Published online Jul 28, 2008. doi: 10.3748/wjg.14.4569
Revised: June 16, 2008
Accepted: June 23, 2008
Published online: July 28, 2008
AIM: To investigate the etiology, diagnosis and treatment of spontaneous perforation of the colon.
METHODS: The clinical data of 10 cases of spontaneous perforation of the colon, observed at Fuding hospital from January 2004 to December 2007, were analyzed retrospectively.
RESULTS: The mean age at onset was 65 years (range from 45 to 73). Seven patients had a history of chronic constipation. All patients complained of sudden lower abdominal pain. The perforation occurred after coloclysis and administration of senna leaves in two patients. Nine patients had signs of peritoneal irritation. Seven cases underwent abdominal paracentesis, which was diagnostic in six. Only one case was definitely diagnosed prior to surgery. One patient underwent neoplasty of the colon, another a partial resection of colon, six a neoplasty of the colon plus sigmoid colostomy, and two underwent Hartmann surgery. All perforation sites were opposite to the mesenteric edge. The perforation sites were located on descending colon in one case, sigmoid colon in three cases, and rectosigmoid colon in six cases. In five patients, surgical pathological examination was consistent with the microscopical changes of colonic perforation caused by feces. Three patients died after surgery.
CONCLUSION: Spontaneous perforation of the colon most commonly occurs among the elderly with chronic constipation. Abdominal paracentesis is helpful for the diagnosis. The perforation site is located opposite to the mesenteric edge. Sigmoid colon and rectosigmoid colon are the most frequent locations. Neoplasty of the colon and sigmoid colostomy are the most frequent treatment. The prognosis is bad and the mortality rate after surgery is high.
- Citation: Yang B, Ni HK. Diagnosis and treatment of spontaneous colonic perforation: Analysis of 10 cases. World J Gastroenterol 2008; 14(28): 4569-4572
- URL: https://www.wjgnet.com/1007-9327/full/v14/i28/4569.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.4569
Spontaneous perforation of the colon is defined as a sudden perforation of the normal colon in the absence of diseases such as tumors, diverticulosis or external injury[1]. It is rare, often misdiagnosed and has a high mortality rate. It is seldom reported in the literature. In this study, we collected 10 cases of such patients during 2004 to 2007, and analyzed their clinical features in order to improve the understanding of this disease. The present study may be helpful for the diagnosis and treatment of spontaneous colonic perforation.
Ten cases of spontaneous perforation of the colon were collected at Fuding hospital from January 2004 to December 2007. The clinicopathological data, including gender, age, past history, symptoms, physical examination, diagnostic assays, pathological examination and surgical information as well as outcome were analyzed retrospectively to assess the diagnosis and treatment.
There were 8 males and 2 females. The mean age at onset of the disease was 65 years (range, 45 to 73). Seven patients had a history of chronic constipation. All patients reported a sudden lower abdominal pain. Three patients had a history of oral administration of nonsteroid anti-inflammatory drugs (NSAIDs) to relieve abdominal pain. Five patients had possible correlated factors: in three, onset occurred after defecation and in the other two it did after coloclysis and administration of senna leaves. Three patients had symptoms compatible with shock prior to surgery. Physical examination showed signs of peritoneal irritation in 9 cases, with tension of all abdominal muscles, tenderness and rebound tenderness. The abdominal X-ray did not reveal any abnormal findings in 4 patients. Seven patients underwent diagnostic abdominal paracentesis. Feculent material was aspirated in six patients. Only one patient was definitely diagnosed before surgery. Five patients were misdiagnosed as having gastric or duodenal perforation, colorectal tumor in two other cases, acute gangrenous perforating appendicitis in one case and acute pancreatitis in one case.
All patients underwent emergency surgical intervention. The time interval between onset and surgery ranged from 15 to 96 h. Seven patients underwent surgery 6 h after hospital admission. One patient underwent neoplasty of the colon, one a partial resection of the colon, six a neoplasty of the colon plus a sigmoid colostomy, and two had Hartmann surgery. All perforation sites were opposite to the mesenteric edge and were located on the descending colon in one case, the sigmoid colon in three, and the rectosigmoid colon in the remaining six.
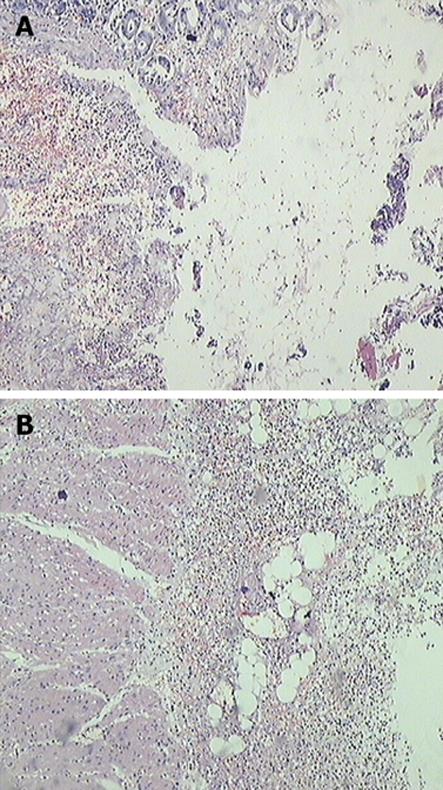
Five patients had surgical pathological examination. Macroscopic examination showed that the perforation sites were all located opposite to the mesenteric edge, had circular shape, and ranged from 2 to 3 cm in diameter. Microscopic examination showed necrosis of the whole wall of the colon. The perforation site was characterized at its surface by inflammatory sphacelus. Granulation tissue grew from the bottom. Submucosal edema, diffuse hemorrhage and abundant neutrophil infiltration were found in the surrounding colonic mucosa, consistent with the microscopical changes typical of colonic perforation caused by feces (Figure 1).
Three patients died after surgery because of multiple organ failure caused by septic shock. The other seven patients survived and six patients who received neoplasty and sigmoid colostomy underwent another surgical intervention to close the stoma 3 months thereafter.
The cause of spontaneous colonic perforation is usually unclear. In general, colonic perforation caused by feces is the most frequent occurrence. The disease has often been seen in patients with chronic constipation. In these cases, the solid feculent mass compresses the colonic wall, diminishes the blood supply and leads to ischemia and necrosis of colonic mucosa, which forms marked feculent ulcer changes. The ulcer might lead to colonic rupture in some cases[2–5]. Maurer et al[3] have proposed the diagnostic criteria of feculent colonic perforation: (1) Rounded shape, more than 1 cm in diameter; (2) The colon is full of stool, which diffuses to the abdominal cavity through the perforation; (3) Ischemia and necrosis of colonic mucosa leading to feculent ulcer and acute inflammatory reaction surrounding the perforation site can be seen at microscopical examination; (4) External injury or other diseases such as obstruction, tumors and diverticulosis must be excluded. All five cases with pathological examination were consistent with the above criteria. Maurer et al[3] also proposed that the feculent ulcer may present at multiple sites. The proportion of cases with multiple ulcers in the same colonic segment is about 28%.
Another cause is idiopathic colonic perforation. The pressure within the colonic lumen increases and distributes asymmetrically, leading to an excess pressure increase at the level of the angle[6]. The colonic wall is hyperdilated, becomes excessively thin and the perforation occurs. Compared to feculent perforation, idiopathic colonic perforation has the following features: (1) The perforation is linear; (2) Feculent ulcer cannot be seen at microscopic examination. The mucosal edge is clear and does not extend to the serosa. The broken ends of the muscular layer are regular[7]. Although these two conditions are different both macroscopically and microscopically, they are occasionally difficult to distinguish at surgery. Surgical pathological examination is necessary to make a definite diagnosis[7].
The most frequent location is opposite to the mesenteric edge of the sigmoid colon and recto-sigmoid colon. Maurer et al[3] reported that 52 out of 81 cases (64%) of feculent perforation occurred at the above sites. In the study of Kasahara et al, 68% (44/65) of idiopathic colonic perforation were located at those sites[7]. In the present study, 9 patients had the same characteristics. This phenomenon may be due to the special physiological and anatomical features of sigmoid colon. There is no ramus anastomoticus between the lowest branch of sigmoid arteries and the superior rectal artery, which causes a physiological ischemia. When some stiff stool goes through sigmoid colon, the colonic wall is compressed and leads to the hindrance of blood supply. The blood supply to the opposite side of the mesentery is poor. The stool is more likely to stay in the rectosigmoid colon because of the confined colonic cavity. The smooth muscle contracts, which leads to the increase of the pressure of colonic cavity[8–12].
This disease is more frequent in the elderly and the mean age at onset is more than 60. About 61% to 81% of patients had constipation history[24]. It is often misdiagnosed because doctors are unaware about this disease. Only 10% of patients are definitely diagnosed prior to surgery[6]. In the present study, only one patient (1/10) was definitely diagnosed before surgery. It is very important to increase the awareness about this disease in order to improve the accuracy of diagnosis. We think that the possibility of this disease should be taken into consideration in elderly patients who have chronic constipation, when they have a history of induction of increased intra-abdominal pressure, present with sudden abdominal pain spreading to the whole abdomen and have peritoneal irritation signs[1314]. In this study, the abdominal paracentesis was diagnostic in 6 out of 7 patients. Therefore, abdominal paracentesis is a valuable tool for the diagnosis of patients with this complication[15].
The mortality rate of this disease is as high as 35% to 47%[27]. In case of perforation, innumerable bacteria spread from the colon into the abdominal cavity and cause acute diffuse peritonitis. Bacterial toxins are absorbed and lead to infectious shock and then multiple organ failure. So, patients should undergo surgery as soon as the disease is definitely diagnosed[16–20]. The types of surgery are different depending on the time of onset, degree of peritonitis, general physical condition and lesion of the colon. The following types of surgery are common: neoplasty, colostomy, neoplasty plus proximal colostomy, Hartmann surgery[21–23]. Neoplasty plus proximal colostomy is the most popular since it is safe and time-sparing. Six patients underwent neoplasty plus proximal colostomy in the present study. Serpell et al[2] found that the mortality and complication rates after Hartmann surgery were lower than in case of other operations because Hartmann surgery dissects the affected colon. Maurer et al[3] proposed that feculent ulcer had multiple origins and, therefore, other segments of the colon should be explored during the operation. If the colonic wall is dilated or thinner, it should be resected. Subtotal colectomy may be essential for some cases, which can spare time-consuming coloclysis during the operation and avoid possible later re-perforation of the affected colon[2425].
Spontaneous colonic perforation is noteworthy due to its high mortality rate. The possibility of this disease should be taken into consideration in elderly patients having chronic constipation and bed-ridden for long periods of time. Doctors should be careful when administering enema and cathartics.
Spontaneous perforation of the colon most commonly occurs in the elderly, is usually misdiagnosed before surgery and leads to a high mortality rate after surgery. Early correct diagnosis, early surgery and appropriate surgical treatment options are the key to improve the prognosis. Effective measures should be carried out to prevent this disease in high-risk patients. This study may help the surgeon to recognize this rare entity.
This article focuses on a rare disease, i.e. acute abdomen due to spontaneous perforation of the colon. It is helpful to increase awareness about spontaneous perforation of the colon.
It is very important to increase the knowledge about this disease in order to improve the diagnostic accuracy. The authors think that the diagnosis of this disease should be considered in elderly patients with chronic constipation, who induce an increase of the intra-abdominal pressure, present with sudden abdominal pain spreading to the whole abdomen and have signs of peritoneal irritation. In this study, the results of abdominal paracentesis were positive for 6 out of 7 patients. Therefore, abdominal paracentesis is valuable for the diagnosis of patients with this complication.
The spontaneous colonic perforation should be correctly diagnosed, due to its high mortality rate. Doctors should be careful when administering enema and cathartics.
This is an interesting series of patients with a rare condition. The authors performed a single study center report of 10 patients. They analyzed the clinicopathological data retrospectively and assessed the diagnostic procedures and the treatment. In addition, they point out to surgeons the importance of recognizing this rare cause of acute abdomen with a high mortality rate.
| 1. | Zhang MJ, Wu JB. Treatment of spontaneous perforation of the large intestine: a report of 9 cases. Zhongguo Putong Waike Zazhi. 2002;32:836-839. |
| 3. | Maurer CA, Renzulli P, Mazzucchelli L, Egger B, Seiler CA, Buchler MW. Use of accurate diagnostic criteria may increase incidence of stercoral perforation of the colon. Dis Colon Rectum. 2000;43:991-998. |
| 4. | Haddad R, Bursle G, Piper B. Stercoral perforation of the sigmoid colon. ANZ J Surg. 2005;75:244-246. |
| 5. | Tokunaga Y, Hata K, Nishitai R, Kaganoi J, Nanbu H, Ohsumi K. Spontaneous perforation of the rectum with possible stercoral etiology: report of a case and review of the literature. Surg Today. 1998;28:937-939. |
| 6. | Bin Xu, Shao WD, Shen HW, Wang QB. Emergence treatment of idiopathic rupture of sigmoid colon. Zhonghua Jizhen Yixue Zazhi. 2004;13:564-566. |
| 7. | Kasahara Y, Matsumoto H, Umemura H, Shirafa S, Kuyama T. Idiopathic perforation of the sigmoid colon in Japan. World J Surg. 1981;5:125-130. |
| 8. | Huang WS, Wang CS, Hsieh CC, Lin PY, Chin CC, Wang JY. Management of patients with stercoral perforation of the sigmoid colon: report of five cases. World J Gastroenterol. 2006;12:500-503. |
| 9. | Matsuo S, Eguchi S, Azuma T, Kanetaka K, Itoh S, Yamaguchi S, Obata S, Kanematsu T. An unusual perforation of the colon: report of two cases. Surg Today. 2002;32:836-839. |
| 10. | Hao WX. Analysis of the etiology and treatment for 18 cases with colonic perforation. Henan Waikexue Zazhi. 2004;10:46-47. |
| 11. | Wang ZQ. Analysis of diagnosis and treatment of spontaneous enterorrhexis. Xinjiang Yixue. 2006;4:58-59. |
| 12. | Zhang LX, Mao GJ, Shao AP. Diagnosis and treatment of spontaneous colonic perforation for 16 cases. Zhonghua Weichang Waike Zazhi. 2006;9:249. |
| 13. | Shao ZJ, Zhang CD, Su ZG. Analysis on spontaneous colonic perforation for 11 patients. Guangxi Yixue. 2006;28:512. |
| 14. | Xu G. Diagnosis and treatment for 7 old men with spontaneous colon rupture. Zhongguo Zhongxiyi Jiehe Waike Zazhi. 2005;11:528. |
| 15. | Li MJ, Xiang JB, Chen LL. Emergency treatment for colonic perforation(29 patients reported). Zhongguo Linchuang Yixue. 2001;11. |
| 16. | Li WZ, Xiao SX, Zeng D. Surgery for 22 old men with colonic perforation. Zhongguo Xiandai Shoushuxue Zazhi. 2004;8:46-47. |
| 17. | Zhe ZF, Sun SH. Analysis on 8 cases with spontaneous colon sigmoideum perforation. Zhongguo Wuzhenxue Zazhi. 2004;4:1124. |
| 18. | Jin MH, Pan F. Analysis on spontaneous colon rupture (3 cases reported). Zhongguo Yishi Jinxiu Zazhi. 2003;11:350. |
| 19. | Chen HK. Analysis on 9 patients with spontaneous colon rupture. Hebei Yixue. 2003;9:643. |
| 20. | Li XJ, Yang CY. Spontaneous intestinal perforation for 3 patients. Guangxi Yixue. 2002;4:212. |
| 21. | Guo ZS, Chen RZ. Treatment of 13 old men with Spontaneous colon sigmoideum. Linchuang Yiyaoxue. 2001;3:145. |
| 22. | Zheng XB, Sun SH. Analysis on 15 patients with spontaneous colon sigmoideum. Zunyi Yixueyuan Xuebao. 2001;3:243. |
| 23. | Xu M. Clinical manifestation and etiology analysis for 6 cases with spontaneous colon sigmoideum. Hebei Yixue. 2003;7:431. |
| 24. | Yi HY, Wang L, Lin Y, Che MZ, Zhang ZS. Aggregate analysis on 103 cases with spontaneous intestinal perforation. Zhongguo Zhongxiyi Jiehe Waike Zazhi. 2004;6:367. |
| 25. | Wang FL, Gao LF, Feng JX. Acute peritonitis induced by intestinal perforation for 30 cases. Heilongjiang Yixue. 2000;4:376. |