Published online Jul 21, 2008. doi: 10.3748/wjg.14.4359
Revised: June 23, 2008
Accepted: June 30, 2008
Published online: July 21, 2008
AIM: To determine the prevalence and risk factors of work-related musculoskeletal disorders in gastrointestinal endoscopists in Korea.
METHODS: A survey of musculoskeletal symptoms, using a self-administered questionnaire, was conducted on 55 endoscopists practicing in general hospitals or health promotion centers.
RESULTS: Forty-nine (89.1%) endoscopists reported musculoskeletal pain on at least one anatomic location and 37 (67.3%) endoscopists complained of pain at rest. Twenty-six (47.3%) endoscopists had severe musculoskeletal pain defined as a visual analogue score greater than 5.5. Factors related to the development of severe pain were (1) standing position during upper endoscopy, (2) specific posture/habit during endoscopic procedures, and (3) multiple symptomatic areas. Finger pain was more common in beginners, whereas shoulder pain was more common in experienced endoscopists. Sixteen percent of symptomatic endoscopists have modified their practice or reduced the number of endoscopic examinations. Only a few symptomatic endoscopists had sought professional consultation with related specialists.
CONCLUSION: The prevalence of musculoskeletal pain in endoscopists is very high. The location of pain was different between beginners and experienced endoscopists. Measures for the prevention and adequate management of endoscopy-related musculoskeletal symptoms are necessary.
- Citation: Byun YH, Lee JH, Park MK, Song JH, Min BH, Chang DK, Kim YH, Son HJ, Rhee PL, Kim JJ, Rhee JC, Hwang JH, Park DI, Shim SG, Sung IK. Procedure-related musculoskeletal symptoms in gastrointestinal endoscopists in Korea. World J Gastroenterol 2008; 14(27): 4359-4364
- URL: https://www.wjgnet.com/1007-9327/full/v14/i27/4359.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.4359
Muscle and joint pains are common complaints in individuals whose job requires repetitive isometric maneuvers or awkward body positions[1]. Musculoskeletal pains have been reported in individuals with different occupations such as bus drivers, unskilled laborers, musicians, physical therapists, and computer keyboard operators[1–7]. Recently, ergonomic mechanisms related to the development of work-related musculoskeletal disorders (MSD) have drawn substantial interest[8–10].
Work-related musculoskeletal symptoms are common in certain medical specialists such as laparoscopic surgeons and dentists[1112]. However, there are very few studies on MSD in gastrointestinal endoscopists. The incidence of musculoskeletal injuries has been variously reported from as low as 13% for neck pain[13] to as high as 57% for back pain[14]. To the best of our knowledge, a detailed study in endoscopists’ on the severity of musculoskeletal symptoms, symptom-related risk factors, and doctor’s response to their own symptoms has not been performed in eastern countries. The purpose of the present study was to assess the prevalence, severity, risk factors, and clinical impact of work-related MSD in gastrointestinal endoscopists in Korea.
From June 2006 to September 2006, 55 endoscopists practicing in 4 general hospitals and 2 health promotion centers were included in the present study. Endoscopists expressed their willingness to participate and completed a self-reported questionnaire. The questionnaire was largely structured; although some questions were kept open. Data were collected on the age, gender, duration of endoscopy practice, underlying musculoskeletal disease, and postures and habits during endoscopy. Workload parameters included total duration of endoscopy practice, weekly working hours and monthly number of endoscopic procedures. The areas of musculoskeletal pain were marked on a figure of the human body, and the severity of pain at each site was expressed using a 100 mm visual analogue scale (VAS), a standard measurement tool in pain research. The presence of severe pain was defined as a VAS value greater than 55 mm[1516]. The participants were also asked as to whether their symptoms affected their ability to perform endoscopic procedures, how they managed their symptoms, and whether they had endoscopy-related symptoms other than MSD.
Continuous data were expressed as mean ± standard deviation (SD) or median with range. Categorical data analysis was conducted using the chi-square test. Continuous data were analyzed using the independent t test. All P values were 2-tailed and P values less than 0.05 were considered statistically significant.
Fifty-five endoscopists (male 37, female 18) participated in the study. The median age was 39 years (range, 28-47 years), and the median duration of practicing endoscopy was 39 mo (range, 1-228 mo). The average procedure time per week was 19.5 ± 7.7 h. The average number of endoscopies performed per month was 270.2 ± 153.2.
Eighty-three percent of the endoscopists reported possible endoscopy-related non-musculoskeletal symptoms, such as decreased visual acuity (63.6%), chronic fatigue (60%), depressive mood (18.2%), dizziness (14.5%), headache (12.7%), and skin allergy (1.8%).
Forty-nine (89.1%) endoscopists reported muscu-loskeletal pain on at least one anatomic location. The average number of symptomatic areas was 3.9 ± 2.8. Forty endoscopists (72.7%) had pain at more than one anatomic location. Thirty-seven endoscopists (67.3%) had pain at rest. The VAS value of the most painful area was 5.4 ± 2.2. The musculoskeletal pain developed at 27.5 ± 37.9 mo (range, 1-156 mo) after starting endoscopy.
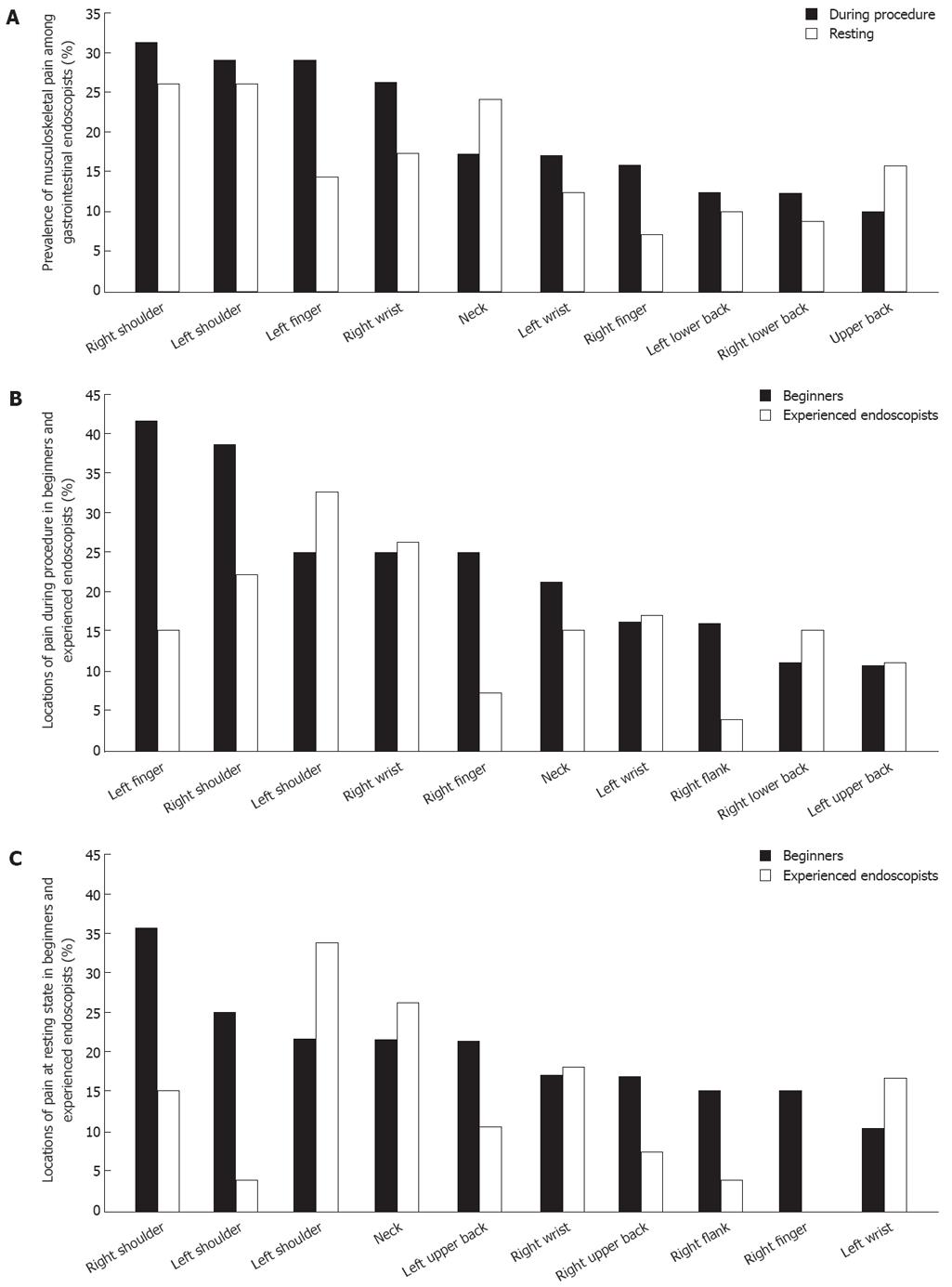
The location and incidence of musculoskeletal pain during endoscopic procedures or at rest are shown in Figure 1A. The most commonly reported painful area during endoscopic procedures was right shoulder, followed by left shoulder and left finger. There was little difference in the overall distribution of the painful areas at rest. However, neck pain and upper back pain were relatively frequent.
The most painful site during endoscopic procedures was the left finger (16.4%), followed by left shoulder and right wrist (14.5%), left wrist (9.1%) and right shoulder (7.3%). The left and right shoulder (12.7%) were the most painful areas at rest, followed by neck (9.1%), right upper back and lower back (5.5%).
Twenty-six endoscopists (47.3%) had severe muscu-loskeletal pain with a VAS value greater than 55 mm[1516]. Three factors were statistically related to the development of severe musculoskeletal pain: (1) standing position during upper endoscopic procedures, (2) specific posture or habit during endoscopic procedures, and (3) multiple symptomatic areas (Table 1). The proportion of endoscopists with severe musculoskeletal pain was slightly higher in female than in male endoscopists (61.1% and 40.5%, respectively; P = 0.152).
| With severe musculoskeletal pain (n = 26) | Without severe musculoskeletal pain (n = 29) | P | |
| Age (median, range, yr) | 34 (29-47) | 36 (28-45) | |
| Sex | |||
| Male | 15 | 22 | |
| Female | 11 | 7 | |
| Career | |||
| Full time faculty | 16 | 15 | |
| Trainee | 10 | 14 | |
| Duration of practicing endoscopy (mean, range, mo) | 40.5 (1-204) | 39 (1-228) | |
| Posture in upper endoscopy | 0.027 | ||
| Mainly standing | 25 | 21 | |
| Mainly sitting | 1 | 8 | |
| Posture in colonoscopy | |||
| Mainly standing | 11 | 12 | |
| Mainly sitting | 15 | 17 | |
| Specific posture or habit during endoscopy (%) | 11 (68.8) | 5 (31.3) | 0.041 |
| Number of endoscopies per month (mean ± SD) | 280.5 ± 159.3 | 260.1 ± 149.7 | |
| Time of endoscopic procedure per week (mean ± SD, h) | 20.5 ± 8.1 | 17.9 ± 7.2 | |
| Number of painful areas (mean ± SD) | 4.8 ± 3.2 | 2.3 ± 2.1 | 0.002 |
Endoscopists were divided into two groups (beginner versus experienced) by the total duration of practicing endoscopy (39 mo, Table 2). In the beginner group, the weekly procedure time was longer and the number of endoscopic examinations was greater. However, there was no significant difference in the prevalence of musculoskeletal pain, number of symptomatic areas, and VAS value of the most painful area between the two groups.
| Beginners (n = 28) | Experienced endoscopists (n = 27) | P | |
| Pain over at least one anatomic location (%) | 26 (92.8) | 23 (85.2) | |
| Severe pain with VAS value > 5.5 (%) | 15 (53.6) | 13 (48.1) | |
| Multiple painful areas (%) | 22 (78.6) | 18 (66.7) | |
| Number of painful areas (mean ± SD) | 3.9 ± 3.0 | 3.1 ± 2.9 | |
| VAS value of the most painful area (mean ± SD) | 4.9 ± 2.3 | 4.7 ± 3.1 | |
| Duration of endoscopic procedure per week (mean ± SD, h) | 23.7 ± 7.6 | 14.9 ± 5.2 | 0.001 |
| Number of endoscopies per month (mean ± SD) | 322.4 ± 159.9 | 216.1 ± 127.4 | 0.009 |
By contrast, the location of pain was different between the two groups (Figure 1B and C). During a procedure, the left finger was the most commonly reported painful area in beginners (42.9%, 12/28), whereas the left shoulder was the most commonly reported painful area by experienced endoscopists (33.3%, 9/27) (Figure 1B). The distribution of the most painful area during endoscopic procedures was also different in the two groups. The most painful area was the left finger (21.4%, 6/28) in beginners, followed by right wrist (10.7%, 3/28), left shoulder (7.1%, 2/28) and left wrist (7.1%, 2/28). However, the most painful locations in experienced endoscopists were the left shoulder (22.2%, 6/27), followed by right wrist (18.5%, 5/27), left finger (11.1%, 3/27) and left wrist (11.1%, 3/27). The distribution of pain and the most painful areas at rest were very similar in the two groups (data not shown).
Among endoscopists with musculoskeletal pain, 16.3% (8/49) reported that they had modified their practice or reduced the number of the endoscopic procedures. A majority (81.6%) of endoscopists with musculoskeletal pain managed their symptoms by themselves using stretching (67.3%), exercising (8.2%) and rest (6.1%). Fourteen endoscopists (28.6%) reported the use of medications such as nonsteroidal anti-inflammatory drugs or topical analgesic patches.
Only 14.3% (7/49) of symptomatic endoscopists had sought advice from specialists on musculoskeletal disorders or had undergone a specific diagnostic work-up. Three endoscopists were diagnosed to have a sprain (n = 1) or a cervical intervertebral disk herniation (n = 2). In the two endoscopists with herniated disc, one required a 4-wk sick leave until the symptoms improved and the other had modified the practice and reduced the number of endoscopic procedures.
Work-related MSDs or overuse syndrome are a group of diseases resulting from repetitive action at the work place[17]. Collagen failure and connective tissue damage results in inflammation, pain, and further weakening of the tissues. Such a vicious cycle can lead to permanent injury and disability if the tissues are not allowed to heal properly[13]. Work-related injury is an important cause of missed workdays and impaired performance at work.
We observed that MSD is very prevalent in gastrointestinal endoscopists in Korea. A majority of endoscopists experienced pain at multiple anatomic areas (72.7%) and two-third (67.3%) complained of the pain at rest. The prevalence of MSD observed in the present study is higher than that noted in previous reports by other groups[1314]. One possible explanation is that the endoscopic workload of the doctors in the present study was very high. In this regard, a previous study reported that the endoscopic volume measured in terms of hours per week, number per week, or percentage of working time was strongly associated with the development of musculoskeletal injuries among endoscopists[13]. Workload-associated factors such as the number or duration of work were also related to the prevalence of MSD in other occupations[1318].
In the present study, 26 (47.3%) endoscopists complained of severe musculoskeletal pain, defined as a VAS value greater than 5.5 (Table 1). Endoscopists with severe pain were more likely to have multiple painful areas than those without severe pain. Contrary to our expectations, there was no significant difference in the endoscopic workload between them. This may be due to the small number of participants of the present study. However, ergonomic factors like bad posture during the procedure may be important in the development of endoscopy-related musculoskeletal symptoms. With respect to this hypothesis, we observed that ergonomic factors, such as specific posture/habit during the procedure and standing position in upper gastrointestinal endoscopy, correlated significantly with the development of severe musculoskeletal pain.
In the present study, the experience level of endoscopists was not related to the prevalence of musculoskeletal pain, the number of symptomatic areas, and the severity of the most painful regions. However, there were differences in the distribution of the symptomatic areas (Figure 1B and C). For example, finger pain was more common in beginners, whereas shoulder pain was more common in experienced endoscopists. This was especially true when the endoscopist was performing a procedure. The exact reason of this difference is unclear, but muscles and/or joints frequently used during an endoscopic procedure may differ with the experience of the endoscopist. In this respect, it should be noted that beginners tend to depend more on the movement of the knob during endoscopy.
The best approach to MSD must be preventive. As noted in a previous report[13], endoscopists in the present study tended to neglect or tried to alleviate their symptoms by themselves without resorting to professional help. However, we found that a small proportion (16.3%) of symptomatic endoscopists modified the procedure patterns or reduced the number of endoscopic procedures. The overall efficacy of an endoscopy unit may be negatively influenced by these factors. Measures for the prevention of work-related MSD may improve the productivity of healthcare institutions. The importance of ergonomics in work-related MSDs has been studied in a certain fields[1920]. Endoscopists should also take advantage of such studies.
A major limitation of our study was that it was difficult to determine whether a particular symptom was related to endoscopy or not. This was related to our study design using a self-administered questionnaire without an objective assessment of the symptoms. However, we presumed that a great proportion of the symptoms in the present study were endoscopy-related. Another limitation was that the participants were working in either general hospitals or health promotion centers, where the volume of endoscopic procedures exceeds the average endoscopic workload. About one-half of endoscopies, in general, were performed under sedation, the proportion of upper to lower endoscopy was approximately three to two, and that of therapeutic endoscopies was almost twenty percent, although this aspect was not investigated in the present survey. Finally, there was no follow-up data in the present study. Large-scaled follow-up studies in various clinical settings are needed.
In conclusion, the prevalence of musculoskeletal symptoms in endoscopists is very high, and the majority of symptomatic endoscopists do not seek professional consultation. The pattern of musculoskeletal pain among beginners and experienced endoscopists was different, suggesting multiple ergonomic mechanisms for symptom development. Measures for the prevention and adequate management of endoscopy-related musculoskeletal symptoms are necessary.
Work related musculoskeletal disorder (MSD) is a common problem in individuals whose job requires repetitive isometric maneuvers or awkward body positions. However, the prevalence of MSD among endoscopists is not well known. The present study was designed to investigate the prevalence and risk factors of work-related MSD in gastrointestinal endoscopist in Korea.
We investigated the incidence, severity, location and clinical impact of work-related MSD during endoscopic procedures and at rest in gastrointestinal endoscopists. The present study is the first detailed study designed to investigate MSD in gastrointestinal endoscopists in eastern countries.
We used a self reported questionnaire in 55 endoscopists practicing in 4 general hospitals and 2 health promotion centers. The severity of MSD was assessed by the visual analogue scale, a standard measurement tool in pain research.
In the present study, the prevalence of musculoskeletal symptoms among endoscopists was very high, and the majority of symptomatic endoscopists did not seek professional consultation. The pattern of musculoskeletal pain in beginners and in experienced endoscopists was different, suggesting multiple ergonomic mechanisms for symptom development. We hope the present study would lead to interest in work-related MSD and ergonomics in gastrointestinal endoscopists.
The present study has shown that the development of severe pain in gastrointestinal endoscopists is related to ergonomic factors, such as specific posture/habit and the standing position during endoscopic procedures. The study suggests that endoscopists need to focus on teaching a beginner about proper posture and manipulation techniques in order to prevent musculoskeletal symptoms.
| 1. | Smith AC, Wolf JG, Xie GY, Smith MD. Musculoskeletal pain in cardiac ultrasonographers: results of a random survey. J Am Soc Echocardiogr. 1997;10:357-362. |
| 2. | Anderson R. The back pain of bus drivers. Prevalence in an urban area of California. Spine. 1992;17:1481-1488. |
| 3. | Mahbub MH, Laskar MS, Seikh FA, Altaf MH, Inoue M, Yokoyama K, Wakui T, Harada N. Prevalence of cervical spondylosis and musculoskeletal symptoms among coolies in a city of Bangladesh. J Occup Health. 2006;48:69-73. |
| 4. | Sakai N, Liu MC, Su FC, Bishop AT, An KN. Hand span and digital motion on the keyboard: concerns of overuse syndrome in musicians. J Hand Surg Am. 2006;31:830-835. |
| 5. | Salik Y, Ozcan A. Work-related musculoskeletal disorders: a survey of physical therapists in Izmir-Turkey. BMC Musculoskelet Disord. 2004;5:27. |
| 6. | Arvidsson I, Arvidsson M, Axmon A, Hansson GA, Johansson CR, Skerfving S. Musculoskeletal disorders among female and male air traffic controllers performing identical and demanding computer work. Ergonomics. 2006;49:1052-1067. |
| 7. | Bragge P, Bialocerkowski A, McMeeken J. A systematic review of prevalence and risk factors associated with playing-related musculoskeletal disorders in pianists. Occup Med (Lond). 2006;56:28-38. |
| 8. | Dennerlein JT, Johnson PW. Changes in upper extremity biomechanics across different mouse positions in a computer workstation. Ergonomics. 2006;49:1456-1469. |
| 9. | Koppejan S, Snijders CJ, Kooiman T, Van Bemmel B. Hand and arm problems in flautists and a design for prevention. Ergonomics. 2006;49:316-322. |
| 10. | Woods M, Babski-Reeves K. Effects of negatively sloped keyboard wedges on risk factors for upper extremity work-related musculoskeletal disorders and user performance. Ergonomics. 2005;48:1793-1808. |
| 11. | Fish DR, Morris-Allen DM. Musculoskeletal disorders in dentists. N Y State Dent J. 1998;64:44-48. |
| 12. | Reyes DA, Tang B, Cuschieri A. Minimal access surgery (MAS)-related surgeon morbidity syndromes. Surg Endosc. 2006;20:1-13. |
| 14. | O'Sullivan S, Bridge G, Ponich T. Musculoskeletal injuries among ERCP endoscopists in Canada. Can J Gastroenterol. 2002;16:369-374. |
| 15. | Collins SL, Moore RA, McQuay HJ. The visual analogue pain intensity scale: what is moderate pain in millimetres? Pain. 1997;72:95-97. |
| 16. | Myles PS, Urquhart N. The linearity of the visual analogue scale in patients with severe acute pain. Anaesth Intensive Care. 2005;33:54-58. |
| 17. | Liberman AS, Shrier I, Gordon PH. Injuries sustained by colorectal surgeons performing colonoscopy. Surg Endosc. 2005;19:1606-1609. |
| 18. | Cromie JE, Robertson VJ, Best MO. Work-related musculoskeletal disorders in physical therapists: prevalence, severity, risks, and responses. Phys Ther. 2000;80:336-351. |
| 19. | Pearce B. Ergonomic considerations in work-related upper extremity disorders. Clin Occup Environ Med. 2006;5:249-266, vi. |
| 20. | Lee EC, Rafiq A, Merrell R, Ackerman R, Dennerlein JT. Ergonomics and human factors in endoscopic surgery: a comparison of manual vs telerobotic simulation systems. Surg Endosc. 2005;19:1064-1070. |