Published online Jun 14, 2008. doi: 10.3748/wjg.14.3598
Revised: May 8, 2008
Accepted: May 15, 2008
Published online: June 14, 2008
Two patients with liver cirrhosis and portal hypertension related to hepatitis infection were admitted to Shanghai Ruijin Hospital due to recurrent melena and hematemesis. Isolated gastric varices were observed in the gastric fundus during the retroflexion of gastroscope. We carried out endoscopic sclerotherapy successfully for bleeding gastric varices with combined cyanoacrylate and aethoxysklerol, which disappeared dramatically several months after two courses of sclerotherapy for each patient. No complication and clinical signs of gastrointestinal re-bleeding were observed during the 6-mo endoscopic follow-up. CT portal angiography (CTPA) has been widely used in the assessment of variceal treatment and improves the results of endoscopic injection therapy.
- Citation: Shi B, Wu W, Zhu H, Wu YL. Successful endoscopic sclerotherapy for bleeding gastric varices with combined cyanoacrylate and aethoxysklerol. World J Gastroenterol 2008; 14(22): 3598-3601
- URL: https://www.wjgnet.com/1007-9327/full/v14/i22/3598.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.3598
Gastric varices have been increasingly recognized as a major cause of gastrointestinal bleeding in patients with portal hypertension. Compared with esophageal variceal bleeding, hemorrhage caused by gastric varices is usually more severe and hemostatic control is reported to be more difficult[1].
Management for gastric varices usually include vasoactive agents, endoscopic therapy and surgery[2]. Rupture of gastric fundal varices is often lethal because of massive bleeding[34]. Three-channel double-balloon catheter might be ineffective for gastric fundal varices when acute bleeding occurs. Endoscopic injection with tissue adhesives such as histoacryl can effectively control active bleeding[56]. However, gastric varices cannot disappear due to the unsatisfactory control of inflammation and fibrous organization caused by adhesives. Although endoscopic variceal ligation therapy (EVL) has shown its benefit for esophageal varices, it cannot achieve a similar success in the management of gastric varices[6]. It was reported that balloon retrograde transvenous obliteration (B-RTO) is a useful treatment for gastric fundal varices, but it requires a gastrorenal shunt as the draining vein[7]. We report two cases of marked gastric varices with no gastrorenal shunt, who were successfully treated with endoscopic therapy with combined adhesives and sclerosants.
Patient one was a 69-year-old male suffering from recurrent melena for 3 mo. He had a 20-year history of hepatitis B virus (HBV) infection and a 8-year history of hepatitis C virus (HCV) infection and was diagnosed having viral liver cirrhosis and portal hypertension two years ago. His Child-Pugh was class B. Patient two was a 61-year-old female with liver cirrhosis and portal hypertension. She was admitted to the gastroenterology ward due to the onset of hematemesis. Her Child-Pugh was class A. Upper gastrointestinal (GI) endoscopy showed massive isolated gastric varices of the gastric fundus with red flat spots on their surface in both patients. No esophageal varices were observed. CTPA revealed dilated portal vein and tortuous splenic vein in both patients while gastric fundal varices were noticed to communicate with the confluence through the left gastric vein. No evidence of gastrorenal shunt was shown. Written informed consent was obtained from the two patients before endoscopic sclerotherapy.
Both patients received endoscopic injection sclero-therapy with combined cyanoacrylate and aethoxysklerol. Routine preparation was carried out and anti-foam agent, simethicone, was administered 20 min before endoscopy. An intravenous infusion of somatostatin at 250 &mgr;g/h was performed 2 h before and 72 h after the therapy. The endoscopic therapy procedure required a retroflex view for variceal visualization. During the treatment, 10 mL of 1% aethoxysklerol (Polidocanol, Germany) was injected into the varix followed by conventional endoscopic injection sclerotherapy with a mixture of 1.5 mL α-cyanoacrylate alkyl (Compont, China) and 1.5 mL iodinated oil (Lipiodol, French). When no active bleeding or oozing of the varix occurred, the procedure was terminated.
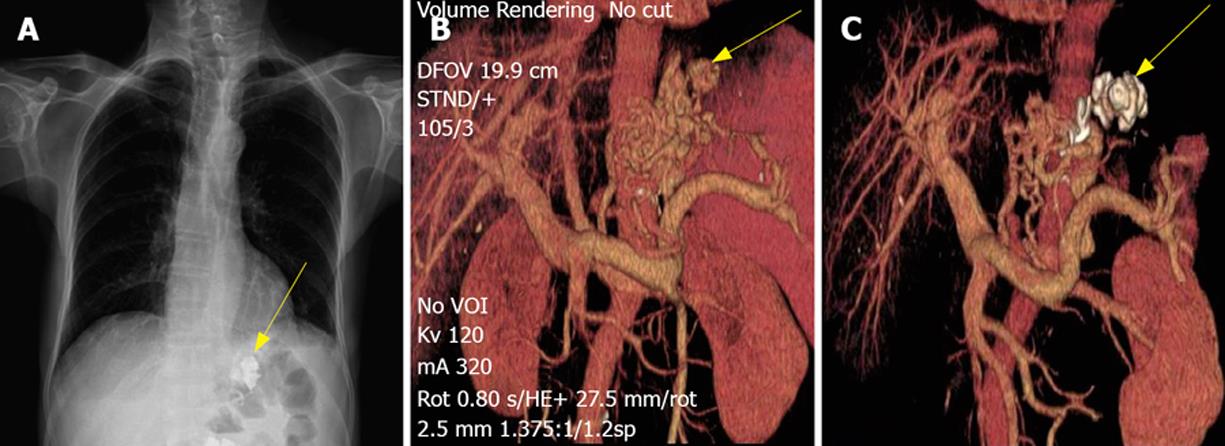
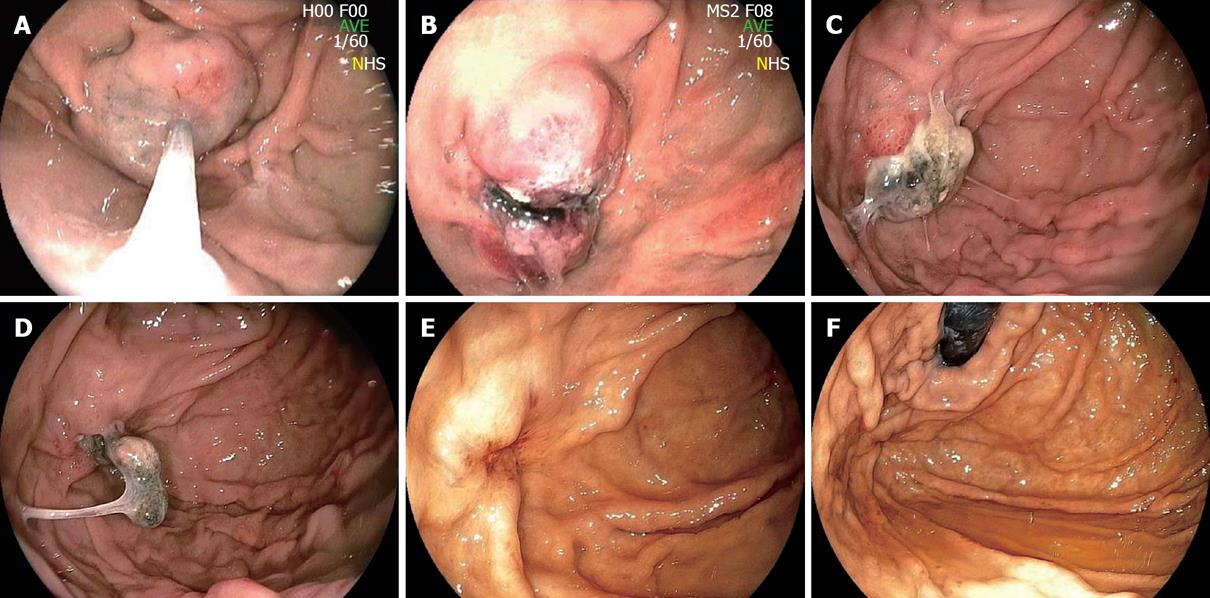
Both patients tolerated the procedure well with no immediate complication. Subsequent chest X-ray one day after sclerotherapy demonstrated a marked collection of cyanoacrylate/lipiodol mixture within the variceal bed in the gastric fundus, but no sign of ectopic infarction. CTPA 3 wk after sclerotherapy showed shrinkage of gastric fundal varices and deposition of cyanoacrylate/lipiodol mixture blocking the draining veins (Figure 1). A repeated sclerotherapy was performed 3 wk later. A 6-mo endoscopic follow-up after the second treatment revealed dramatic disappearance of gastric varices in both patients (Figure 2). The two patients were free from re-bleeding after the last endoscopic treatment.
The incidence of gastric variceal bleeding is lower than that of esophageal varices. However, rupture of gastric varices usually results in more severe hemorrhage and a higher mortality[1].
Since the description of experience with the use of cyanoacrylate compounds in endoscopic treatment of gastric varices in an experimental dog model in 1975[8], adhesives such as N-butyl-2-cyanoacrylate (histoacryl) have been proved safe and efficient in the treatment of active bleeding of gastric varices. N-butyl-2-cyanoacrylate has not been approved for its use in treatment of variceal bleeding by China State Food and Drug Administration (SFDA). In our cases, α-cyanoacrylate alkyl, an analogue of N-butyl-2-cyanoacrylate approved by SFDA, showed a similar pharmaceutical effect to N-butyl-2-cyanoacrylate. The adhesive polymer, an unabsorbable foreign body in the bed of varices after injection, could block the ruptured vein yet had a weak effect on promoting organization of the veins. Ulceration may occur and the polymer extrudes from the vessel bed several weeks after injection, during which fatal re-bleeding may occur[9]. The similar extrusion process was performed for the 69-year-old male patient during the endoscopic follow-up period (Figure 3).
Polidocanol is a well-accepted sclerosant for obliteration of gastric varices. It can produce significant thrombosis, inflammatory reaction and fibrous degene-ration, thus finally eliminating the varices. Though sclerosing agents are widely used in the treatment of esophageal varices, they are far less promising for the treatment of gastric varices[1011]. In Japan, ethanolamine oleate (EO) remains the first choice of sclerotherapeutic agents for eradicating esophageal varices, yet it has not been greatly used in the management of gastric varices. Oho and colleagues[12] reported that the rate of initial hemostasis is significantly lower in patients with bleeding gastric varices treated with EO than in those treated with butyl cyanoacrylate.
In our cases, the effect of α-cyanoacrylate alkyl and aethoxysklerol on gastric varices was satisfactory and their gastric varices disappeared six months after treatment.
Rare but serious complications of endoscopic sclerotherapy may include cerebral stroke, pulmonary embolism, portal vein embolism and splenic infarction[1314]. Gastric varices are characterized by an enlarged caliber of the vessel bed, large draining veins and rapid blood flow, which may exacerbate the situation. Fortunately, no complication was found in these two patients.
After sclerotherapy, both patients were given antacids to suppress the secretion of gastric acid, thus protecting the gastric mucosa and promoting the healing of ulcer. The dosage of rabeprazole, a proton-pump inhibitor, may be increased to 20 mg once a day per oral depending on the severity of ulcer on the surface of varices. Meanwhile, the patients were given propranolol and isosorbide mononitrate to reduce their portal pressure. After sclerotherapy, re-bleeding, especially during the process of adhesive extrusion, should be prevented.
CTPA can serve as an important supplement and an alternative technique for gastric varices. It can be applied in choosing appropriate candidates, evaluating and following up patients with gastric varices[15]. We detected the varices and made assessments of portosystemic collaterals through CTPA before sclerotherapy, which demonstrated the afferent and efferent vessels of gastric varices. Willmann and colleagues[16] demonstrated that CTPA is able to differentiate between submucosal and perigastric fundal varices, which is of paramount interest since only the former may cause gastrointestinal hemorrhage. CTPA revealed the vessels blocked by adhesive polymer, obliteration and elimination of gastric varices, suggesting that injection of adhesives in combination with sclerosants is an effective treatment modality for gastric varices.
In conclusion, although the optimal treatment for gastric fundal variceal bleeding remains controversial, sclerotherapy with combined α-cyanoacrylate alkyl and aethoxysklerol is an alternative and feasible treatment modality for gastric fundal varices.
| 1. | Sarin SK, Lahoti D, Saxena SP, Murthy NS, Makwana UK. Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology. 1992;16:1343-1349. |
| 2. | Garcia-Tsao G, Sanyal AJ, Grace ND, Carey WD. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Am J Gastroenterol. 2007;102:2086-2102. |
| 3. | Watanabe K, Kimura K, Matsutani S, Ohto M, Okuda K. Portal hemodynamics in patients with gastric varices. A study in 230 patients with esophageal and/or gastric varices using portal vein catheterization. Gastroenterology. 1988;95:434-440. |
| 4. | Akahoshi T, Hashizume M, Shimabukuro R, Tanoue K, Tomikawa M, Okita K, Gotoh N, Konishi K, Tsutsumi N, Sugimachi K. Long-term results of endoscopic Histoacryl injection sclerotherapy for gastric variceal bleeding: a 10-year experience. Surgery. 2002;131:S176-S181. |
| 5. | Sarin SK, Jain AK, Jain M, Gupta R. A randomized controlled trial of cyanoacrylate versus alcohol injection in patients with isolated fundic varices. Am J Gastroenterol. 2002;97:1010-1015. |
| 6. | Lo GH, Lai KH, Cheng JS, Chen MH, Chiang HT. A prospective, randomized trial of butyl cyanoacrylate injection versus band ligation in the management of bleeding gastric varices. Hepatology. 2001;33:1060-1064. |
| 7. | Ninoi T, Nishida N, Kaminou T, Sakai Y, Kitayama T, Hamuro M, Yamada R, Nakamura K, Arakawa T, Inoue Y. Balloon-occluded retrograde transvenous obliteration of gastric varices with gastrorenal shunt: long-term follow-up in 78 patients. AJR Am J Roentgenol. 2005;184:1340-1346. |
| 8. | Rosch J, Goldman ML, Dotter CT. Experimental catheter obstruction of the gastric coronary vein. Possible technique for percutaneous intravascular tamponade of the gastroesophageal varices. Invest Radiol. 1975;10:206-211. |
| 9. | Soehendra N, Grimm H, Nam VC, Berger B. N-butyl-2-cyanoacrylate: a supplement to endoscopic sclerotherapy. Endoscopy. 1987;19:221-224. |
| 10. | Trudeau W, Prindiville T. Endoscopic injection sclerosis in bleeding gastric varices. Gastrointest Endosc. 1986;32:264-268. |
| 11. | Sarin SK. Long-term follow-up of gastric variceal sclerotherapy: an eleven-year experience. Gastrointest Endosc. 1997;46:8-14. |
| 12. | Oho K, Iwao T, Sumino M, Toyonaga A, Tanikawa K. Ethanolamine oleate versus butyl cyanoacrylate for bleeding gastric varices: a nonrandomized study. Endoscopy. 1995;27:349-354. |
| 13. | Binmoeller KF. Glue for gastric varices: some sticky issues. Gastrointest Endosc. 2000;52:298-301. |
| 14. | Feretis C, Dimopoulos C, Benakis P, Kalliakmanis B, Apostolidis N. N-butyl-2-cyanoacrylate (Histoacryl) plus sclerotherapy versus sclerotherapy alone in the treatment of bleeding esophageal varices: a randomized prospective study. Endoscopy. 1995;27:355-357. |
| 15. | Matsumoto A, Kitamoto M, Imamura M, Nakanishi T, Ono C, Ito K, Kajiyama G. Three-dimensional portography using multislice helical CT is clinically useful for management of gastric fundic varices. AJR Am J Roentgenol. 2001;176:899-905. |