Published online Jul 7, 2008. doi: 10.3748/wjg.14.4091
Revised: June 8, 2008
Accepted: June 15, 2008
Published online: July 7, 2008
In this case report, we present a patient who suffered from gastrointestinal bleeding. The bleeding source was a gastric arterio-venous malformation emerging from the splenic artery. Attempts to stop the bleeding failed and therapeutic angiography succeeded in occluding the vessel. A search at the literature has not yielded any other case report describing this anatomical anomaly.
- Citation: Elazary R, Verstandig A, Rivkind AI, Almogy G. Gastric arterio-venous malformation emerging from splenic artery. World J Gastroenterol 2008; 14(25): 4091-4092
- URL: https://www.wjgnet.com/1007-9327/full/v14/i25/4091.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.4091
Upper gastrointestinal bleeding is a common cause for patient admission to the general surgery departments. There are various pathologies which lead to bleeding; however, bleeding due to gastric arterio-venous malformation is not commonly seen. In this article we present a patient with sustained hematemesis, whose medical workup revealed the bleeding source to be the stomach. The bleeding could not be stopped by upper endoscopy. Celiac trunk angiography demonstrated arterio-venous malformation emerging from the splenic artery and embolization of the vessel was performed. A search of the English medical literature for congenital anomalies such as aretrio-venous malformations supplied by the splenic artery did not yield any similar descriptions.
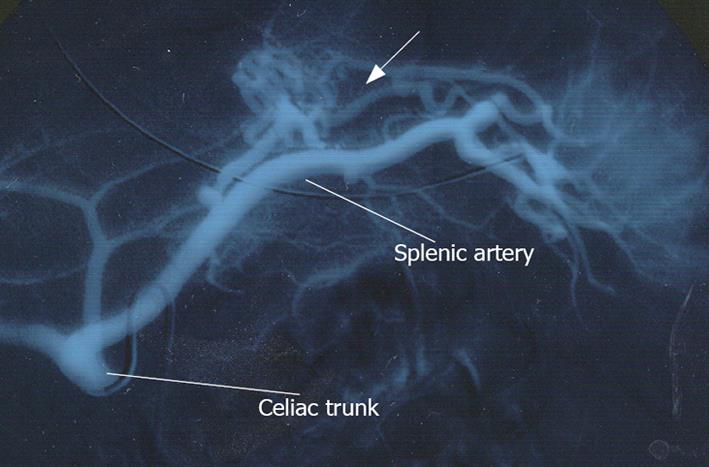
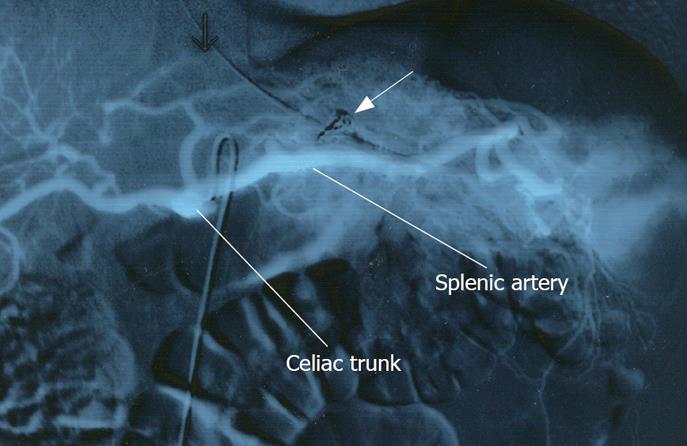
A 24-year-old previously healthy male was transferred to our general surgery department due to unsuccessful treatment of acute upper gastrointestinal bleeding. Ten days ago, he had been admitted to hospital due to hematemesis and melena. He underwent an upper endoscopy, which demonstrated a small gastric ulcer covered by a blood clot, without a visible vessel. The ulcer was endoscopically coagulated using Argon beam. Four days later the patient had sustained hematemesis again. He underwent a second endoscopy, which showed a large clot covering a gastric ulcer. During hospitalization he was treated with ten units of packed red blood cells. Due to the relapse of symptoms and massive transfusion of blood products an angiography was performed. An aberrant gastric arterio-venous malformation supplied by the splenic artery was demonstrated. Attempts to embolize the vessel failed and the patient was referred to our institute. Upon arrival, his pulse was 102 bpm, and blood pressure 140/80 mmHg. Blood tests showed hemoglobin level of 10.2 mg/dL. Naso-gastric tube was inserted and drained fresh blood. Celiac trunk angiography was performed and revealed an arterio-venous malformation emerging from the splenic artery (Figure 1). Arterial embolization was achieved by selective injection of embospheres (diameter of 0.5-0.7mm) and placement of several detachable coils until flow arrest was obtained (Figure 2). The procedure was performed without any immediate complications. Two days following the procedure the patient developed a fever of 38°C, and suffered from left upper quadrant abdominal pain, both were attributed to segmental infarction of the spleen. Blood tests showed a constant level of hemoglobin. Eight days after the procedure he underwent elective upper endoscopy which showed mild fundal gastritis without an ulcer. On a six-month follow up, the patient presented no symptoms.
Upper gastrointestinal bleeding is a common cause for admission of patients to emergency departments[1]. The most common etiologies are esophageal or gastric varices due to portal hypertension, erosive gastritis, peptic ulcers and gastric benign or malignant tumors. Other rare pathologies are aorto-enteric fistula which can cause massive upper gastrointestinal bleeding, gastric arterio-venous malformation[2] which is very common in patients who suffer from end stage renal failure, or Dieulafoy’s syndrome[3] which is a congential dysplastic large caliber artery often lying at the submucosa of the gastric fundus, where erosion of the overlying mucosa is believed to cause significant bleeding. The pathogenesis of arterio-venous malformations of the splenic artery[4] is described in the medical literature as a cause of left sided portal hypertension (arterio-venous malformation is caused by blunt or penetrating trauma to the splenic artery which produces a fistula between the artery and the vein). A high flow of blood directly from the artery through the portal venous system elevates the portal blood pressure. Other pathology of the splenic artery which can cause massive upper gastrointestinal or intra-abdominal bleeding, is aneurysm of the artery. Aneurysms are the third most common intra-abdominal aneurysms, they are more common in multi-gravid women or patients with pancreatitis or abdominal trauma, and rarely cause any symptoms. Erosion into the gastric wall initiates gastric bleeding which may be massive.
The arterial supply of the vascular malformation described in this case emerged from the splenic artery, the patient did not sustain any abdominal trauma. It seems that an embryological developmental defect caused this congenital anomaly. Searching the English medical literature for articles describing this rare pathology has not found any similar descriptions. We assume that growing use of angiographic modalities for diagnosis and treatment of pathologies will show in the future more congenital anomalies which have not been characterized yet. The arterio-venous malformation has also supplied part of the spleen. According to this, we recommend not to discharge the patients too early after the procedure because of possible occurrence of complications related to partial infraction of the spleen. Usually such an infraction necessitates only observation and analgesia.
| 1. | Kramer SC, Gorich J, Rilinger N, Siech M, Aschoff AJ, Vogel J, Brambs HJ. Embolization for gastrointestinal hemorrhages. Eur Radiol. 2000;10:802-805. |
| 2. | Sherman L, Shenoy SS, Satchidanand SK, Neumann PR, Barrios GG, Peer RM. Arteriovenous malformation of the stomach. Am J Gastroenterol. 1979;72:160-164. |
| 3. | Juler GL, Labitzke HG, Lamb R, Allen R. The pathogenesis of Dieulafoy's gastric erosion. Am J Gastroenterol. 1984;79:195-200. |
| 4. | Baron PW, Sindram D, Suhocki P, Webb DD, Clavien PA. Upper gastrointestinal bleeding from gastric submucosal arterial collaterals secondary to splenic artery occlusion: treatment by splenectomy and partial gastric devascularization. Am J Gastroenterol. 2000;95:3003-3004. |