Published online Nov 14, 2008. doi: 10.3748/wjg.14.6589
Revised: October 15, 2008
Accepted: October 22, 2008
Published online: November 14, 2008
A Killian-Jamieson diverticulum (KJD) is an unfamiliar and rare cervical esophageal diverticulum. This diverticulum originates on the anterolateral wall of the proximal cervical esophagus through a muscular gap (the Killian-Jamieson space) below the cricopharyngeal muscle and lateral to the longitudinal muscle of the esophagus. To date, only surgical treatment has been recommended for a symptomatic KJD due to its close proximity to the recurrent laryngeal nerve and the concern of possible nerve injury. Recently, traditional open surgery for a symptomatic KJD is being challenged by the development of new endoscopic techniques and devices. We present here a case of a symptomatic KJD that was successfully treated with the flexible endoscopic diverticulotomy using two new devices. An isolated-tip needle-knife papillotome (Iso-Tome) was used for the dissection of the tissue bridge of the diverticulum. And a flexible overtube with a modified distal end (a fitted overtube) was used for adequate visualization of the tissue bridge of the diverticulum and protection of the surrounding tissue during dissection of the tissue bridge. Our successful experience suggests that the flexible endoscopic diverticulotomy with the use of appropriate endoscopic devices can be a safe and effective method for the treatment of a symptomatic KJD.
- Citation: Lee CK, Chung IK, Park JY, Lee TH, Lee SH, Park SH, Kim HS, Kim SJ. Endoscopic diverticulotomy with an isolated-tip needle-knife papillotome (Iso-Tome) and a fitted overtube for the treatment of a Killian-Jamieson diverticulum. World J Gastroenterol 2008; 14(42): 6589-6592
- URL: https://www.wjgnet.com/1007-9327/full/v14/i42/6589.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.6589
A Killian-Jamieson diverticulum (KJD) is an unfamiliar and rare disease entity as compared with Zenker’s diverticulum (ZD), which is the most commonly encountered diverticulum of the cervical esophagus[1-4]. These two types of cervical esophageal diverticula can be diagnosed and can be differentiated by radiological studies or by the use of endoscopy. A KJD originates on the anterolateral wall of the proximal cervical esophagus through a muscular gap (the Killian-Jamieson space) below the cricopharyngeal muscle and lateral to the longitudinal muscle of the esophagus[1-4]. A ZD develops at the anatomically weak posterior zone (the Killian’s triangle) just above the cricopharyngeal muscle[1-4]. Although a KJD is anatomically distinct from a ZD, the symptoms attributable to a KJD are similar to those of a ZD[3]. To date, only surgical management has been recommended in symptomatic patients with a KJD[2]. Very recently, the first report of the flexible endoscopic treatment of a KJD was published[4].
We present here a rare case of a symptomatic KJD that was successfully treated with the flexible endoscopic diverticulotomy using an isolated-tip needle-knife papillotome (Iso-Tome) and a fitted overtube.
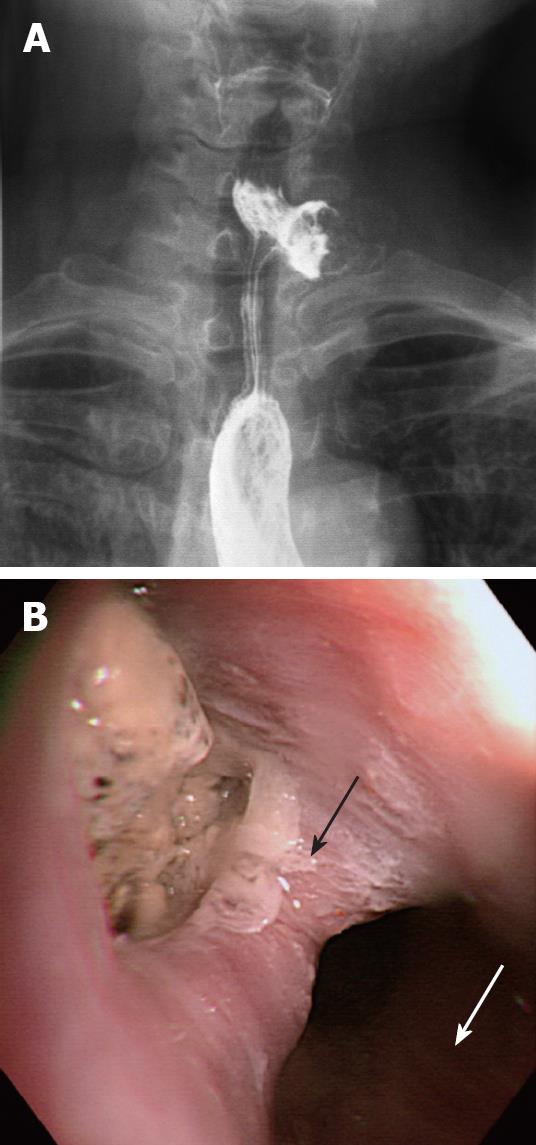
A 55-year-old woman was referred from a local clinic for a 6-mo history of pharyngeal discomfort and an abnormal contrast esophagogram. An anteroposterior projection of a barium swallow image revealed a 1.6 cm left-sided KJD with a wide neck (Figure 1A). The diverticulum was filled with contrast and food debris, as demonstrated by filling defects in the contrast pool. Contrast retention was persistent regardless of the barium swallow. An initial esophagoscopy showed a diverticulum protruding into the anterolateral wall of the cervical esophagus (Figure 1B). Despite overnight fasting, the diverticular wall was not clearly identified as food debris, was fully impacted inside the diverticular sac. The opening of the esophageal lumen was identified at the posterolateral side of the diverticular opening. Based on the esophagogram and the endoscopic finding, we could diagnose a true KJD. There was no coexisting ZD.
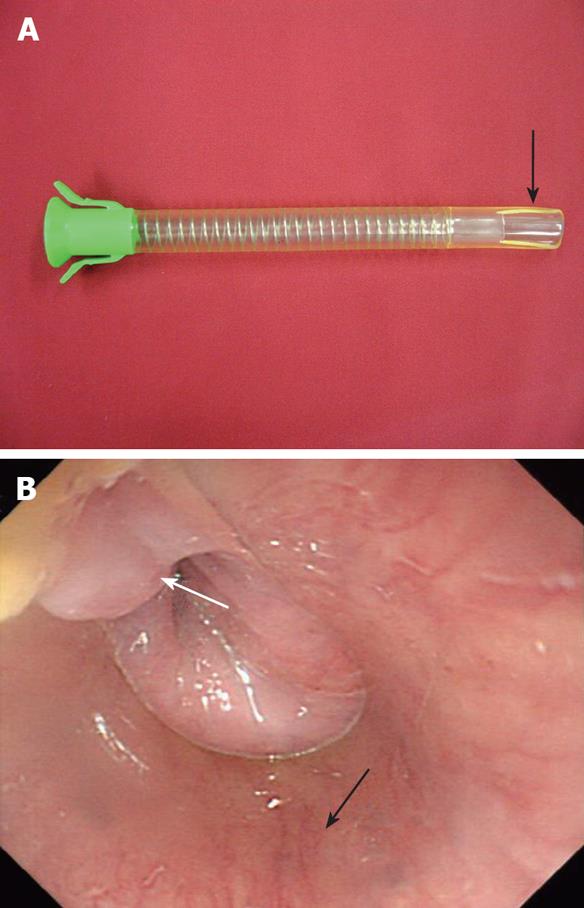
An endoscopic diverticulotomy, with the use of a forward-viewing flexible endoscope (GIF-Q260; Olympus Optical, Tokyo, Japan), was performed on an inpatient basis under conscious sedation with the administration of midazolam and propofol. Informed written consent was obtained before the procedure. In order to obtain good visualization of the tissue bridge of the KJD and to maintain a clear operational field, we used an overtube designed for endoscopic variceal ligation (Flexible Overtube; Sumitomo Bakelite Inc, Tokyo, Japan). Before the procedure, the distal end of an overtube was snipped off with a scissor in a rectangular form (Figure 2A). This ‘fitted’ overtube was advanced into the esophageal lumen under an endoscopic view. The position of the modified distal end of the overtube was adjusted so that it was possible to locate the tissue bridge of the KJD within the hollow rectangle (Figure 2B).
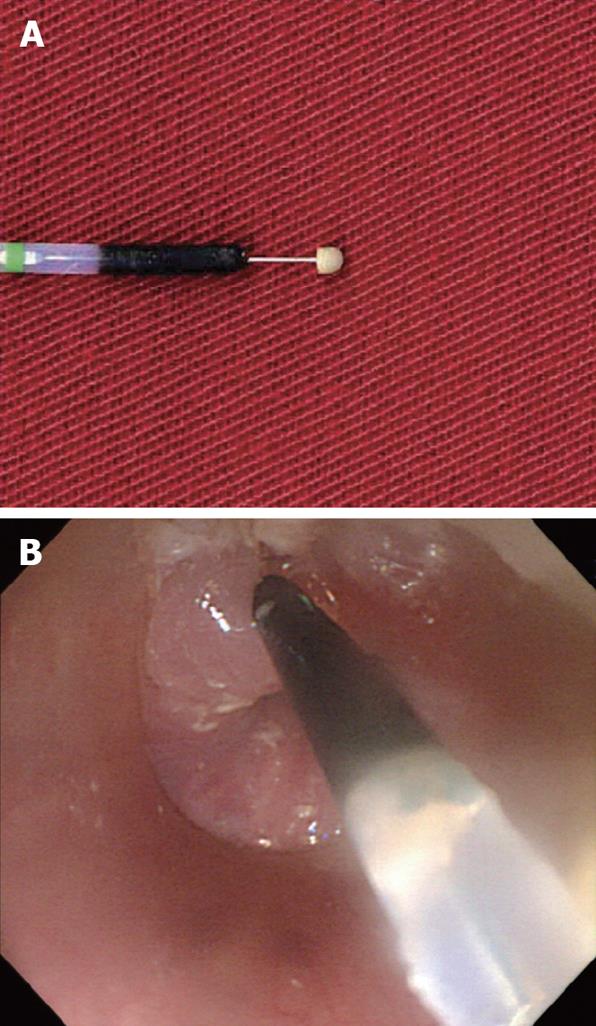
The diverticular sac was not clearly visualized during the procedure due to the presence of impacted food debris. We used an isolated-tip needle-knife papillotome (Iso-Tome, MTW Endoskopie, Wesel, Germany) and Endo-cut (VIO 300D, ERBE, Tübingen, Germany) for dissection of the tissue bridge (Figure 3A). The direction of the cut was from the diverticular lumen towards the esophageal lumen. Dissection of the tissue bridge was performed at its midpoint by direct contact of the needle of the Iso-Tome with the tissue bridge of the diverticulum in a slightly vertical manner (Figure 3B). About three-fourths of the height of the tissue bridge was separated after the dissection. Minor blood oozing developed at the incised wound, but the bleeding was successfully controlled with the use of argon plasma coagulation (APC). The total time of the procedure from insertion of the endoscope to complete hemostasis with APC was 11 min. The patient was discharged two days after the procedure without any procedure-related complications.
A follow up esophagoscopy was performed at three months after the procedure. The esophagoscopy revealed a wide communication between the diverticular sac and the esophageal lumen without a significant tissue bridge (Figure 4). There was no residual food debris inside the diverticular sac and the patient denied having any of the previous symptoms.
A KJD is an uncommon cervical esophageal diverticulum located on the proximal lateral side of the cervical esophagus (also called as proximal lateral cervical diverticulum)[1-4]. Because of the unfamiliarity and rarity of this entity, a KJD is often unrecognized and misdiagnosed as a ZD on an endoscopic finding. Accurate differentiation between a ZD and KJD relies on radiological studies, especially the use of a contrast esophagogram. Unfortunately, we had no initial lateral view of the esophagogram, but we finally confirmed the presence of a KJD after a serial esophagogram and interpretation of the endoscopic findings at our institution. Although the pathogenesis of a KJD is unclear, only surgical treatment has been recommended for a symptomatic KJD due to its close proximity to the recurrent laryngeal nerve and the concern of possible nerve injury[3]. Recently, the use of flexible endoscopic diverticulotomy for the treatment of a symptomatic KJD was introduced by Tang et al[4]. The technique is primarily based upon a needle-knife incision of the esophageal circular muscle under the assistance of an auxiliary transparent hood as reported by the investigators. The investigators recommended that endoscopic management of a symptomatic KJD was designed to widen the opening of the diverticulum and allow subsequent fluent drainage of food material. The basic principle is not different from that for a ZD, to dissect the septum between the diverticular sac and the esophagus and then allow an overflow of food material from the diverticular sac into the esophageal lumen[5]. The aim of performing the diverticulotomy in the present case was the creation of a communication between the diverticular sac and the esophageal lumen for fluent drainage of food debris without retention inside the diverticulum, thereby resolving the patient symptoms.
Endoscopic treatment of the KJD was successful with a good symptomatic resolution in this case. We want to introduce two new devices for a safe diverticulotomy. First, we used an isolated-tip needle-knife papillotome (Iso-Tome) for the dissection of the tissue bridge of the diverticulum instead of a classical needle-knife. The most feared complication of needle-knife based endotherapy of the esophageal diverticula is mediastinitis[6]. The Iso-Tome was originally introduced in our institution for a safe and effective pre-cut papillotomy during an ERCP[7]. The Iso-Tome has a semi-oval shaped isolated-tip made of epoxide adhesive, which prevents electrical leakage from the tip of the incising needle, thereby preventing an unintended deep cut and perforation. This definite merit has been reported for the endoscopic treatment of an intraluminal duodenal diverticulum[8]. The semi-oval shape of the tip is also advantageous for placing the Iso-Tome into a narrow space, such as a diverticular sac filled with impacted food debris. A diverticular sac is not often clearly visualized on endoscopy due to impacted food debris inside the diverticulum. If the depth of the diverticulum is not measured endoscopically, a blind dissection with a needle-knife incision may be associated with overextension beyond the inferior border of the diverticulum and subsequent mediastinitis. In our practice, the Iso-Tome was inserted through the biopsy channel of the endoscope. The tip of the Iso-Tome was intentionally pushed into the gap between the food material and the inner wall of the diverticulum, and was then positioned at the bottom of the diverticulum (Figure 3B). The lower bottom of the diverticulum could be assumed by placement of the Iso-Tome inside the diverticulum before dissection. Another advantage of the use of the Iso-Tome is stable control of the direction of dissection. The dissection with the use of the Iso-Tome is made from the diverticular lumen towards the esophageal lumen. Unintended slippage of the knife on the inner wall of the diverticulum can be prevented by hooking the inner diverticular wall by the shoulder of the semi-oval tip of the Iso-Tome. These advantages suggest that the use of the Iso-Tome is a safe and effective alternative to the use of the classical needle-knife in the treatment of cervical esophageal diverticula.
As a second device, we used a fitted overtube for adequate visualization of the tissue bridge of the diverticulum and protection of the surrounding tissue during dissection of the tissue bridge. Several accessory tools (a nasogastric tube, transparent hood and diverticulosope) have been introduced for flexible endoscopic treatment of cervical esophageal diverticula to overcome technical problems, especially for a ZD[9-12]. All of these accessory tools are commercially available and can be useful for flexible endoscopic treatment of a ZD. In our case, the use of a flexible overtube with a modified distal end allowed clear isolation and better exposure of the tissue bridge within the fixed operational field (Figure 2B). The surrounding esophageal wall, except for the operational field, could be prevented from exposure to unintended electrical damage. Effective stabilization of esophageal motility allowed free movement of the tip of the endoscope inside the overtube. Direct compression of the more proximal esophageal wall by the overtube could prevent aspiration of undigested food debris during the procedure. Modification of the distal end of the overtube was easily adjusted according to the form and size of the diverticular opening before the procedure.
In conclusion, the flexible endoscopic diverticulotomy can be a safe and effective method for the treatment of a symptomatic KJD. We expect that the two new devices can assist a safer and easier flexible endoscopic treatment for any kind of cervical esophageal diverticula, including both a KJD and a ZD.
Peer reviewer: Spiros Sgouros, Naypaktias 5, Agia Paraskevi, Athens 15341, Greece
S- Editor Tian L E- Editor Zheng XM
| 1. | Ekberg O, Nylander G. Lateral diverticula from the pharyngo-esophageal junction area. Radiology. 1983;146:117-122. |
| 2. | Rodgers PJ, Armstrong WB, Dana E. Killian-Jamieson diverticulum: a case report and a review of the literature. Ann Otol Rhinol Laryngol. 2000;109:1087-1091. |
| 3. | Rubesin SE, Levine MS. Killian-Jamieson diverticula: radiographic findings in 16 patients. AJR Am J Roentgenol. 2001;177:85-89. |
| 4. | Tang SJ, Tang L, Chen E, Myers LL. Flexible endoscopic Killian-Jamieson diverticulotomy and literature review (with video). Gastrointest Endosc. 2008;68:790-793. |
| 5. | Mulder CJ, Costamagna G, Sakai P. Zenker's diverticulum: treatment using a flexible endoscope. Endoscopy. 2001;33:991-997. |
| 6. | Vogelsang A, Preiss C, Neuhaus H, Schumacher B. Endotherapy of Zenker's diverticulum using the needle-knife technique: long-term follow-up. Endoscopy. 2007;39:131-136. |
| 7. | Park SH, Kim HJ, Park DH, Kim JH, Lee JH, Lee SH, Chung IK, Kim HS, Kim SJ. Pre-cut papillotomy with a new papillotome. Gastrointest Endosc. 2005;62:588-591. |
| 8. | Lee SH, Park SH, Lee JH, Park DH, Chung IK, Kim SJ, Kim HC. Endoscopic diverticulotomy with an isolated-tip papillotome (Iso-Tome) in a patient with intraluminal duodenal diverticulum. Gastrointest Endosc. 2005;62:817-819. |
| 9. | Hashiba K, de Paula AL, da Silva JG, Cappellanes CA, Moribe D, Castillo CF, Brasil HA. Endoscopic treatment of Zenker's diverticulum. Gastrointest Endosc. 1999;49:93-97. |
| 10. | Sakai P, Ishioka S, Maluf-Filho F, Chaves D, Moura EG. Endoscopic treatment of Zenker's diverticulum with an oblique-end hood attached to the endoscope. Gastrointest Endosc. 2001;54:760-763. |
| 11. | DOHLMAN G, MATTSSON O. The endoscopic operation for hypopharyngeal diverticula: a roentgencinematographic study. AMA Arch Otolaryngol. 1960;71:744-752. |
| 12. | Evrard S, Le Moine O, Hassid S, Devière J. Zenker's diverticulum: a new endoscopic treatment with a soft diverticuloscope. Gastrointest Endosc. 2003;58:116-120. |