Published online Aug 28, 2008. doi: 10.3748/wjg.14.5015
Revised: July 13, 2008
Accepted: July 20, 2008
Published online: August 28, 2008
AIM: To determine the role of scintigraphy in patients with gastrointestinal (GI) bleeding of unknown localization.
METHODS: We performed retrospective analyses on 92 patients receiving scintigraphies from 1993 to 2000 in the University of Regensburg hospital, which were done for localization of GI bleeding as a diagnostic step after an unsuccessful endoscopy. In addition to the scintigraphies, further diagnostic steps such as endoscopy, angiography or operations were performed. In some of the scintigraphies with negative results, a provocation test for bleeding with heparinisation was carried out.
RESULTS: 73% of all scintigraphies showed a positive result. In 4.5% of the positive results, the source was located in the stomach, in 37% the source was the small bowel, in 25% the source was the right colon, in 4.5% the source was the left colon, and in 20% no clear localization was possible. Only 4% of all scintigraphies were false positive. A reliable positive scintigraphy was independent of the age of the examined patient. A provocation test for bleeding with heparin resulted in an additional 46% of positive scintigraphies with a reliable localization in primary negative scintigraphies.
CONCLUSION: Our results show that scintigraphy and scintigraphy with heparin provocation tests are reliable procedures. They enable a reliable localization in about half of the obscure GI-bleeding cases. Scintigraphy is superior to angiography in locating a bleeding. It is shown that even in the age of video capsule endoscopy and double-balloon enteroscopy, scintigraphy provides a reliable and directed localization of GI bleeding and offers carefully targeted guidance for other procedures.
- Citation: Brünnler T, Klebl F, Mundorff S, Eilles C, Reng M, Korn HV, Schölmerich J, Langgartner J, Grüne S. Significance of scintigraphy for the localization of obscure gastrointestinal bleedings. World J Gastroenterol 2008; 14(32): 5015-5019
- URL: https://www.wjgnet.com/1007-9327/full/v14/i32/5015.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.5015
| Characteristics (n = 92) | ||
| Average | Range (%) | |
| Age | 60 | 17-88 |
| Male | 52 | 56.5 |
| Gastrointestinal bleeding without underlying disease | 47 | 51.1 |
| Gastrointestinal bleeding with underlying | 45 | 48.9 |
| disease | ||
| Gastro-intestinal malignancy | 11 | 11.9 |
| Diverticulosis | 5 | 5.4 |
| Acute leukemia | 6 | 6.5 |
| Chronic renal insufficiency | 3 | 3.3 |
| Angiodysplasia | 3 | 3.3 |
| Chronic inflammatory bowel disease | 4 | 4.4 |
| Hepatic cirrhosis | 3 | 3.3 |
| Others | 10 | 11.9 |
| Acute gastro-intestinal bleeding | 55 | 59.8 |
| Chronic gastro-intestinal bleeding | 37 | 40.2 |
| Use of red blood cell concentrates | ||
| ≤ 1 | 70 | 76.1 |
| 2 | 17 | 18.5 |
| ≥ 3 | 5 | 5.4 |
| Provocation test with heparin | 13 | 14.1 |
| Positive | 9 | 9.8 |
| Negative | 4 | 4.4 |
| Intestinoscopies during surgery | 8 | 8.7 |
| With a definite bleeding localization | 2 | 2.2 |
| Without a definite bleeding localization | 6 | 6.5 |
| Mortality | 9 | 10.9 |
| Negative scintigraphy result | Positive scintigraphy result | |
| Total (n = 92) | n = 25 (27.2%) | n = 67 (72.8%) |
| Total time of scintigraphy (h) | 18 (0.75-25) | 19 (1-48) |
| Radioactivity (MBq) | 903 (312-1360) | 975 (486-1300) |
| Gastrointestinal bleeding without underlying disease | 11 (44%) | 36 (54%) |
| Gastrointestinal bleeding with underlying disease | 14 (56%) | 31 (46%) |
| Acute bleeding | 17 (68%) | 38 (57%) |
| Chronic bleeding | 8 (32%) | 29 (43%) |
| Surgery required | 3 (3.3%) | 22 (23.9%) |
| Laboratory values | ||
| Hemoglobin (mg/dL) | 10.1 (6.9-15.5) | 8.6 (3.2-15.6) |
| Platelet count (/dL) | 241 (18-643) | 268 (40-665) |
| PTT (s) | 36.5 (24.2-6.9) | 33.5 (21.2-64.7) |
| Quick (%) | 89 (51-100) | 89 (39-100) |
| Use of red blood cell concentrates | ||
| ≤ 1 | 20 | 50 |
| 2 | 5 | 12 |
| ≥ 3 | 0 | 5 |
Gastrointestinal (GI) bleeding is a common GI disorder that requires an exact localization to guarantee adequate treatment. The clinical presentation ranges from asymptomatic or mild symptoms to a life threatening situation with mortality rates of up to 10%-14%[1-3]. Most deaths are associated with comorbidities and often occur in elderly patients[1,2]. Moreover the incidence of GI bleeding increases with age[3].
GI bleeding is usually categorized by its localization as an upper GI bleeding (originating proximal to the Ligament of Treitz) or a lower GI bleeding (localized distal to the Ligament of Treitz), or must be classified as obscure bleeding if not defined[4]. Dependent on local and on other factors, such as hemodynamic instability or age, different diagnostic steps, including endoscopic, radiological, or nuclear medical methods, must be performed. An example for such a diagnostic algorithm was published by Lee and Laberge 2004[5].
Radionucleotide imaging is one diagnostic possibility for the detection of GI bleeding. Its sensitivity as well as its specificity for bleeding localization seems to be high, with results of 93% to 95% at a rate of 0.04 mL/min for red blood cell (RBC) scans[6]. Its accuracy rises up from 41% to 97% when the results are verified by endoscopy, angiography or surgery[7]. This method offers advantages in being non-invasive, not requiring special preparations for the patient, and detecting both arterial and venous bleeding sites, whereas angiography only detects arterial bleedings. Moreover it offers the capability of imaging over a prolonged period of time. But, as a disadvantage, localization of bleeding sites is often not precise.
In our study we retrospectively evaluated the results of 92 patients requiring scintigraphy with 99mTechnetium (99mTc) labelled red blood cells with special focus on elderly patients, patients with scintigraphy after a provocation test with heparin, and comparison of the results with angiography.
This is a retrospective study performed at a university hospital. By searching the internal medicine databases, 92 patients were identified with the diagnosis GI bleeding of unknown localization who underwent scintigraphy with 99mTc-marked red blood cells as a diagnostic procedure. If a patient required a second hospital stay, it was considered as a new case. Demographic (age, sex) and clinical data (length of hospital stay, underlying diseases if related to bleeding) as well as diagnostic and therapeutic approaches performed were collected by reviewing patient flow charts. Thereby we assessed the time of scintigraphy in relation to the time of first bleeding symptoms. Duration of not more than 7 d was classified as acute bleeding; a bleeding persisting for more than 7 d was classified as chronic bleeding. For laboratory values, we assessed the red blood cell count, and if patients required blood products we evaluated the number of red blood cell units and classified the patients as having received one unit, two units, three or more units.
For negative scintigraphies, a provocation test for bleeding with heparinisation was carried out. Comparative diagnostic or therapeutic procedures following scintigraphy, such as gastroscopy, colonoscopy, angiography, laparoscopy, and computed tomography (CT) scan, were assessed.
For scintigraphy with 99mTc labeled red blood cells, a kit from Nycomed Amersham Sorin Italia, containing 24 mg DTPA, 3.6 mg SnCl2 H2O, 22 mg Sodium-acetate and 9 mg Sodium-chloride, was used. The intravenous 22mTc pertechnetate activity was 1000 MBq. Imaging procedures were performed dynamically during the first hour (one picture every second during the influx period, then one picture per minute until 1 h) with a static image after exactly 1 h. If further images were needed they were performed up to 29 h after the initial application. For imaging procedures, a Siemens Company camera was used as well as an Icon Processing Work Station for reconstructions.
Statistical analyses were performed with SPSS 12.0 statistical software (SPSS inc., Chicago, IL) and Microsoft Excel. Values are shown as total numbers, average or median with range, or as percentages where necessary. Kind support for statistical analyses was given by Metronomia Clinical Research GmbH (Munich, Germany).
From our database, we identified 92 patients with GI bleeding who received scintigraphy as a diagnostic procedure and for whom complete data could be collected. Table 1 shows demographic characteristics, underlying diseases, fractions of acute and chronic bleeding, use of red blood cell units and the need of heparin induced provocation as a further diagnostic step for all 92 patients.
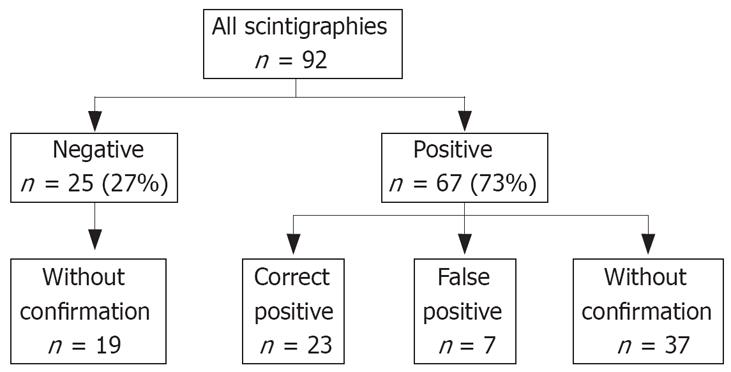
The details of performed scintigraphy in relation to a positive or negative result are shown in Table 2. In 25 patients (27%), there was no evidence of GI bleeding and no further examination or treatment was necessary in 19 patients. In 67 patients (73%), a positive result was found. Verification of the location was performed with further diagnostic procedures, such as gastroscopy, colonoscopy, angiography, computed tomography, and laparoscopy. 23 results were definitively correct and 7 were definitively false. A positive scintigraphy result was not confirmed by further diagnostic procedures in 37 patients (Figure 1).
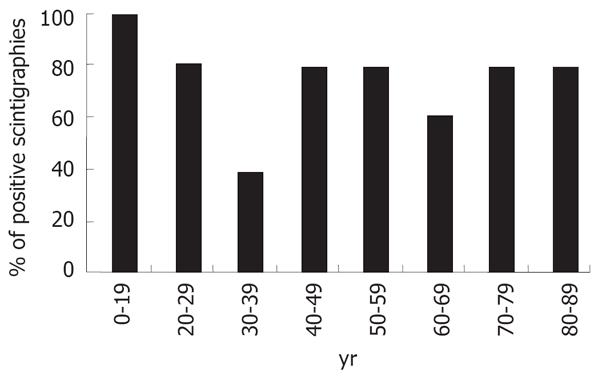
Concerning reliable positive scintigraphies, no significant difference between age-groups was found (Figure 2).
A provocation test with heparin was performed in 13 patients. Five of these patients had previously received a scintigraphy without heparinisation, which was negative in 2 patients, slightly positive in 2 patients, and positive without localization in one patient. The other 8 patients received a heparin-provocated scintigraphy initially in our hospital because they had a negative scintigraphy outside the university hospital. Six (46%) patients had a positive result with localization of the bleeding, 3 (23%) patients showed a positive result without localization, and 4 (31%) patients showed a negative result.
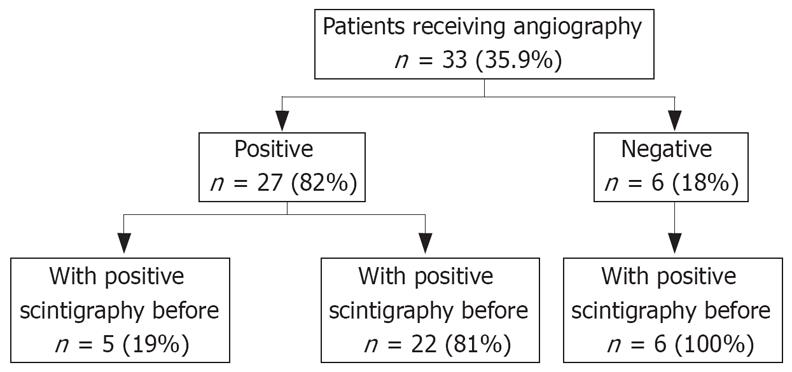
An angiogram was performed in 33 of our 92 patients. 6 patients were negative in both tests. Retrospectively, 1 of these 6 patients showed a false negative result in both of the examinations. Twenty two patients had a negative angiogram, however, 9 of these patients showed a positive scintigraphy result (correct localization in 8 patients and unclear localization in 1 patient). Thirteen patients showed a false positive scintigraphy result. Five patients showed a positive angiogram with positive scintigrams. The localization was correct in 2 patients, unclear in 2 patients and in 1 patient correct in the angiogram but false positive in the scintigram (Figure 3).
Our results showed a sensitivity of 79% (23/29) for the presence of bleeding with scintigraphy, and a specificity of 30% (19/63). The negative predictive value was 76% (19/25), the positive predictive value 77%, including the patients with a positive scintigraphy result without confirmation 34% (23/67).
Nine of 92 patients died. Death occurred due to underlying diseases, which was hemato-oncologic malignancy in 6 patients, sepsis by vasculitis and gangrenous leg in one patient, sepsis and cirrhosis of the liver in one patient, and terminal heart insufficiency due to ischemic cardiomyopathy in one patient.
No death was correlated to the performed scintigraphy, and there were no procedure-associated complications documented. In the subpopulation of patients receiving heparinisation, no patient died. Scintigraphy itself, even with heparin-induced provocation, seems to be a safe procedure.
Scintigraphy with 99mTc labelled red blood cells is a possible tool in the diagnosis of GI bleeding[8-13]. The reported success rates for identifying correct locations of bleeding range from 19% to 96% according to the literature[14-19].
Different reasons may explain the wide range of sensitivities, specifies or accuracies of localizations. In some studies, results were not confirmed by further diagnostic procedures or were confirmed by diagnostic tests, such as barium contrast studies or simple clinical observation, which are not very effective procedures regarding localization of GI bleeding. Therefore, confirmation of scintigraphy results differs in the reported studies making comparisons of results difficult.
In previous studies, focus was on positive results rather than negative results, however, mortality and morbidity due to diagnostic and therapeutic procedures can be controlled by a cautious and well planned surgical approach. It has been shown in this context that a negative result is predictive of a good outcome, and may help in diagnostic risk stratification by avoiding unnecessary emergency care[20]. This fact may also be reflected in our population with 3 out of 25 patients dying in the subpopulation of patients with negative scintigraphy results but with no death correlated with the GI bleeding.
For imaging procedures, we used scintigraphy with 99mTc-labelled red blood cells. Imaging protocols have recently been well described[21-23]. Active bleeding rates greater than 0.3 mL/min can be detected[24] and also some evidence exists that bleeding rates lower than 0.1 mL/min can be detected[25]. In contrast to the erythrocyte labelled method, there is also the possibility of using 99mTc-labelled sulfur colloid scintigraphy. This method, first described in 1977[26], is also a successful tool for identification of bleeding sites, but may be problematic in the detection of bleeding in the stomach, proximal duodenum, or colonic flexures, due to intense radiotracer activity within the liver and the spleen. It has been shown that there is no practical advantage in the use of 99mTechnetium labelled red blood cell scintigraphy over 99mTc-labeled sulfur colloid scintigraphy[27].
Our study has some limitations. One limitation is the study was retrospective within a single centre. Moreover, the patient cohort was mixed in terms of existing underlying diseases.
Our study shows that scintigraphies, as well as scintigraphies with heparin provocation tests, are safe procedures. They enable a reliable localization in about half of the GI bleeding cases. Scintigraphy is, in our setting, superior to angiography and there is evidence that it seems to be a helpful procedure especially for older patients who are restricted concerning invasive procedures. To our knowledge, no literature exists specifically for older patients receiving blood pool scintigraphy.
Even in the era of video capsule endoscopy and double-ballon enteroscopy, we showed that scintigraphy is a safe and helpful diagnostic tool, which allows for safe detection of GI bleeding sites and therefore carefully targeted use of further procedures.
In 30%-35% of all gastrointestinal (GI) bleedings no clear localization of the bleeding site through endoscopy is possible. For further diagnostic steps scintigraphy is a safe method to detect the possible localizations of a so far unknown bleeding.
Blood pool scintigraphy is an established method in the diagnostic of the obscure GI bleeding. Our data show that it is a safe procedure being non-invasive with low-examination-related risks. Further prospective evaluation and correlation with further diagnostic tests as i.e. capsule endoscopy and double-balloon enteroscopy scintigraphy is needed.
It is shown that even in the time of video capsule endoscopy and double-balloon enteroscopy blood pool scintigraphy enables a reliable and directed localization of a GI bleeding and a carefully targeted use of further diagnostic procedures.
These findings may help to optimize the diagnostic approach in patients with an obscure GI bleeding.
The study was a retrospective analysis of 92 patients for patients with unknown intestinal bleeds further leading to unsuccessful endoscopy. The significance of scintigraphy is under evaluation and this paper helps to bring focus on this issue particularly as there is presently a limited ability to detect GI bleeding.
Peer reviewer: Phillip S Oates, PhD, Department of Physiology, School of Biomedical and Chemical Sciences, the University of Western Australia, Perth, Western Australia 6009, Australia
S- Editor Li DL L- Editor Lutze M E- Editor Yin DH
| 1. | Longstreth GF. Epidemiology and outcome of patients hospitalized with acute lower gastrointestinal hemorrhage: a population-based study. Am J Gastroenterol. 1997;92:419-424. |
| 2. | Longstreth GF. Epidemiology of hospitalization for acute upper gastrointestinal hemorrhage: a population-based study. Am J Gastroenterol. 1995;90:206-210. |
| 3. | Palmer K. Management of haematemesis and melaena. Postgrad Med J. 2004;80:399-404. |
| 4. | Zuckerman GR, Prakash C, Askin MP, Lewis BS. AGA technical review on the evaluation and management of occult and obscure gastrointestinal bleeding. Gastroenterology. 2000;118:201-221. |
| 5. | Lee EW, Laberge JM. Differential diagnosis of gastrointestinal bleeding. Tech Vasc Interv Radiol. 2004;7:112-122. |
| 6. | Zuckier LS. Acute gastrointestinal bleeding. Semin Nucl Med. 2003;33:297-311. |
| 7. | Zuckerman GR, Prakash C. Acute lower intestinal bleeding: part I: clinical presentation and diagnosis. Gastrointest Endosc. 1998;48:606-617. |
| 8. | Bearn P, Persad R, Wilson N, Flanagan J, Williams T. 99mTechnetium-labelled red blood cell scintigraphy as an alternative to angiography in the investigation of gastrointestinal bleeding: clinical experience in a district general hospital. Ann R Coll Surg Engl. 1992;74:192-199. |
| 9. | Dusold R, Burke K, Carpentier W, Dyck WP. The accuracy of technetium-99m-labeled red cell scintigraphy in localizing gastrointestinal bleeding. Am J Gastroenterol. 1994;89:345-348. |
| 10. | Emslie JT, Zarnegar K, Siegel ME, Beart RW Jr. Technetium-99m-labeled red blood cell scans in the investigation of gastrointestinal bleeding. Dis Colon Rectum. 1996;39:750-754. |
| 11. | Garofalo TE, Abdu RA. Accuracy and efficacy of nuclear scintigraphy for the detection of gastrointestinal bleeding. Arch Surg. 1997;132:196-199. |
| 12. | Hunter JM, Pezim ME. Limited value of technetium 99m-labeled red cell scintigraphy in localization of lower gastrointestinal bleeding. Am J Surg. 1990;159:504-506. |
| 13. | Leitman IM, Paull DE, Shires GT 3rd. Evaluation and management of massive lower gastrointestinal hemorrhage. Ann Surg. 1989;209:175-180. |
| 14. | Nicholson ML, Neoptolemos JP, Sharp JF, Watkin EM, Fossard DP. Localization of lower gastrointestinal bleeding using in vivo technetium-99m-labelled red blood cell scintigraphy. Br J Surg. 1989;76:358-361. |
| 15. | O'Neill BB, Gosnell JE, Lull RJ, Schecter WP, Koch J, Halvorsen RA, Harris HW. Cinematic nuclear scintigraphy reliably directs surgical intervention for patients with gastrointestinal bleeding. Arch Surg. 2000;135:1076-1081; discussion 1081-1082. |
| 16. | Orecchia PM, Hensley EK, McDonald PT, Lull RJ. Localization of lower gastrointestinal hemorrhage. Experience with red blood cells labeled in vitro with technetium Tc 99m. Arch Surg. 1985;120:621-624. |
| 17. | Rantis PC Jr, Harford FJ, Wagner RH, Henkin RE. Technetium-labelled red blood cell scintigraphy: is it useful in acute lower gastrointestinal bleeding? Int J Colorectal Dis. 1995;10:210-215. |
| 18. | Suzman MS, Talmor M, Jennis R, Binkert B, Barie PS. Accurate localization and surgical management of active lower gastrointestinal hemorrhage with technetium-labeled erythrocyte scintigraphy. Ann Surg. 1996;224:29-36. |
| 19. | Van Geelen JA, De Graaf EM, Bronsveld W, Boer RO. Clinical value of labeled red blood cell scintigraphy in patients with difficult to diagnose gastrointestinal bleeding. Clin Nucl Med. 1994;19:949-952. |
| 20. | Zettinig G, Staudenherz A, Leitha T. The importance of delayed images in gastrointestinal bleeding scintigraphy. Nucl Med Commun. 2002;23:803-808. |
| 21. | Maurer AH. Gastrointestinal bleeding and cine-scintigraphy. Semin Nucl Med. 1996;26:43-50. |
| 22. | McKusick KA, Froelich J, Callahan RJ, Winzelberg GG, Strauss HW. 99mTc red blood cells for detection of gastrointestinal bleeding: experience with 80 patients. AJR Am J Roentgenol. 1981;137:1113-1118. |
| 23. | Winzelberg GG, Froelich JW, McKusick KA, Strauss HW. Scintigraphic detection of gastrointestinal bleeding: a review of current methods. Am J Gastroenterol. 1983;78:324-327. |
| 24. | Winzelberg GG, McKusick KA, Strauss HW, Waltman AC, Greenfield AJ. Evaluation of gastrointestinal bleeding by red blood cells labeled in vivo with technetium-99m. J Nucl Med. 1979;20:1080-1086. |
| 25. | Thorne DA, Datz FL, Remley K, Christian PE. Bleeding rates necessary for detecting acute gastrointestinal bleeding with technetium-99m-labeled red blood cells in an experimental model. J Nucl Med. 1987;28:514-520. |
| 26. | Alavi A, Dann RW, Baum S, Biery DN. Scintigraphic detection of acute gastrointestinal bleeding. Radiology. 1977;124:753-756. |
| 27. | Ponzo F, Zhuang H, Liu FM, Lacorte LB, Moussavian B, Wang S, Alavi A. Tc-99m sulfur colloid and Tc-99m tagged red blood cell methods are comparable for detecting lower gastrointestinal bleeding in clinical practice. Clin Nucl Med. 2002;27:405-409. |