Published online Nov 28, 2008. doi: 10.3748/wjg.14.6881
Revised: October 31, 2008
Accepted: November 7, 2008
Published online: November 28, 2008
Port site hernia develops through a fascial or peritoneal layer that was inadequate or not repaired. It is a rare complication of laparoscopic surgery which may lead to serious problems. Here, we present a 77-year-old female, diagnosed with a small bowel hernia through a 10-mm port site. We had performed ten cases of laparoscopy-assisted distal gastrectomy before this case. The patient complained of left lower abdominal pain with a palpable mass. Abdominal CT showed an incarcerated small bowel hernia and the patient underwent segmental resection of the strangulated small bowel through a minimally extended port site incision.
- Citation: Lee JH, Kim W. Strangulated small bowel hernia through the port site: A case report. World J Gastroenterol 2008; 14(44): 6881-6883
- URL: https://www.wjgnet.com/1007-9327/full/v14/i44/6881.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.6881
Recently, laparoscopy-assisted gastrectomy (LAG) for early gastric cancer has been accepted as technically and oncologically safe and feasible. During LAG, 10 mm or larger trocars are used for traction of the intra-abdominal organs, and fascial defects created by those trocars are usually closed because of concern over the potential for small bowel hernia. Port site hernia is a rare complication following laparoscopic surgery: however, occurrence of this may be dangerous and, hence, may have a fatal outcome. Therefore, we report the clinical course of our case and prepare a review for the management of port site hernia.
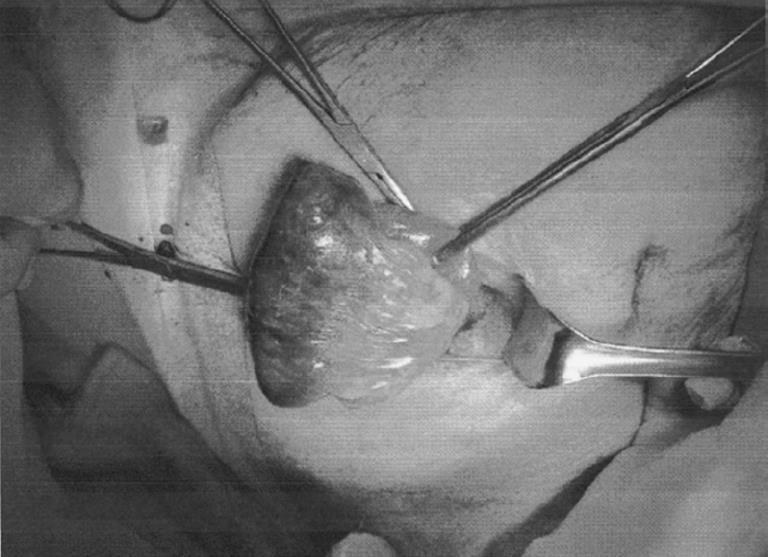
A 77-year-old woman was admitted to our hospital for gastric cancer treatment. She had complained of dyspepsia and epigastric discomfort for 20 d: following gastrofiberoscopy, early gastric cancer (type I + IIa) was found at the prepyloric antrum. She had no past medical history except well-controlled hypertension, and no abnormalities were found during preoperative evaluation. During laparoscopic surgery, a total of 5 trocars were applied to perform surgical procedures, and all the trocars used were the bladed type. A 10 mm trocar was inserted into the abdominal cavity via the umbilicus to prepare the pneumoperitoneum for electro-laparoscopy. After sufficient inflation of the abdominal cavity, 5 mm and 12 mm trocars were placed into the right side, and 5 mm and 10 mm trocars were inserted into the left side. She underwent LAG with D1 + β lymph node dissection and Billorth-II gastrojejunostomy. The fascial defects at the 10 mm and 12 mm port sites were repaired by 2-0 absorbable vicryl sutures. The patient’s recovery was progressing favorably, so we put her on a diet on the 2nd day after surgery, and no abnormalities were detected. On the 7th day after the operation, the patient complained of vague abdominal pain and vomiting, but those symptoms were alleviated by conservative support. The next day, however, the patient developed a fever (38°C) and manifested left lower quadrant abdominal pain with a palpable mass. Emergency ultrasonography and abdominal CT were performed, and a structure that looked like an abscess or hernia of the small bowel was detected (Figure 1). We suspected an incarcerated port site or strangulated hernia of the small bowel and performed exploratory surgery. The port site incision that had been made on the left lower quadrant was transversely extended to about 4 cm long. After fascial layer sutures were untied, it was observed that the strangulated small bowel was pushing into a peritoneal defect in the abdominal wall (Figure 2). The length of incarcerated small bowel was about 10 cm long. After that was taken out through an extended incision, we carefully observed its viability and decided to remove a ischemic portion of the small bowel through an extended port site. Then we performed segmental resection of the strangulated small bowel and end-to-end anastomosis. After the operation, there were no specific events, and the patient recovered.
Port site hernia is a rare complication following laparoscopic surgery. Tonouchi et al[1] reported that the incidence of port site hernia was 0.65%-2.80% and classified port site hernia into three types. The early-onset type occurs immediately after the operation, the late-onset type develops after several months and the special-type presents as dehiscence of the whole abdominal wall. Relative to the size of the port site, Kadar et al[2] reported that incidence of port site hernia was 0.23% at a 10 mm port site and 3.1% at a 12 mm port site, and Mayol et al[3] reported umbilical port site hernia with an incidence of 1.6%. Port site hernia may occur at any time during the postoperative course, though our case occurred early during the postoperative course[4-6]. It is known that a port site of larger than 10 mm in diameter usually causes hernia while a 5 mm port site rarely causes hernia[5]. Hence, most surgeons routinely repair the fascia of 10 mm or larger port sites to prevent hernia.
In an experimental study of wounds relative to the type of trocar, Kolata et al[7] reported that a non-bladed trocar created smaller peritoneal port site wounds than a conventional pyramidal tip trocar and they hypothesized that a non-bladed type of trocar might reduce the chance of trocar wound hernia. Another study showed that a 10 mm or 12 mm port site created by a non-bladed trocar did not require fascial closure if it was placed in a non-midline position above the arcuate line[8]. Since the non-bladed trocar split the muscle rather than cutting it, it allowed the oblique muscle to reanneal together more readily. Moreover, this study suggested that misalignment of the fascial defect (created by the non-bladed trocar) aided inhibition of trocar site hernia. However, recently non-bladed trocars have mostly been used to access the port site; hence, many cases occur under this condition and some reports have suggested that herniation through the peritoneal defect might develop even though the fascial defect has been repaired. In our case, an intestinal hernia via peritoneal defect developed below the repaired fascial layer. Therefore, fascial and, if possible, peritoneal repair of port sites are necessary to prevent port site hernia.
Many methods and devices for closure of port sites have been introduced[9,10], and each of them has its merits and demerits. Generally, it is not difficult to repair port sites that are larger than 10 mm using a small retractor and hemostat unless a patient is severely obese. However, if the port site is less than 5 mm, it will be hard to close and extension of the port site may be necessary for repair. Some devices, such as a Deschamps needle, a suture carrier, and an Endoclose suture device (Tyco Auto Suture International, Inc. Norwalk, CT, USA) , may be helpful in repairing fascial and peritoneal defects[9]. In addition to direct repair of the port site, recently the port plug technique without suturing was introduced. Moreno-Sanz et al[10] reported that inserting a Bioabsorbable Hernia Plug (W.L Gore and Associates Inc, Flagstaff, AZ, USA) to the port site was safe and feasible as a way to prevent port site hernia. Before this unexpected event, trocar sites had been imprudently repaired. After that incident, we made every effort to repair the fascial and peritoneal defects of the port site using an extremely concaved needle and a hemostat as far as possible. After skin and subcutaneous tissue were retracted to opposite sites using small retractors, visualized fascia were clamped using a hemostat and the hemostat was then lifted to allow for detection of the peritoneum. After the peritoneum was clamped by the hemostat, the two layers were closed separately or together. This technique was similar to the dual-hemostat technique introduced by Spalding et al[11] and was feasible and simple to perform unless a patient was severely obese.
Clinical courses of port site hernia are varied and depend on the degree of intestinal entry to the defect. Most patients present with vague abdominal pain, nausea, vomiting, a palpable or painful mass around port site, and fever if the bowel is incarcerated. If a patient complains of mild symptoms including nausea, vomiting and vague abdominal pain, early diagnosis may be delayed. Plain radiographs may be useful in some cases; however, plain radiographs only reveal the existence or nonexistence of the bowel obstruction. Therefore, they are limited in diagnosing port site hernia. In the case of Boughey et al[12], a definite diagnosis was achieved by explorative laparoscopic examination. Abdominal CT may be an effective diagnostic method if a patient complains of the symptoms described above without a palpable mass as it can differentiate adhesion from port site hernia and indicate the location of the port site hernia. Therefore, if atypical symptoms persist with obscure plain radiographs, abdominal CT is helpful in early diagnosis. Exploratory surgery with reduction of the incarcerated bowel is used to treat a port site hernia. According to previous reports, there are a few ways to access the abdominal cavity. One is a laparoscopic approach and another is an open approach through extension of the port site involved or other incision sites. Unless the incarcerated bowel is frankly ischemic, the laparoscopic approach is an acceptable method. In our case, we extended the port site and corrected the disorder because strangulation of the bowel was apparent.
In conclusion, it is necessary to repair the fascial and peritoneal layers to prevent port site hernia. Although port site hernia is rare, surgeons should keep this possibility in mind. Prompt intervention may reduce unfavorable events if port site hernia is suspected.
Peer reviewer: Dr. Kalpesh Jani, Sigma 102, Abhishek House, Vadodara 390011, India
S- Editor Zhong XY L- Editor O’Neill M E- Editor Zheng XM
| 1. | Tonouchi H, Ohmori Y, Kobayashi M, Kusunoki M. Trocar site hernia. Arch Surg. 2004;139:1248-1256. |
| 2. | Kadar N, Reich H, Liu CY, Manko GF, Gimpelson R. Incisional hernias after major laparoscopic gynecologic procedures. Am J Obstet Gynecol. 1993;168:1493-1495. |
| 3. | Mayol J, Garcia-Aguilar J, Ortiz-Oshiro E, De-Diego Carmona JA, Fernandez-Represa JA. Risks of the minimal access approach for laparoscopic surgery: multivariate analysis of morbidity related to umbilical trocar insertion. World J Surg. 1997;21:529-533. |
| 4. | Itoh T, Fuji N, Taniguchi H, Watanabe T, Kosuga T, Kashimoto K, Naito K. Port site herniation of the small bowel following laparoscopy-assisted distal gastrectomy: a case report. J Med Case Reports. 2008;2:48. |
| 5. | Reardon PR, Preciado A, Scarborough T, Matthews B, Marti JL. Hernia at 5-mm laparoscopic port site presenting as early postoperative small bowel obstruction. J Laparoendosc Adv Surg Tech A. 1999;9:523-525. |
| 6. | Cadeddu MO, Schlachta CM, Mamazza J, Seshadri PA, Poulin EC. Soft-tissue images. Trocar-site hernia after laparoscopic procedures. Can J Surg. 2002;45:9-10. |
| 7. | Kolata RJ, Ransick M, Briggs L, Baum D. Comparison of wounds created by non-bladed trocars and pyramidal tip trocars in the pig. J Laparoendosc Adv Surg Tech A. 1999;9:455-461. |
| 8. | Liu CD, McFadden DW. Laparoscopic port sites do not require fascial closure when nonbladed trocars are used. Am Surg. 2000;66:853-854. |
| 9. | Shaher Z. Port closure techniques. Surg Endosc. 2007;21:1264-1274. |
| 10. | Moreno-Sanz C, Picazo-Yeste JS, Manzanera-Díaz M, Herrero-Bogajo ML, Cortina-Oliva J, Tadeo-Ruiz G. Prevention of trocar site hernias: description of the safe port plug technique and preliminary results. Surg Innov. 2008;15:100-104. |
| 11. | Spalding SC, Ponsky TA, Oristian E. A new Dual-hemostat technique to facilitate the closure of small laparoscopic trocar incisions. Surg Endosc. 2003;17:164-165. |
| 12. | Boughey JC, Nottingham JM, Walls AC. Richter's hernia in the laparoscopic era: four case reports and review of the literature. Surg Laparosc Endosc Percutan Tech. 2003;13:55-58. |