Published online Feb 7, 2008. doi: 10.3748/wjg.14.815
Revised: November 1, 2007
Published online: February 7, 2008
It is one of the most important problems for general surgeons to decide which operation should be undertaken on patients with intra-abdominal infection, especially those with concomitant abdominal hypertension. Recentlly, closure techniques using prosthetic meshes in order to retain abdominal tension and to control sepsis have become very popular for patients with abdominal sepsis and hypertension. We used chorioamniotic membrane instead of plastic material to cover the open abdomen. We conclude that human chorioamniotic membrane prepared under sterile conditions may be an alternative to conventional plastic bags in daily practice, for preventing serosal erosion and fistulas in patients undergoing open abdominal surgery.
- Citation: Tekin S, Tekin A, Küçükkartallar T, Çakir M, Kartal A. Use of chorioamniotic membrane instead of bogota bag in open abdomen: How I Do It? World J Gastroenterol 2008; 14(5): 815-816
- URL: https://www.wjgnet.com/1007-9327/full/v14/i5/815.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.815
There are some important indications for open abdominal surgery, such as abdominal compartment syndrome, damage control surgery, severe peritonitis and infected pancreatic necrosis. A Bogota bag, which is sutured to the abdominal wall or to the fascia, is used to cover the open abdomen. It needs to be changed frequently until the underlying problem in the abdomen is solved. If there is no need of early abdominal closure, a skin graft is placed over the granulation tissue that covers the viscus. After that, the deliberately created ventral hernia is repaired 6-12 mo later. The above situation has been changed considerably with the introduction of vacuum application and biological prosthetic material[1–5]. Until recently, the practice was to discharge patients with an open fascia and partially closed skin.
An open abdomen is a heavy burden for the body. Electrolyte-fluid losses and protein-energy requirements are high in the open abdomen. The need for intensive care also increases costs, and the condition becomes more serious if there are coexisting fistulae or an open stoma in the gut.
We consider the use of chorioamniotic membrane as a biological material when vacuum application is not possible or plastic cover might be harmful. To the best of our knowledge, this is the first instance in which chorioamniotic membrane has been used for this purpose.
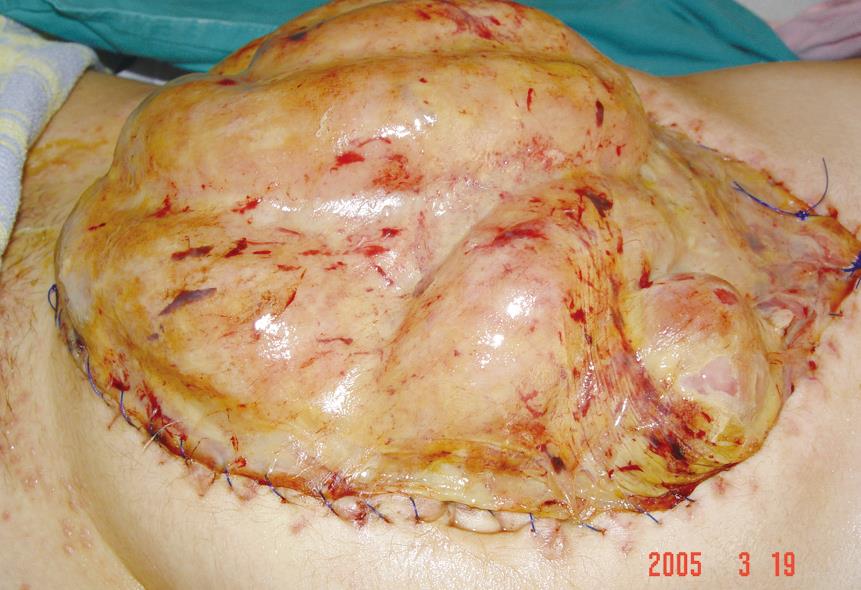
The chorioamniotic membrane was obtained from elective cesarean section, after patient consent was obtained. The membrane was prepared under sterile conditions by removing the cotyledons from the placenta (Figure 1). The membrane was then kept in 1 L normal saline containing 1 g streptomycin and 1 MU penicillin at 4°C for 24 h. After each irrigation of the abdomen, chorioamniotic membrane was applied as a cover, with maternal surface facing the viscera (Figure 2). This procedure was repeated every 2 d. Immediately following the second application, it was clearly observed that serosal erosion showed signs of healing and the adhesions between the loops became clearer. The application decreased edema of the gut and abdominal wall, and the bowel was attached to the abdominal wall (Figure 3). Patients were discharged for definitive treatment planned after 6 mo. There were no problems in early follow-up. Six months postoperatively, ventral hernias were successfully repaired using omental or online mesh hernioplasty.
Open abdomen is a life saving procedure when indicated. Its mortality and morbidity increase when combined with that of the primary underlying illness[5]. Currently, patients with open abdomen are discharged with a ventral hernia, which is covered with a graft that needs further repair.
It is reported that by using vacuum methods, fascial defects are reduced sufficiently to be closed[1–4]. It is also reported that in cases where closure is inadequate, by using acellular dermis, patients can be sent home without a fascial defect[5]. However, there is no long-term follow-up of wide series on outcomes with this biological material.
In our patients, human chorioamniotic membrane obtained from elective cesarean sections was used instead of the plastic Bogota bag. It is a natural biological material, therefore, it is a more appropriate cover for erosion of the intestinal serosa. Moreover, chorioamniotic membrane accelerated adhesions among the loops and helped to stabilize the abdomen.
There are different indications for the use of placental amniotic membrane. It is used successfully to cover tendon defects, to prevent adhesions[6]. The membrane is also used for eye and skin diseases[7]. Previously, in order to prevent fistula of damaged bowel segments, fibrin glue, together with acellular dermal matrix, was used for covering the open abdomen. We have used human chorioamniotic membrane for the same purpose[89].
We use the chorioamniotic membrane because the amniotic membrane is very thin. The maternal surface is placed over the viscera. Another possibility is to place the membrane between the viscus and the peritoneum. Similar outcomes may be expected with this method and vacuum techniques. In the latter, the deepest part of the vacuum system which is plastic cover is placed between the peritoneum and the viscus to prevent the parietal peritoneum from adhering to the visceral peritoneum. In our method, because the fetal surface is not sticky and smooth, it might prevent the viscus from adhering to the peritoneum. In the present case, because it was impossible to keep the viscus in the abdomen, we deliberately aimed for adhesion between the parietal and visceral peritoneum.
We conclude that human chorioamniotic membrane prepared under sterile conditions may be an alternative to conventional plastics bags in daily practice, for preventing serosal erosion and fistulas in patients with an open abdomen. The biological membrane is cheap, practical and is well suiting over viscera. It is sutured easily and does not make plies like the plastic material in use.
| 1. | Miller PR, Meredith JW, Johnson JC, Chang MC. Prospective evaluation of vacuum-assisted fascial closure after open abdomen: planned ventral hernia rate is substantially reduced. Ann Surg. 2004;239:608-614; discussion 614-616. |
| 2. | Stone PA, Hass SM, Flaherty SK, DeLuca JA, Lucente FC, Kusminsky RE. Vacuum-assisted fascial closure for patients with abdominal trauma. J Trauma. 2004;57:1082-1086. |
| 3. | Navsaria PH, Bunting M, Omoshoro-Jones J, Nicol AJ, Kahn D. Temporary closure of open abdominal wounds by the modified sandwich-vacuum pack technique. Br J Surg. 2003;90:718-722. |
| 4. | Garner GB, Ware DN, Cocanour CS, Duke JH, McKinley BA, Kozar RA, Moore FA. Vacuum-assisted wound closure provides early fascial reapproximation in trauma patients with open abdomens. Am J Surg. 2001;182:630-638. |
| 5. | Scott BG, Feanny MA, Hirshberg A. Early definitive closure of the open abdomen: a quiet revolution. Scand J Surg. 2005;94:9-14. |
| 6. | Demirkan F, Colakoglu N, Herek O, Erkula G. The use of amniotic membrane in flexor tendon repair: an experimental model. Arch Orthop Trauma Surg. 2002;122:396-399. |
| 7. | Santos ST, Cua IY, Uy HS, Lim-Bon-Siong R. Amnion membrane versus bandage contact lens in the treatment of acute injury. Philipp J Ophthalmol. 2001;26:1-2. |