Published online Aug 14, 2008. doi: 10.3748/wjg.14.4823
Revised: July 7, 2008
Accepted: July 14, 2008
Published online: August 14, 2008
Biliary rhabdomyosarcoma (BRMS) is an uncommon childhood malignancy which has been managed surgically. We present a case of a 3-year-old boy with BRMS, in whom endoscopic retrograde cholangiopancreatography (ERCP) was successfully used both diagnostically and therapeutically, thus obviating the need for surgery and its attendant risks of morbidity and mortality. We conclude that ERCP is an effective alternative to surgery for BRMS in some patients.
- Citation: Himes RW, Raijman I, Finegold MJ, Russell HV, Fishman DS. Diagnostic and therapeutic role of endoscopic retrograde cholangiopancreatography in biliary rhabdomyosarcoma. World J Gastroenterol 2008; 14(30): 4823-4825
- URL: https://www.wjgnet.com/1007-9327/full/v14/i30/4823.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.4823
Biliary rhabdomyosarcoma (BRMS) is an uncommon cause of recurrent jaundice and conjugated hyperbi-lirubinemia in children. Because its presentation may mimic that of a choledochal cyst, the correct diagnosis is frequently made intraoperatively at a planned choledochal cystectomy. However, identification of this entity prior to surgery is important because early surgery may carry excess morbidity and mortality. We present a patient with BRMS in whom therapeutic endoscopy was used successfully as an adjunct to chemotherapy and radiotherapy.
A 3-year-old African American boy was referred to our center with a 1-wk history of scleral icterus, pruritus and light-colored diarrhea. His medical history included a self-limited episode of scleral icterus accompanied by diarrhea 1 mo earlier. His family history was unremarkable. Examination revealed a well-developed, healthy-appearing child. His abdomen was non-distended, the liver was soft and palpable 6 cm beneath the right costal margin without splenomegaly.
Laboratory investigations showed serum aspartate aminotransferase (AST) 391 U/L (20-60 U/L), alanine aminotransferase (ALT) 269 U/L (5-45 U/L), alkaline phosphatase (AP) 2 759 U/L (145-320 U/L), gamma-glutamyl transferase (GGT) 704 U/L (6-19 U/L), unconjugated bilirubin (UCB) 0.5 mg/dL (< 1 mg/dL), conjugated bilirubin (CB) 1.3 mg/dL (< 0.35 mg/dL) and international normalized ratio (INR) 0.9 (0.9-1.1). Hepatitis A, B and C serologies and stool studies were negative; amylase and lipase were normal.
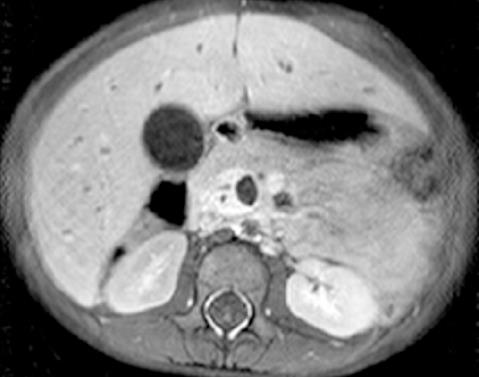
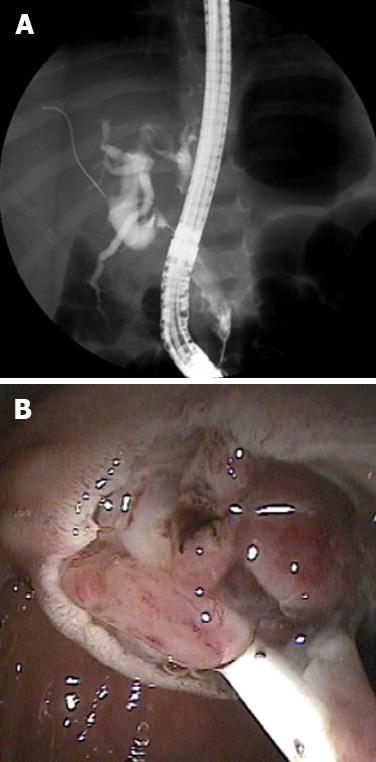
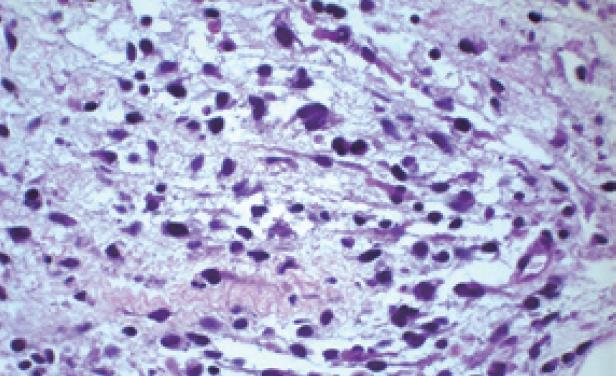
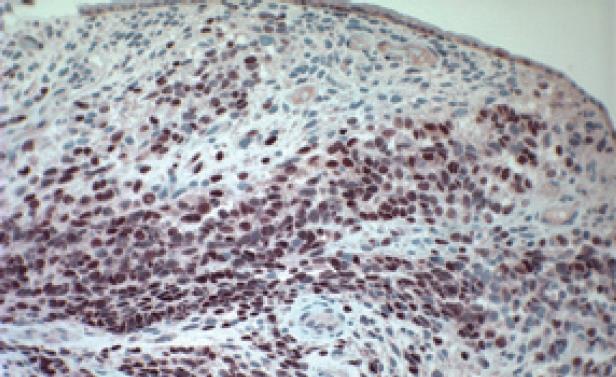
Abdominal ultrasound revealed dilated intrahepatic and extrahepatic bile ducts and a dilated gallbladder without stones, which was suspicious for a choledochal cyst. Abdominal magnetic resonance imaging (MRI) showed an enhancing soft-tissue mass (5.8 cm × 2 cm × 1.5 cm) within the common bile duct (CBD) suggestive of BRMS (Figure 1). No intra-abdominal lymphadenopathy was present. The patient underwent (ERCP) to obtain tissue for diagnostic confirmation and for placement of a biliary stent. Filling defects were present on opacification of the biliary tree (Figure 2A) and sphincterotomy of the boggy ampulla revealed a protuberant fleshy mass (Figure 2B). Histology showed poorly differentiated round to stellate-shaped neoplastic cells in a myxoid stroma consistent with rhabdomyosarcoma of the botryoid subtype (Figure 3). Immunohistochemical stains for myogenin (Figure 4) and MyoD1 were positive. Chest computed tomography, whole body bone scan and bone marrow examination were unremarkable and a venous access device was placed to commence chemotherapy with vincristine, actinomycin-D and cyclophosphamide.
After 12 wk of chemotherapy the patient was anicteric and the tumor was undetectable by MRI, so the biliary stent was removed. At this endoscopy a repeat biopsy was obtained at the tumor bed which was histologically consistent with BRMS. Based on persistent disease, a radiation dose of 50.4 Gy was subsequently delivered to the tumor bed. The patient has completed therapy without significant complications.
Although it is the most common biliary tumor in children, BRMS comprises only about 1% of all rhabdomyosarcomas[1-3]. BRMS usually arises in the CBD, but may originate from anywhere along the biliary tree. Positive regional lymph nodes or distant metastases were present at diagnosis in nearly 25% of children in one series[4]; and hepatic, pulmonary, peritoneal and bone metastases have been described.
Median age at presentation is 3 years and males are affected more often than females[1]. Presenting signs and symptoms include jaundice, scleral icterus, pruritus, acholic stools and abdominal pain or distention. Fever, vomiting, diarrhea, malaise and anorexia occur less frequently.
Laboratory evaluation of patients reveals AP and gamma glutamyl-transferase elevation out of proportion to transaminases and a variable increase in CB depending on the extent of biliary obstruction. As in our patient, imaging shows a dilated biliary tree and may demonstrate an obstructive soft-tissue density.
Treatment protocols developed by the Soft Tissue Sarcoma Committee of the Children’s Oncology Group, formerly the Intergroup Rhabdomyosarcoma Study Group (IRSG), stratify patients according to the site and size of the tumor, histologic subtype, degree of surgical resection and presence or absence of nodal disease or distant metastases. Although early case series advocated primary surgical resection together with chemotherapy and radiotherapy, a review by Spunt and colleagues[4] described the clinical features and outcomes of 25 children with BRMS and questioned the necessity of aggressive surgical excision for patients with tumors in this primary site. In their series, only six patients underwent gross tumor resections, of which, only two resulted in negative margins. In spite of residual tumor burden, however, 92% of patients who survived post-operatively remained disease-free. Moreover, they found that complications were more frequent in patients who underwent primary resection, these included ascending cholangitis, peritonitis, small bowel obstruction and peptic ulcer disease. The estimated five-year survival for all patients with BRMS in this study was 66%; patients with local/regional disease fared better with 78% survival at five years[4].
BRMS is a rare malignancy of childhood that presents with clinical and radiographic evidence that can mimic choledochal cysts. With highly effective chemotherapy, ERCP is an important diagnostic and therapeutic modality that may obviate the need for early and aggressive surgery in patients with BRMS.
Peer reviewer: J Michael Millis, PhD, Department of Surgery, University of Chicago, 5841 S. Maryland Avenue, MC 2027, Chicago 60637, United States
S- Editor Li DL L- Editor Ma JY E- Editor Yin DH
| 1. | Kebudi R, Gorgun O, Ayan I, Cosar R, Bilgic B. Rhabdomyosarcoma of the biliary tree. Pediatr Int. 2003;45:469-471. |
| 2. | Zampieri N, Camoglio F, Corroppolo M, Cecchetto M, Ornis S, Ottolenghi A. Botryoid rhabdomyosarcoma of the biliary tract in children: a unique case report. Eur J Cancer Care (Engl). 2006;15:463-466. |
| 3. | Roebuck DJ, Yang WT, Lam WW, Stanley P. Hepatobiliary rhabdomyosarcoma in children: diagnostic radiology. Pediatr Radiol. 1998;28:101-108. |
| 4. | Spunt SL, Lobe TE, Pappo AS, Parham DM, Wharam MD Jr, Arndt C, Anderson JR, Crist WM, Paidas C, Wiener E. Aggressive surgery is unwarranted for biliary tract rhabdomyosarcoma. J Pediatr Surg. 2000;35:309-316. |