMahon BP, Witteman B, Gravesen FH, Lorenzo CS, O’Rourke RW, Shumaker DA, Owens MM. Tailored transoral incisionless fundoplication (TIF) in the treatment of GERD: the anatomic and physiologic basis for reconstruction of the esophagogastric junction using a novel approach. Gastoenterology. 2008;134:A854. |