Published online Dec 21, 2008. doi: 10.3748/wjg.14.7252
Revised: November 23, 2008
Accepted: November 30, 2008
Published online: December 21, 2008
Mucinous cystic neoplasms (MCNs) of the pancreas occur mostly in females and are potentially sex hormone-sensitive. However, a MCN occurring during pregnancy is quite rare. A 30-year-old woman in the tenth week of pregnancy was referred to us because of a rapid increase in left hypochondrial distending pain. On ultrasound, the patient had a large intra-abdominal cystic lesion. She was thereafter diagnosed with missed abortion and a computed tomography scan showed that the lesion was a cystic tumor 18 cm in diameter originating from the pancreatic tail. The patient subsequently underwent tumor resection with distal pancreatectomy, sparing the spleen. Histopathological analysis of the specimen revealed a pancreatic MCN with moderate dysplasia. Immunohistochemically, the tumor was positive for both estrogen and progesterone receptors. To our knowledge, this is the first reported case of pancreatic MCN with moderate dysplasia in association with pregnancy. Our case strongly indicates that pancreatic MCN is female-hormone dependent.
- Citation: Ikuta SI, Aihara T, Yasui C, Iida H, Yanagi H, Mitsunobu M, Kakuno A, Yamanaka N. Large mucinous cystic neoplasm of the pancreas associated with pregnancy. World J Gastroenterol 2008; 14(47): 7252-7255
- URL: https://www.wjgnet.com/1007-9327/full/v14/i47/7252.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.7252
Mucinous cystic neoplasm (MCN) of the pancreas is an uncommon tumor characterized by a proliferation of mucin-producing columnar epithelium supported by ovarian-type stroma[1,2]. MCNs are typically located in the pancreatic body or tail and rarely communicate with the pancreatic duct[1,2]. Pancreatic MCNs occur almost exclusively in females, and are potentially sex hormone-sensitive, according to the studies reported to date[2]. However, MCNs encountered in pregnancy are rare; only eight such cases have been reported in the English literature[3-10]. In this report, we describe a 30-year-old woman with a large pancreatic MCN that grew rapidly during the early stage of pregnancy.
A 30-year-old woman in the tenth week of pregnancy was referred to our hospital due to increasing distending pain in the left hypochondrial region over the last month. She had no notable medical history, but had complained of vague epigastric discomfort over the past several years. Physical examination suggested the presence of an elastic hard mass, approximately 20 cm in diameter, in the left upper quadrant. Laboratory tests showed slight anemia and normal levels of amylase, liver enzymes, and tumor markers. An abdominal ultrasound demonstrated a huge cystic lesion in the left upper abdomen. Soon after hospitalization, her pregnancy ended in missed abortion at 10 wk gestation, which was confirmed by clinical and ultrasound findings. Further evaluation by computed tomography (CT) scanning revealed a well-demarcated cystic mass, measuring 18 cm × 14 cm, probably originating from the distal pancreas (Figure 1). There were no septa or protruding lesions inside the cystic mass.
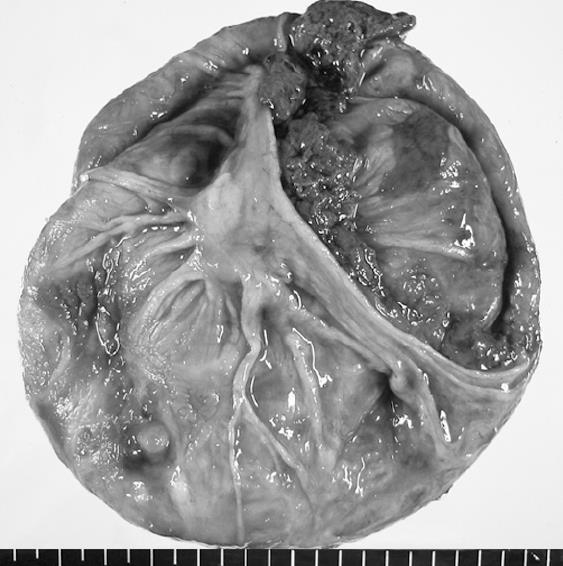
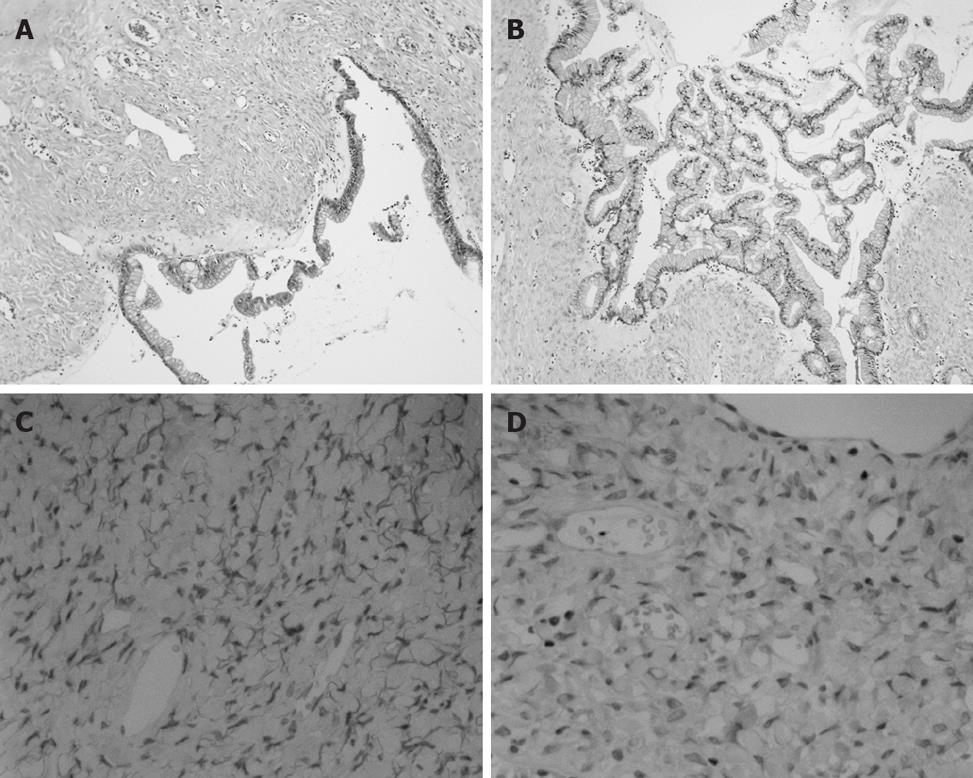
Ultrasound-guided percutaneous cyst aspiration was then performed to reduce the pain, and 2100 mL of dark-brownish mucinous fluid was aspirated, without spillage into the peritoneal cavity. The aspirated fluid showed an amylase level of 59 IU/L, a carcinoembryonic antigen (CEA) level of 32100 ng/mL, and a carbohydrate-associated antigen (CA) 19-9 level of 34500 U/mL. Cytological examination of the fluid was class II with no malignant findings. Thus, a diagnosis of possible pancreatic MCN was made. After dilatation and curettage, the cystic mass was resected with distal pancreatectomy. Since invasive carcinoma was not suspected by preoperative images and intraoperative findings, the spleen was preserved. The tumor was unilocular, had thick walls, and was filled with tenacious mucoid material and necrotic debris (Figure 2). Histopathological analysis showed a mucin-producing columnar epithelium lining the inner wall of the cyst, with ovarian-type stromal tissue (Figure 3A). The epithelium had a focal papillary architecture without significant cytologic atypia, giving a diagnosis of pancreatic MCN with moderate dysplasia (Figure 3B). Immunohistochemical studies showed positive staining for both progesterone and estrogen receptors in the stromal cell nuclei (Figure 3C and D). The patient had an uneventful post-operative course, and she remained disease-free for 12 mo after surgery.
To our knowledge, eight cases of pancreatic MCN associated with pregnancy have been reported since the first report in 1968 by Smithers et al[7]. Four cases were histologically diagnosed as benign mucinous cystadenoma[3-6], while the other four were diagnosed as mucinous cystadenocarcinoma[7-10]. Our case might be the first case of pancreatic MCN with moderate dysplasia (also referred to as “borderline tumor”), in association with pregnancy.
Although cystic tumors of the pancreas often grow slowly and can remain indolent for many years[5,10], MCNs which develop during pregnancy tend to grow more rapidly and achieve extraordinary size. Kato et al[4] reported that a pancreatic MCN in a pregnant patient rapidly increased in volume from 2619 to 4950 mL over 46 d. Ganepola et al[3] also reported a case whose cyst increased in size from 5.5 cm to more than 12 cm within 4 mo. In a recent review, 344 MCNs defined by ovarian-type stroma had a mean size of 8.7 cm (range, 0.6-35 cm)[11], whereas in the review of reported cases and in our case, pregnancy associated-MCNs had a mean size of 15 cm (range, 10-22 cm).
These findings are consistent with the concept that pancreatic MCNs may be responsive to female sex hormones. One series reported that stromal cell nuclei were positive for estrogen receptors in 15 of 65 MCN cases (23%) and for progesterone receptors in 46 cases (71%)[2]. The predominantly female occurrence and the expression of female hormone receptors in MCNs has been the subject of much speculation. One possibility is that MCNs originate from primitive ovarian cells, which are incorporated into the embryonic pancreas when the left primordial gonad is in close proximity to the dorsal pancreatic anlage during embryogenesis[1]. The dorsal pancreatic anlage gives rise to the body and tail of the pancreas, and this hypothesis could explain the predilection of MCNs for the distal pancreas. Another possibility is that the neoplastic epithelial cells of MCNs might induce ovarian stromal differentiation in cells that normally reside in the pancreas. This concept is based on the fact that the stroma in the fetal pancreas is morphologically similar to that of MCNs[12]. However, direct evidence for these hypotheses has yet to be found.
Pancreatic MCN presents a clinical problem in that it always carries a malignant potential. Mucinous cystadenocarcinoma can be considered not only as a neoplasm arising de novo but also as an evolution of the benign form[8]. As large tumor size was reported to be one of the predictive factors of malignant MCNs[13], it is prudent to assume that the increased growth of MCNs during pregnancy brings with it some degree of increased risk for malignant transformation[9]. However, it remains unclear whether high levels of estrogen and progesterone in pregnancy accelerate the malignant transformation of a benign tumor into a malignant tumor. In fact, there is evidence that a decrease in progesterone receptor immunoreactivity was correlated with histological or cytological atypicality and a worse prognosis[2].
Pancreatic MCN detected during pregnancy requires special management considerations due to its large size and resultant risk for fetal growth restriction. So far, there have been four cases of successful antepartum resection of pancreatic MCN during pregnancy that later resulted in healthy infants[3-5,9]. These authors have recommended the second trimester as a safe period for surgery because this period provides enough time for fetal maturity. Since the tumor in the present case did not compress the uterus, there may be no direct correlation between tumor progression and miscarriage in our patient.
In the present case, successful cyst aspiration provided a basis for accurate diagnosis as well as symptom relief for the patient. Cyst fluid analysis has recently been utilized to differentiate pancreatic cystic neoplasms. van der Waaij et al[14] found that an amylase concentration below 250 U/L effectively ruled out pseudocyst. In addition, it has been reported that cyst fluid CA 19-9 level greater than 50 000 U/mL had a sensitivity of 75% and a specificity of 90% for distinguishing mucinous tumors from other cystic lesions[15]. Furthermore, a recent series[16] revealed that cyst fluid CEA greater than 800 ng/mL had a sensitivity of 42.9% and a specificity of 95.2% for diagnosing pancreatic MCNs. When performing cyst aspiration, however, care must be taken to avoid spillage of cyst contents, which may result in the development of pseudomyxoma peritonei[4].
In summary, our report describes the ninth case of pancreatic MCN associated with pregnancy and the first such case of MCN with moderate dysplasia. Our case strongly indicates that pancreatic MCN is a hormone-dependent tumor that can grow dramatically during pregnancy. Considering the malignant potential of this tumor and adverse effects on the fetus, complete resection should be performed without delay.
Peer reviewer: Alyssa M Krasinskas, MD, Assistant Professor, Department of Pathology, University of Pittsburgh Medical Center, Presbyterian Hospital, A610, 200 Lothrop Street, Pittsburgh, PA 15213-2546, United States
S- Editor Li LF L- Editor Webster JR E- Editor Lin YP
| 1. | Zamboni G, Scarpa A, Bogina G, Iacono C, Bassi C, Talamini G, Sessa F, Capella C, Solcia E, Rickaert F. Mucinous cystic tumors of the pancreas: clinicopathological features, prognosis, and relationship to other mucinous cystic tumors. Am J Surg Pathol. 1999;23:410-422. |
| 2. | Thompson LD, Becker RC, Przygodzki RM, Adair CF, Heffess CS. Mucinous cystic neoplasm (mucinous cystadenocarcinoma of low-grade malignant potential) of the pancreas: a clinicopathologic study of 130 cases. Am J Surg Pathol. 1999;23:1-16. |
| 3. | Ganepola GA, Gritsman AY, Asimakopulos N, Yiengpruksawan A. Are pancreatic tumors hormone dependent?: A case report of unusual, rapidly growing pancreatic tumor during pregnancy, its possible relationship to female sex hormones, and review of the literature. Am Surg. 1999;65:105-111. |
| 4. | Kato M, Kubota K, Kita J, Shimoda M, Rokkaku K, Inaba N, Fukasawa I, Honma K. Huge mucinous cystadenoma of the pancreas developing during pregnancy: a case report. Pancreas. 2005;30:186-188. |
| 5. | Lopez-Tomassetti Fernandez EM, Martin Malagon A, Arteaga Gonzalez I, Muniz Montes JR, Diaz Luis H, Gonzalez Hermoso F, Carrillo Pallares A. Mucinous cystic neoplasm of the pancreas during pregnancy: the importance of proper management. J Hepatobiliary Pancreat Surg. 2005;12:494-497. |
| 6. | Ishikawa K, Hirashita T, Kinoshita H, Kitano M, Matsuo S, Matsumata T, Kitano S. Large mucinous cystadenoma of the pancreas during pregnancy: report of a case. Surg Today. 2007;37:1013-1017. |
| 7. | Smithers BM, Welch C, Goodall P. Cystadenocarcinoma of the pancreas presenting in pregnancy. Br J Surg. 1986;73:591. |
| 8. | Baiocchi C, Landonio G, Majno M, Minola E, Scanzi F, Ghislandi E. Pancreatic cystadenocarcinoma and pregnancy: a case report. Tumori. 1990;76:294-295. |
| 9. | Herring AA, Graubard MB, Gan SI, Schwaitzberg SD. Mucinous cystadenocarcinoma of the pancreas during pregnancy. Pancreas. 2007;34:470-473. |
| 10. | Ozden S, Haliloglu B, Ilter E, Akin FT, Kebudi A, Peker O. An extremely rare cause of acute abdomen in pregnancy: ruptured pancreatic mucinous cystadenocarcinoma. Pancreas. 2007;34:474-476. |
| 11. | Goh BK, Tan YM, Chung YF, Chow PK, Cheow PC, Wong WK, Ooi LL. A review of mucinous cystic neoplasms of the pancreas defined by ovarian-type stroma: clinicopathological features of 344 patients. World J Surg. 2006;30:2236-2245. |
| 12. | Volkan Adsay N. Cystic lesions of the pancreas. Mod Pathol. 2007;20 Suppl 1:S71-S93. |
| 13. | Crippa S, Salvia R, Warshaw AL, Dominguez I, Bassi C, Falconi M, Thayer SP, Zamboni G, Lauwers GY, Mino-Kenudson M. Mucinous cystic neoplasm of the pancreas is not an aggressive entity: lessons from 163 resected patients. Ann Surg. 2008;247:571-579. |
| 14. | van der Waaij LA, van Dullemen HM, Porte RJ. Cyst fluid analysis in the differential diagnosis of pancreatic cystic lesions: a pooled analysis. Gastrointest Endosc. 2005;62:383-389. |
| 15. | Hammel P, Levy P, Voitot H, Levy M, Vilgrain V, Zins M, Flejou JF, Molas G, Ruszniewski P, Bernades P. Preoperative cyst fluid analysis is useful for the differential diagnosis of cystic lesions of the pancreas. Gastroenterology. 1995;108:1230-1235. |