Published online Nov 7, 2008. doi: 10.3748/wjg.14.6428
Revised: August 16, 2008
Accepted: August 24, 2008
Published online: November 7, 2008
We report port site and distant metastases of unsuspected gallbladder cancer after laparoscopic cholecystectomy diagnosed by positron emission tomography (PET) in two patients. Patient 1, a 72-year-old woman was diagnosed as cholelithiasis and cholecystitis and received laparoscopic cholecystectomy. Unsuspected gallbladder cancer was discovered with histological result of well-differentiated squamous cell carcinoma of the gallbladder infiltrating the entire wall. A PET scan using F-18-fluorodeoxyglucose (FDG-PET) before radical resection revealed residual tumor in the gallbladder fossa and recurrence at port site and metastases in bilateral hilar lymph nodes. Patient 2, a 69-year-old woman underwent laparoscopic cholecystectomy more than one year ago with pathologically confirmed unsuspected adenosquamous carcinoma of stage pT1b. At 7-mo follow-up after surgery, the patient presented with nodules in the periumbilical incision. Excisional biopsy of the nodule revealed adenosquamous carcinoma. The patient was examined by FDG-PET, demonstrating increased FDG uptake in the right lobe of the liver and mediastinal lymph nodes consistent with metastatic disease. This report is followed by a discussion about the utility of FDG-PET in the gallbladder cancer.
- Citation: Hu JB, Sun XN, Xu J, He C. Port site and distant metastases of gallbladder cancer after laparoscopic cholecystectomy diagnosed by positron emission tomography. World J Gastroenterol 2008; 14(41): 6428-6431
- URL: https://www.wjgnet.com/1007-9327/full/v14/i41/6428.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.6428
The vast majority of cholecystectomies are currently performed laparoscopically, and unsuspected gallbladder cancer can be discovered incidentally following 1% of routine cholecystectomies[1]. There is a suspicion that recurrence of the tumor in the abdominal incision is more common after laparoscopic operations. Several possible factors probably involved in the development of such metastases have been proposed[2,3]. Resection of the recurrent malignancy developed in the port sites is warranted, and may lead to survival benefit only when the port site metastases is the only manifestation of recurrent disease. The preoperative accurate evaluation of recurrent gallbladder cancer is essential for reasonable treatment. We report two cases of port site and distant metastases of unsuspected gallbladder cancer after laparoscopic cholecystectomy diagnosed by FDG-PET.
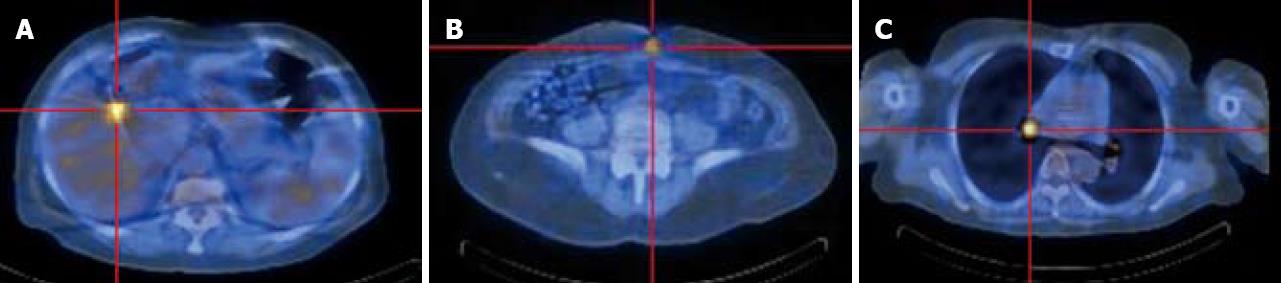
A 72-year-old woman presented with right upper quadrant pain and fever. She had a history of cholelithiasis documented by ultrasound, and intermittent attacks of biliary colic over 2 years. She was diagnosed with cholelithiasis and cholecystitis. She received laparoscopic cholecystectomy and the gallbladder was noted to be edematous and thick-walled, with multiple stones. Histological evaluation revealed an unsuspected well differentiated squamous cell carcinoma of the gallbladder infiltrating the entire wall. More than one month after surgery, she visited our hospital for further radical surgery. Palpable nodules in the periumbilical incision were found by physical examination during admission. A FDG-PET scan was performed, demonstrating increased uptake of the radiopharmaceutical in the gallbladder fossa and periumbilical area as well as bilateral hilar lymph nodes (Figure 1). The lesions were interpreted as residual tumor in the gallbladder fossa and recurrence at port site and metastases in bilateral hilar lymph nodes. Tru-cut biopsy confirmed metastatic squamous cell carcinoma similar to the previous histology. The patient refused further treatment and was discharged.
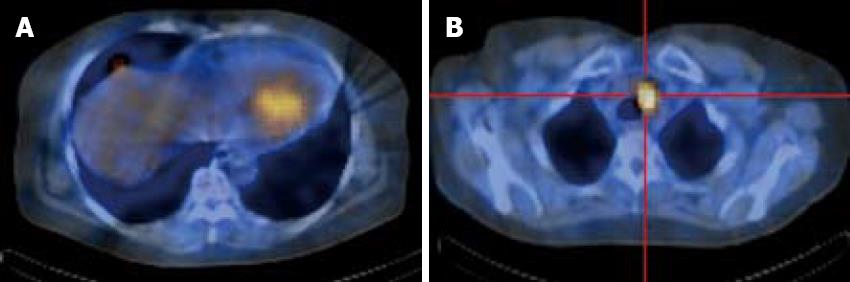
A 69-year-old woman with a history of intermittent right upper quadrant pain over 11 years underwent laparoscopic cholecystectomy more than 1 year ago. The histological examination revealed an unsuspected adenosquamous carcinoma of stage pT1b (tumor invades into muscularis). At 7-mo follow-up after surgery, the patient presented with nodules in the periumbilical incision interpreted as inflammation or postoperative change. The nodule enlarged progressively, and she visited our hospital 19 mo after surgery. Abdominal CT scan revealed a small nodule in the right lobe of the liver, which was difficult to interpret. Excisional biopsy of the nodule in the periumbilical incision was performed and histological examination revealed adenosquamous carcinoma. The patient was examined by FDG-PET, demonstrating increased FDG uptake in the right lobe of the liver and mediastinal lymph nodes consistent with metastatic disease (Figure 2). Chest computed tomography demonstrated enlarged mediastinal lymph nodes consistent with metastases. The patient has subsequently been treated with Gemzar and oxaliplatin with regression of tumor. She died of a non-cancer related cause 4 mo after the second operation.
PET is a noninvasive scanning method to assess metabolism in vivo by means of positron-emitting radiolabeled tracers. This is in contrast with conventional imaging modalities, including ultrasonography (US), computed tomography (CT) and magnetic resonance imaging (MRI) which evaluate structural or anatomical changes[3]. The tracer to measure cellular metabolism commonly used in PET is FDG. FDG is a glucose analogue that is phosphorylated in the cells, but not further metabolized. Most malignant tumors show increased uptake of FDG because malignant transfor-mation and growth of tumor cells is associated with overexpression of glucose transporters and increased hexokinase activity[4].
FDG-PET imaging has been increasingly used to identify and stage various tumors. The majority of these studies show FDG-PET to be superior to traditional imaging in the differential diagnosis of malignancy. This has been particularly notable in the evaluation of recurrent or metastatic disease[5-7]. A few studies have evaluated the use of FDG-PET in the assessment of biliary system tumors or gallbladder carcinoma[4,8-10]. In the study of Anderson et al, nine of 14 gallbladder cancer patients had residual carcinoma at the time of PET[9]. FDG-PET was useful in our cases to delineate recurrent gallbladder cancer, and its extent and had an important clinical impact on the selection of proper treatment. In both cases, FDG-PET detected residual tumor or port site and distant metastatic diseases and changed the surgical plan of radical resection with intent for cure. This report emphasizes that FDG-PET may play an important role in the posttherapy follow-up of gallbladder cancer. Taking the accumulation of FDG in the malignant gallbladder cancer cells into consideration, FDG-PET can be considered as a complementary preoperative staging method. In cases in which it is easy to understaging gallbladder cancer before surgery such as peritoneal seeding, small hepatic metastases, and small regional lymph nodes involvement, FDG-PET may be able to provide important diagnostic information to obtain a correct presurgical staging, and sometimes lead to the change of treatment.
Gallbladder cancer is a relatively rare disease that has no specific symptoms or signs, and the clinical presentations of gallbladder cancer, and gallstone disease are commonly difficult to distinguish. The only effective treatment for carcinoma of the gallbladder is operative resection, and an open technique is preferred. Unfortunately, as is often the case, the lack of presurgical differential diagnosis hampers the planning of surgery. Recently, a few published articles have studied the utility of FDG-PET in gallbladder cancer focusing on not only posttherapy follow-up and preoperative staging, but also the establishment of the benign or malignant natures of gallbladder lesions. Koh et al[10] reported that FDG- PET provided reliable differential diagnoses, identifying gallbladder carcinoma with 75% sensitivity, 87.5% specificity, and 81.3% accuracy. Anderson et al[9] report that the sensitivity of this modality was 78% in their series of 14 gallbladder cancer cases. In the study of Antonio et al, which comprises a series of 16 patients, FDG-PET showed a sensitivity of 0.80, a specificity of 0.82 in diagnosing gallbladder cancer[4]. These studies revealed that FDG-PET can provide important information for establishing the nature of gallbladder lesions especially when in conjunction with conventional modalities.
Because FDG is taken up not only by malignant tumor cells, but also by activated inflammatory cells, benign inflammatory or infectious lesions typically without obvious increase of FDG uptake under some circumstances can produce false positive results[11,12]. The most common reason for false positive FDG-PETs is an inflammatory lesion. Xanthogranulomatous cholecystitis and polypoid lesion with adenomyomatosis are also the common reasons caused false positive result[4,10,11]. PET imaging must be interpreted with caution in patients with known severe inflammatory or granulomatous disease. Nishiyama et al[12] illustrated the relationship between the severity of inflammation and the specificity of PET, and proposed that patients with signs of acute inflammation should be excluded from examination. If the PET scans are performed under conditions with no or low-grade inflammation, an accurate diagnosis of acute or chronic cholecystitis as a benign lesion may be possible.
Although PET was sensitive for the detection of gallbladder cancer, some false negative findings also occurred. The limited sensitivity of FDG-PET for small lesions may have several causes[10,12]. Some factors illustrate the intrinsic limitations of PET resolution for small lesions: activity in small lesions may be underestimated because of the partial-volume effect, movement artifacts caused by nongated breath holding, or physiologic liver FDG uptake. PET scanning performed under suboptimal conditions can also decrease the sensitivity: patient fasting may be too short, and lead to an unnecessarily high liver FDG uptake; the duration of FDG administration and data acquisition may be too short. In diabetic patients, the rate of FDG accumulation in the tumor is decreased, impaired the sensitivity of FDG-PET[10]. In patients with mucinous adenocarcinoma of the gallbladder, a false-negative result has also been reported, probably secondary to poor cellular density[4]. To increase the sensitivity for small lesions, the underestimation due to the partial-volume effect may be reduced by improving the spatial resolution of PET; movement artifacts may be reduced by breath gating of the measurement, and by avoiding reintroduction of the patient to the scanner; PET scanning can be well performed under optimal conditions. Nishiyama et al adopted dual-time-point FDG-PET to evaluate the nature of gallbladder lesions, and demonstrated that delayed FDG-PET was more helpful than early FDG-PET in the evaluation of malignancy, because of the increased uptake by lesions, and the increased lesion-to-background contrast[12]. Recent hybrid PET-CT systems provide structural and functional information simultaneously, and may offer early and accurate staging with an improved specificity[13,14].
In conclusion, despite the relatively small number of gallbladder cancer patients, received FDG-PET scan, this imaging may play an important role in the differential diagnosis, staging, restaging, and posttherapy follow-up of gallbladder cancer.
Peer reviewer: Dr. Yogesh K Chawla, Professor, Department of Hepatology, Postgraduate Institute of Medical Education and Research, Chandigarh 160012, India
S- Editor Zhong XY E- Editor Ma WH
| 1. | Akyurek N, Irkorucu O, Salman B, Erdem O, Sare M, Tatlicioglu E. Unexpected gallbladder cancer during laparoscopic cholecystectomy. J Hepatobiliary Pancreat Surg. 2004;11:357-361. |
| 2. | Lundberg O. Port site metastases after laparoscopic cholecystectomy. Eur J Surg Suppl. 2000;11:27-30. |
| 3. | Lomis KD, Vitola JV, Delbeke D, Snodgrass SL, Chapman WC, Wright JK, Pinson CW. Recurrent gallbladder carcinoma at laparoscopy port sites diagnosed by positron emission tomography: implications for primary and radical second operations. Am Surg. 1997;63:341-345. |
| 4. | Rodriguez-Fernandez A, Gomez-Rio M, Llamas-Elvira JM, Ortega-Lozano S, Ferron-Orihuela JA, Ramia-Angel JM, Mansilla-Rosello A, Martinez-del-Valle MD, Ramos-Font C. Positron-emission tomography with fluorine-18-fluoro-2-deoxy-D-glucose for gallbladder cancer diagnosis. Am J Surg. 2004;188:171-175. |
| 5. | Herder GJ, Kramer H, Hoekstra OS, Smit EF, Pruim J, van Tinteren H, Comans EF, Verboom P, Uyl-de Groot CA, Welling A. Traditional versus up-front [18F] fluorodeoxyglucose-positron emission tomography staging of non-small-cell lung cancer: a Dutch cooperative randomized study. J Clin Oncol. 2006;24:1800-1806. |
| 6. | Wiering B, Krabbe PF, Jager GJ, Oyen WJ, Ruers TJ. The impact of fluor-18-deoxyglucose-positron emission tomography in the management of colorectal liver metastases. Cancer. 2005;104:2658-2670. |
| 7. | Sperti C, Pasquali C, Fiore V, Bissoli S, Chierichetti F, Liessi G, Pedrazzoli S. Clinical usefulness of 18-fluorodeoxyglucose positron emission tomography in the management of patients with nonpancreatic periampullary neoplasms. Am J Surg. 2006;191:743-748. |
| 8. | Wakabayashi H, Akamoto S, Yachida S, Okano K, Izuishi K, Nishiyama Y, Maeta H. Significance of fluorodeoxyglucose PET imaging in the diagnosis of malignancies in patients with biliary stricture. Eur J Surg Oncol. 2005;31:1175-1179. |
| 9. | Anderson CD, Rice MH, Pinson CW, Chapman WC, Chari RS, Delbeke D. Fluorodeoxyglucose PET imaging in the evaluation of gallbladder carcinoma and cholangiocarcinoma. J Gastrointest Surg. 2004;8:90-97. |
| 10. | Koh T, Taniguchi H, Yamaguchi A, Kunishima S, Yamagishi H. Differential diagnosis of gallbladder cancer using positron emission tomography with fluorine-18-labeled fluoro-deoxyglucose (FDG-PET). J Surg Oncol. 2003;84:74-81. |
| 11. | Fletcher JW, Djulbegovic B, Soares HP, Siegel BA, Lowe VJ, Lyman GH, Coleman RE, Wahl R, Paschold JC, Avril N. Recommendations on the use of 18F-FDG PET in oncology. J Nucl Med. 2008;49:480-508. |
| 12. | Nishiyama Y, Yamamoto Y, Fukunaga K, Kimura N, Miki A, Sasakawa Y, Wakabayashi H, Satoh K, Ohkawa M. Dual-time-point 18F-FDG PET for the evaluation of gallbladder carcinoma. J Nucl Med. 2006;47:633-638. |
| 13. | Rodriguez-Fernandez A, Gomez-Rio M, Medina-Benitez A, Moral JV, Ramos-Font C, Ramia-Angel JM, Llamas-Elvira JM, Ferron-Orihuela JA, Lardelli-Claret P. Application of modern imaging methods in diagnosis of gallbladder cancer. J Surg Oncol. 2006;93:650-664. |
| 14. | Casneuf V, Delrue L, Kelles A, Van Damme N, Van Huysse J, Berrevoet F, De Vos M, Duyck P, Peeters M. Is combined 18F-fluorodeoxyglucose-positron emission tomography/computed tomography superior to positron emission tomography or computed tomography alone for diagnosis, staging and restaging of pancreatic lesions? Acta Gastroenterol Belg. 2007;70:331-338. |