Published online Nov 14, 2008. doi: 10.3748/wjg.14.6546
Revised: September 16, 2008
Accepted: September 23, 2008
Published online: November 14, 2008
AIM: To investigate the prognostic value of the model for end-stage liver disease (MELD) and three new MELD-based models combination with serum sodium in decompensated cirrhosis patients-the MELD with the incorporation of serum sodium (MELD-Na), the integrated MELD (iMELD), and the MELD to sodium (MESO) index.
METHODS: A total of 166 patients with decompensated cirrhosis were enrolled into the study. MELD, MELD-Na, iMELD and MESO scores were calculated for each patient following the original formula on the first day of admission. All patients were followed up at least 1 year. The predictive prognosis related with the four models was determined by the area under the receiver operating characteristic curve (AUC) of the four parameters. Kaplan-Meier survival curves were made using the cut-offs identified by means of receiver operating characteristic (ROC).
RESULTS: Out of 166 patients, 38 patients with significantly higher MELD-Na (28.84 ± 2.43 vs 14.72 ± 0.60), iMELD (49.04 ± 1.72 vs 35.52 ± 0.67), MESO scores (1.59 ± 0.82 vs 0.99 ± 0.42) compared to the survivors died within 3 mo (P < 0.001). Of 166 patients, 75 with markedly higher MELD-Na (23.01 ± 1.51 vs 13.78 ± 0.69), iMELD (44.06 ± 1.19 vs 34.12 ± 0.69), MESO scores (1.37 ± 0.70 vs 0.93 ± 0.40) than the survivors died within 1 year (P < 0.001). At 3 mo of enrollment, the iMELD had the highest AUC (0.841), and was followed by the MELD-Na (0.766), MESO (0.723), all larger than MELD (0.773); At 1 year, the iMELD still had the highest AUC (0.783), the difference between the iMELD and MELD was statistically significant (P < 0.05). Survival curves showed that the three new models were all clearly discriminated the patients who survived or died in short-term as well as intermediate-term (P < 0.001).
CONCLUSION: Three new models, changed with serum sodium (MELD-Na, iMELD, MESO) can exactly predict the prognosis of patients with decompensated cirrhosis for short and intermediate period, and may enhance the prognostic accuracy of MELD. The iMELD is better prognostic model for outcome prediction in patients with decompensated cirrhosis.
.
- Citation: Jiang M, Liu F, Xiong WJ, Zhong L, Chen XM. Comparison of four models for end-stage liver disease in evaluating the prognosis of cirrhosis. World J Gastroenterol 2008; 14(42): 6546-6550
- URL: https://www.wjgnet.com/1007-9327/full/v14/i42/6546.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.6546
| 3-mo follow-up | 1-yr follow-up | |||
| Clinical features | Survival group | Death group | Survival group | Death group |
| Age (yr) | 61.2 ± 12.7 | 66.1 ± 13.0a | 60.3 ± 13.0 | 64.8 ± 12.4a |
| Bilirubin (μmol/L) | 44.2 ± 40.1 | 106.2 ± 117.9a | 43.1 ± 43.7 | 77.0 ± 91.0a |
| Creatinine (μmol/L) | 85.5 ± 34.0 | 115.3 ± 67.7a | 82.8 ± 32.2 | 103.8 ± 55.8a |
| INR | 1.64 ± 0.51 | 2.21 ± 1.38a | 1.58 ± 0.49 | 2.00 ± 1.07a |
| Serum sodium (mmol/L) | 137.3 ± 4.9 | 130.4 ± 6.8b | 137.7 ± 5.2 | 133.2 ± 6.3b |
| MELD | 13.2 ± 5.6 | 20.5 ± 10.5b | 8.63 ± 2.13 | 10.5 ± 2.52b |
| MELD-Na | 14.7 ± 6.8 | 28.8 ± 15.0b | 14.2 ± 5.31 | 20.5 ± 9.42b |
| iMELD | 35.5 ± 7.6 | 49.0 ± 10.6b | 34.1 ± 7.5 | 44.1 ± 10.3b |
| MESO | 0.99 ± 0.42 | 1.59 ± 0.82b | 0.93 ± 0.40 | 1.37 ± 0.70b |
The model for end-stage liver disease (MELD) was developed as a prognostic model of short-term mortality in patients with cirrhosis treated with transjugular intrahepatic portosystemic shunt (TIPS)[1]. The scoring system has been widely applied in recent years and shown to predict mortality across a broad spectrum of liver diseases in most studies. But, there is not any parameter correlated with complications of cirrhosis in this formula. Its ability of prognosis is decreased. Some studies have indicated that serum sodium is the independent predictor of mortality in patients with cirrhosis[2,3]. And the incorporation of Na into the MELD may enhance its prognostic accuracy[4,5]. Then some scholars had successively introduced three new mathematical equations based on both MELD and Na, known as the MELD with the incorporation of serum sodium (MELD-Na)[6], the integrated MELD (iMELD) score[7] and the MELD to sodium (MESO) index[8]. In this study, we compared the value of MELD and three new MELD-based models in combination with serum sodium in to evaluate the short-term and intermediate-term prognosis of decompensated cirrhosis patients through retrospective analysis of 166 decompensated cirrhosis cases.
From October, 2005 to May, 2007, 166 patients with decompensated cirrhosis who had been in Department of Gastroenterology of Shanghai East Hospital affiliated to Tongji University were evaluated, and their medical profiles were retrospectively analyzed in this study. The clinical diagnosis was all based on the program of 2000 for the prevention and treatment of virus hepatitis established in Xi’an Congresses[9]. We excluded patients with past or current hepatocellular carcinoma, serious diseases in other systems, admission to hospital repeatedly and incomplete case records. This study included 105 (63.7%) males and 61 (36.3%) females, with mean age 62.3 ± 12.9 (range 29-87) years.
Baseline laboratory results of all the patients obtained at admission (i.e. serum bilirubin, serum creatinine, serum sodium, INR) were retrieved from the medical records. All patients were followed up for 1 year. The outcome was assessed as the 3-, 6- and 12-mo mortality.
All prognostic models were calculated based on laboratory results obtained on the first day of admission. The MELD equation was used to calculate the severity score: 9.6 × loge [creatinine (mg/dL)] + 3.8 × loge [bilirubin (mg/dL)] + 11.2 × loge (INR) + 6.43[10]. The MELD-Na equation was based on the MELD and Na: MELD + 1.59 × (135 - Na)[6], with maximum and minimum Na values of 135 and 120 mmol/L, respectively. The iMELD equation was based on the MELD score, age (years), and Na (mmol/L): MELD + (0.3 × age) - (0.7 + Na) + 100[7]. The MESO index was defined as [MELD/Na (mmol/L)] × 10[8].
All statistical analyses were conducted with the SPSS for Windows version 13 release. Categorical variables were compared by Pearson Chi-squared test and continuous variables were compared by Student’s t-test. To assess the ability of the four MELD-based models in predicting the risk of mortality at 3, 6 and 12 mo, our analysis was performed by the measurement of the c-statistic equivalent to the area under the receiver operating characteristic curve (AUC). The cumulative transplant-free survival at different cut-offs were performed by Kaplan-Meier analysis and compared by log rank test. P < 0.05 was considered statistically significant.
Thirty-eight (22.9%) patients died at 3 mo, and 75 (45.2%) patients died at 1 year. At 3 mo of enrollment, 38 patients with significantly higher MELD-Na (28.84 ± 2.43 vs 14.72 ± 0.60), iMELD (49.04 ± 1.72 vs 35.52 ± 0.67), MESO scores (1.59 ± 0.82 vs 0.99 ± 0.42) compared to the survivors died (P < 0.001). At 1 year of enrollment, 75 patients with markedly higher MELD-Na (23.01 ± 1.51 vs 13.78 ± 0.69), iMELD (44.06 ± 1.19 vs 34.12 ± 0.69), MESO scores (1.37 ± 0.70 vs 0.93 ± 0.40) than the survivors died within 1 year (P < 0.001). The differences of age and serum sodium, two parameters incorporated into three new models, between the survival group and the death group, were also statistically significant at 3 mo and 1 year, especially serum sodium (P < 0.001) (Table 1).
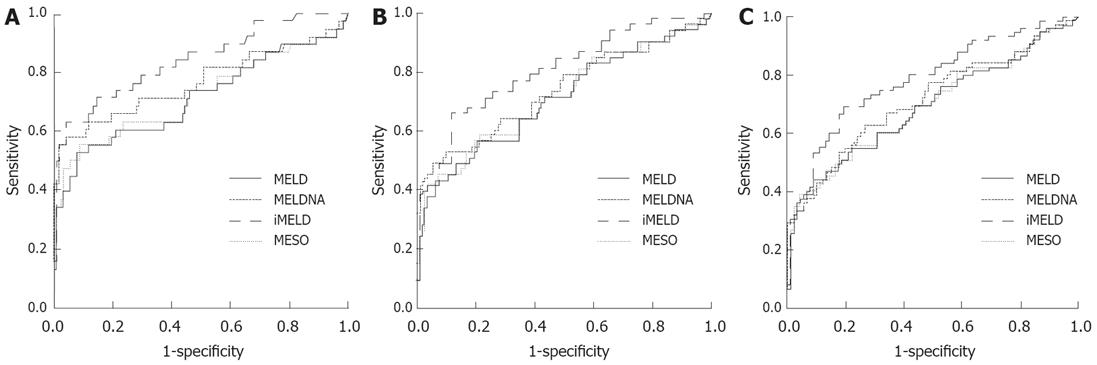
At 3 mo of enrollment, the iMELD had the highest AUC (0.841), followed by the MELD-Na (0.766), MESO (0.723) and MELD (0.712) (Figure 1A). At 6 mo and 1 year, the iMELD still had the highest AUC (0.806 and 0.783, respectively), followed by the MELD-Na (0.738 and 0.714, respectively), MESO (0.715 and 0.694, respectively) and MELD (0.708 and 0.689, respectively) (Figure 1B and C). The iMELD had a significantly higher AUC in comparison with MELD at 3 mo, 6 mo and 1 year (P < 0.05).
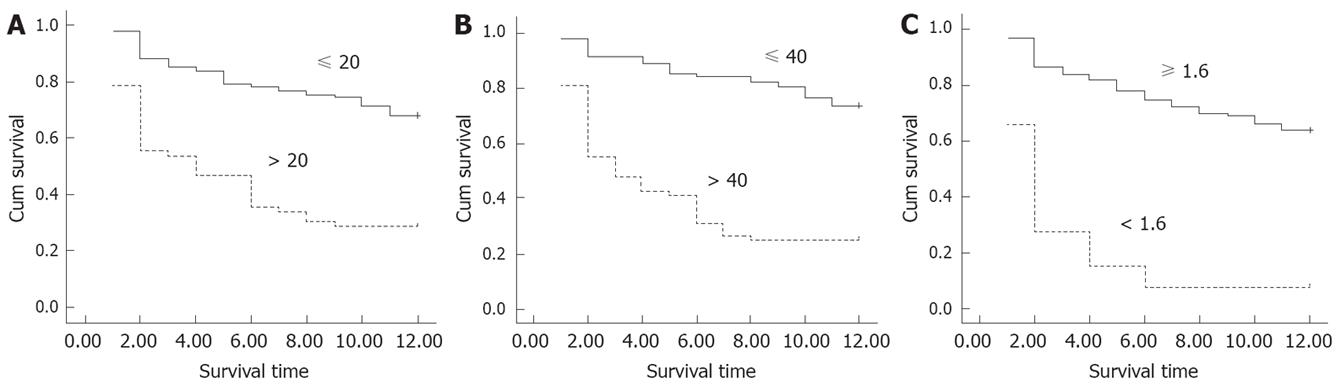
The most discriminative cut-offs from the ROC with the c-statistic and 1 year mortality for MELD-Na, iMELD and MESO were 20, 40 and 1.6, respectively. According to these cut-offs, survival curves are given in Figure 2. The cut-offs of three new models were indicated to discern between the patients who would be survived and dead in 3 mo and 1 year (P < 0.001).
MELD was initially created to predict survival following elective placement of TIPS[1]. The MELD scoring system has been widely applied in recent years and shown to predict mortality across a broad spectrum of liver diseases in most studies[11-14]. MELD has been demonstrated to have a better ability in short-term or intermediate-term outcome prediction in comparison with the Child-Turcotte-Pugh (CTP) system[15-17]. Nonetheless, MELD still has potential limitations[18-21]. Hepatic encephalopathy, esophageal varices bleeding and spontaneous bacterial peritonitis are common complications with cirrhosis, which had been considered one of the allocation policies of liver providing. The patients with these complications all had relatively ideal long-term survival rates. But, there is no parameter correlated with these complications in MELD. Portal hypertension is responsible for above-mentioned complications[22,23]. Hyponatremia is a common event in liver cirrhosis. It develops primarily as a result of free water retention, which is positively correlated with the severity of portal hypertension[24]. Consequently, the serum sodium (SNa) level may inversely reflect the severity of portal hypertension. Those with low MELD scores who have persistent ascites and low SNa are at a disadvantage. This group of patients has a higher mortality than that predicted by the MELD score alone[15]. Many studies have proposed serum sodium can be used to exactly evaluate the prognosis and mortality of patients with cirrhosis, which is objective, quantitative, and reproducible. The incorporation of Na into the MELD may enhance prognostic accuracy[4,5,25].
In 2006, Biggins et al[6] first established “MELD-Na”. Under the new system, a patient with serum Na of 130 mEq/L and a MELD score of 14 will have a “MELD-Na” score of 22 and will be allocated an organ, whereas another patient with serum Na of 135 mEq/L and a MELD score of 20 (“MELD-Na” score of 20) will be given a lower priority. Obviously, the latter patient with a higher MELD score is being given a higher priority under the new system. Thus, this analysis suggests that a significant number of patients with low serum Na will benefit by receiving a priority score corresponding to their mortality risk. Studies in Korea and Hongkong both confirmed that MELD-Na performed better than MELD in predicting 3-mo and 1-year mortality[26,27]. Later, Huo et al[8] developed MESO as MELD to SNa ratio. The AUC was 0.860 for SNa, 0.795 for the MESO index and 0.789 for MELD at 3 mo of enrollment. Among patients with Child-Pugh class A or B, the MESO index had a significantly higher AUC compared with MELD (P < 0.001). In survival analysis, MESO index > 1.6 independently predicted a higher mortality rate (relative risk: 3.32; P < 0001) using the Cox model. The latest study[7] incorporated both serum sodium and age into the new formula: iMELD. The iMELD was better than original MELD in evaluating the mortality of cirrhosis patients 1 year after TIPS: AUC increased by 13.4% and the likelihood ratio statistic from 23.5 to 48.2; it was demonstrated for patients with cirrhosis on the waiting list for liver transplantation by increasing auROC (+8%) and likelihood ratio statistic (from 41.4 to 82.0).
Our study compared MELD with three new MELD-based models containing Na. It is discovered that the AUCs of MELD-Na, iMELD, MESO were all larger than MELD in evaluating the short-term and intermediate-term prognosis of decompensated cirrhosis patients. Among the four models, iMELD had the biggest AUC at different periods and showed significant differences with MELD. The iMELD was demonstrated to be better prognostic model for outcome prediction in patients with cirrhosis, which is similar to that reported by Huo et al[28]. Interestingly, in addition to the MELD and Na, the iMELD also takes into account the factor of age. Age was associated to the risk of mortality as a continuous variable, with older patients having worse survival. The association of aging with mortality in cirrhosis has been shown in the past[29,30]. Most recently, a systematic review of 118 prognostic studies in patients with cirrhosis showed that age is the most important independent prognostic factor of survival[31]. It has been suggested that aging may reflect a longer duration of cirrhosis and a more severe liver disease.
One of the important aspects of the MELD and its derived models is that they are continuous variables and account for the spectrum of disease severity. However, using the most discriminative cut-off from the ROC for different models may provide additional information in certain clinical settings. From the survival curves, it was indicated that the cut-offs of three new models may discern between the patients who would be survived and dead in 3 mo and 1 year. In our study, although the AUCs of MELD-Na and MESO were larger than MELD at 3 mo, 6 mo and 1 year, the comparisons showed no significant differences. The research should be improved more thoroughly and objectively using larger series of patients.
In conclusion, three new models combination with serum sodium (MELD-Na, iMELD, MESO) can all exactly predict the prognosis of patients with decompensated cirrhosis for short and intermediate period, and may enhance the prognostic accuracy of MELD. The iMELD is better prognostic model for outcome prediction in patients with decompensated cirrhosis.
The model for end-stage liver disease (MELD) has been widely applied in recent years and shown to predict mortality across a broad spectrum of liver diseases. But MELD still has potential limitations and its ability of prognosis is decreased. In order to further improve the formula, many researches have been performed recent years.
Some studies have indicated that serum sodium is the independent predictor of mortality in patients with cirrhosis. And the incorporation of Na into the MELD may enhance its prognostic accuracy. Some scholars had successively introduced three new mathematical equations based on both MELD and Na.
Limited data are available for a direct comparison of the performance of the MELD-Na and MELD, and the predictive ability of the other models has not yet been confirmed. In this study, authors compare the short- and intermediate-term prognostic ability of the 4 models-MELD, MELD-Na, iMELD, and MESO index - in a single institute to determine if Na-containing MELD systems have a better predictive accuracy in patients with cirrhosis.
The result of our study showed the prognostic value of the four models for end-stage liver disease. It will provide us the ideal formula which can exactly evaluate the prognosis of cirrhosis in clinic.
The area under a receiver operating characteristic (ROC) curve (AUC) is a commonly used index for summarizing the ability of a continuous diagnostic test to discriminate between healthy and diseased subjects.
This is a good paper with some practical value. The authors investigated the prognostic value of MELD and three new MELD-based models combination with serum sodium in decompensated cirrhosis patients.
Peer reviewer: Jia-Yu Xu, Professor, Shanghai Second Medical University, Rui Jin Hospital, 197 Rui Jin Er Road, Shanghai 200025, China
S- Editor Li DL L- Editor Kumar M E- Editor Ma WH
| 1. | Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, D’Amico G, Dickson ER, Kim WR. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33:464-470. |
| 2. | Wang YW, Huo TI, Yang YY, Hou MC, Lee PC, Lin HC, Lee FY, Chi CW, Lee SD. Correlation and comparison of the model for end-stage liver disease, portal pressure, and serum sodium for outcome prediction in patients with liver cirrhosis. J Clin Gastroenterol. 2007;41:706-712. |
| 3. | Selcuk H, Uruc I, Temel MA, Ocal S, Huddam B, Korkmaz M, Unal H, Kanbay M, Savas N, Gur G. Factors prognostic of survival in patients awaiting liver transplantation for end-stage liver disease. Dig Dis Sci. 2007;52:3217-3223. |
| 4. | Biggins SW, Rodriguez HJ, Bacchetti P, Bass NM, Roberts JP, Terrault NA. Serum sodium predicts mortality in patients listed for liver transplantation. Hepatology. 2005;41:32-39. |
| 5. | Ruf AE, Kremers WK, Chavez LL, Descalzi VI, Podesta LG, Villamil FG. Addition of serum sodium into the MELD score predicts waiting list mortality better than MELD alone. Liver Transpl. 2005;11:336-343. |
| 6. | Biggins SW, Kim WR, Terrault NA, Saab S, Balan V, Schiano T, Benson J, Therneau T, Kremers W, Wiesner R. Evidence-based incorporation of serum sodium concentration into MELD. Gastroenterology. 2006;130:1652-1660. |
| 7. | Luca A, Angermayr B, Bertolini G, Koenig F, Vizzini G, Ploner M, Peck-Radosavljevic M, Gridelli B, Bosch J. An integrated MELD model including serum sodium and age improves the prediction of early mortality in patients with cirrhosis. Liver Transpl. 2007;13:1174-1180. |
| 8. | Huo TI, Wang YW, Yang YY, Lin HC, Lee PC, Hou MC, Lee FY, Lee SD. Model for end-stage liver disease score to serum sodium ratio index as a prognostic predictor and its correlation with portal pressure in patients with liver cirrhosis. Liver Int. 2007;27:498-506. |
| 9. | The societies of communicable diseases and parasitic diseases of Chinese Medical Association. The program for the prevention and treatment of virus hepatitis. Zhonghua Ganzangbing Zazhi. 2000;8:324-329. |
| 10. | Wiesner R, Edwards E, Freeman R, Harper A, Kim R, Kamath P, Kremers W, Lake J, Howard T, Merion RM. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124:91-96. |
| 11. | Dunn W, Jamil LH, Brown LS, Wiesner RH, Kim WR, Menon KV, Malinchoc M, Kamath PS, Shah V. MELD accurately predicts mortality in patients with alcoholic hepatitis. Hepatology. 2005;41:353-358. |
| 12. | Ahmad J, Downey KK, Akoad M, Cacciarelli TV. Impact of the MELD score on waiting time and disease severity in liver transplantation in United States veterans. Liver Transpl. 2007;13:1564-1569. |
| 13. | Huo TI, Wu JC, Lin HC, Lee FY, Hou MC, Lee PC, Chang FY, Lee SD. Evaluation of the increase in model for end-stage liver disease (DeltaMELD) score over time as a prognostic predictor in patients with advanced cirrhosis: risk factor analysis and comparison with initial MELD and Child-Turcotte-Pugh score. J Hepatol. 2005;42:826-832. |
| 14. | Yu JW, Wang GQ, Li SC. Prediction of the prognosis in patients with acute-on-chronic hepatitis using the MELD scoring system. J Gastroenterol Hepatol. 2006;21:1519-1524. |
| 15. | Srikureja W, Kyulo NL, Runyon BA, Hu KQ. MELD score is a better prognostic model than Child-Turcotte-Pugh score or Discriminant Function score in patients with alcoholic hepatitis. J Hepatol. 2005;42:700-706. |
| 16. | Durand F, Valla D. Assessment of the prognosis of cirrhosis: Child-Pugh versus MELD. J Hepatol. 2005;42 Suppl:S100-S107. |
| 17. | Liu F, Xiong WJ, Liu YB. The value of delta model of end stage liver disease in predicting the prognosis of patients with decompensated liver cirrhosis. Zhonghua Xiaohua Zazhi. 2007;27:371-373. |
| 18. | Mishra P, Desai N, Alexander J, Singh DP, Sawant P. Applicability of MELD as a short-term prognostic indicator in patients with chronic liver disease: an Indian experience. J Gastroenterol Hepatol. 2007;22:1232-1235. |
| 19. | Neuberger J. Allocation of donor livers--is MELD enough? Liver Transpl. 2004;10:908-910. |
| 21. | Cholongitas E, Senzolo M, Triantos C, Samonakis D, Patch D, Burroughs AK. MELD is not enough--enough of MELD? J Hepatol. 2005;42:475-477; author reply 478-479. |
| 22. | Bosch J, Garcia-Pagan JC. Complications of cirrhosis. I. Portal hypertension. J Hepatol. 2000;32:141-156. |
| 23. | Ripoll C, Banares R, Rincon D, Catalina MV, Lo Iacono O, Salcedo M, Clemente G, Nunez O, Matilla A, Molinero LM. Influence of hepatic venous pressure gradient on the prediction of survival of patients with cirrhosis in the MELD Era. Hepatology. 2005;42:793-801. |
| 24. | Freeman RB, Wiesner RH, Edwards E, Harper A, Merion R, Wolfe R. Results of the first year of the new liver allocation plan. Liver Transpl. 2004;10:7-15. |
| 25. | Heuman DM, Abou-Assi SG, Habib A, Williams LM, Stravitz RT, Sanyal AJ, Fisher RA, Mihas AA. Persistent ascites and low serum sodium identify patients with cirrhosis and low MELD scores who are at high risk for early death. Hepatology. 2004;40:802-810. |
| 26. | Kim SY, Yim HJ, Lee J, Lee BJ, Kim DI, Jung SW, Han WS, Lee JS, Koo JS, Seo YS. [Comparison of CTP, MELD, and MELD-Na scores for predicting short term mortality in patients with liver cirrhosis]. Korean J Gastroenterol. 2007;50:92-100. |
| 27. | Wong VW, Chim AM, Wong GL, Sung JJ, Chan HL. Performance of the new MELD-Na score in predicting 3-month and 1-year mortality in Chinese patients with chronic hepatitis B. Liver Transpl. 2007;13:1228-1235. |
| 28. | Huo TI, Lin HC, Huo SC, Lee PC, Wu JC, Lee FY, Hou MC, Lee SD. Comparison of four model for end-stage liver disease-based prognostic systems for cirrhosis. Liver Transpl. 2008;14:837-844. |
| 29. | Gines P, Quintero E, Arroyo V, Teres J, Bruguera M, Rimola A, Caballeria J, Rodes J, Rozman C. Compensated cirrhosis: natural history and prognostic factors. Hepatology. 1987;7:122-128. |
| 30. | de Jongh FE, Janssen HL, de Man RA, Hop WC, Schalm SW, van Blankenstein M. Survival and prognostic indicators in hepatitis B surface antigen-positive cirrhosis of the liver. Gastroenterology. 1992;103:1630-1635. |