Published online Jun 14, 2008. doi: 10.3748/wjg.14.3587
Revised: May 12, 2008
Accepted: May 19, 2008
Published online: June 14, 2008
We herein report a case of a hilar tumor with extensive invasion to the proper hepatic artery, which was successfully treated with a radical resection in a 57-year-old female patient after a stepwise hepatic arterial embolization. She underwent right colectomy and partial hepatectomy for advanced colon cancer two years ago and radiofrequency ablation therapy for a liver metastasis one year ago, respectively. A recurrent tumor was noted around the proper hepatic artery with invasion to the left hepatic duct and right hepatic artery 7 mo previously. We planned a radical resection for the patient 5 mo after the absence of tumor progression was confirmed while he was undergoing chemotherapy. To avoid surgery-related liver failure, we tried to promote the formation of collateral hepatic arteries after stepwise arterial embolization of the posterior and anterior hepatic arteries two weeks apart. Finally, the proper hepatic artery was occluded after formation of collateral flow from the inferior phrenic and superior mesenteric arteries was confirmed. One month later, a left hepatectomy with hepatic arterial resection was successfully performed without any major complications.
- Citation: Miura T, Hakamada K, Ohata T, Narumi S, Toyoki Y, Nara M, Ishido K, Ohashi M, Akasaka H, Jin H, Kubo N, Ono S, Kijima H, Sasaki M. Resection of a locally advanced hilar tumor and the hepatic artery after stepwise hepatic arterial embolization: A case report. World J Gastroenterol 2008; 14(22): 3587-3590
- URL: https://www.wjgnet.com/1007-9327/full/v14/i22/3587.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.3587
Locally advanced hilar tumor often involves the hepatic artery (HA) within the hepatoduodenal ligament, and a concomitant resection may be required for its cure. However, hepatic arterial resection is uncommon, because the reconstruction requires microvascular techniques[1–3] and major complications may occur[45]. Arterioportal shunting has reported as an alternative to microvascular reconstruction[67]. However, this approach also requires vascular reconstruction and could cause an occlusion. We herein report the use of stepwise arterial embolization as another alternative to microvascular reconstruction and arterioportal shunting after performing a hepatic arterial resection.
A 57-year-old female patient underwent a right colectomy for ascending colon cancer in March, 2001. In January, 2003, liver metastasis was noted in the left medial segment (Couinaud’s Segment 4; S4). She underwent a partial hepatectomy and ligation of the gastroduodenal and right gastric arteries for hepatic arterial infusion. In September, 2004, a recurrence in S4 was identified and a partial hepatectomy was carried out again. In September, 2005, a metastatic tumor appeared in S4 again and radiofrequency ablation therapy was performed.
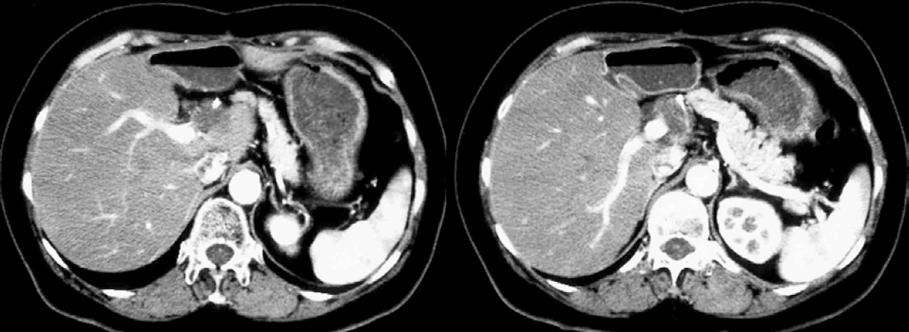
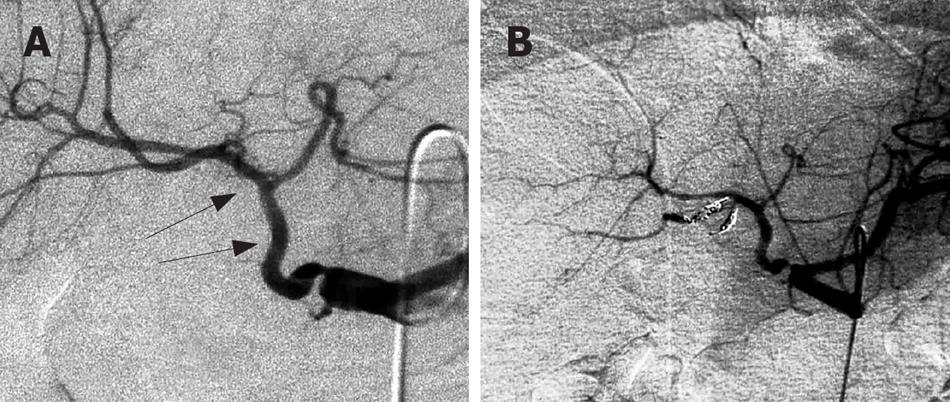
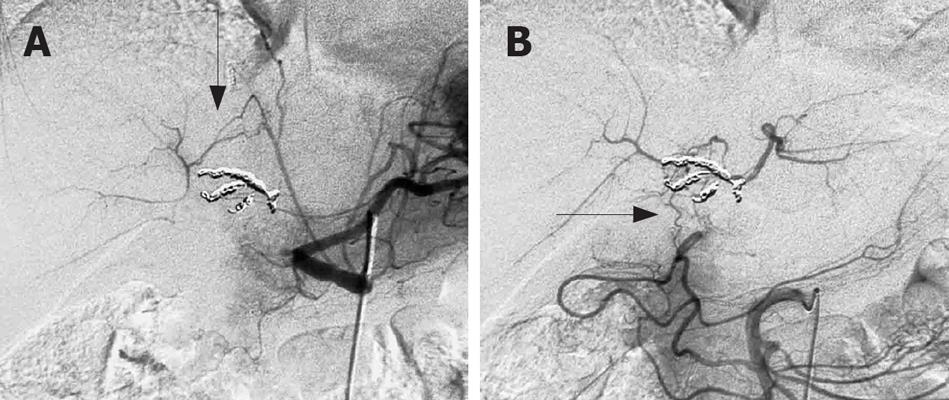
In April, 2006, a recurrent tumor was noted around the proper HA with invasion to the left hepatic duct and the proper and right HAs (Figure 1). After 5 mo of continuing chemotherapy, we decided to perform a radical resection since no tumor progression or other metastatic lesions were observed. For the radical resection, left hepatectomy and proper hepatic arterial resection were needed. To avoid surgery-related liver failure, we tried to form collateral hepatic arteries after stepwise arterial embolization of the HA. At first, the posterior right hepatic artery (PRHA) was embolized with interlocking detachable coils (IDC) and fibered platinum coils (FPC; Boston Scientific, USA) (Figure 2). We placed seven IDC with their diameter ranging from 2 mm to 4 mm and length ranging from 4 cm to 8 cm, and 3 FPC (straight) measuring 5 mm in length. Two weeks later, the branches of the PRHA were enhanced from the branches of the anterior right hepatic artery (ARHA) (Figure 3). After the development of collateral arteries was confirmed in the right liver, the ARHA was embolized with IDC and FPC. We placed nine IDC, with their diameter ranging from 2 mm to 5 mm and length ranging from 4 cm to 6 cm, and 4 FPC (straight) measuring 5 mm in length. Finally, the proper HA was occluded with IDC after confirming the formation of collateral flow from the inferior phrenic artery (IPA) and the superior mesenteric artery (SMA) was confirmed (Figure 4). We placed two IDC, 2 mm and 4 mm in diameter, 4 cm and 8 cm in length, respectively. After such embolization, the patient had no complications including hepatic dysfunction or liver abscess.
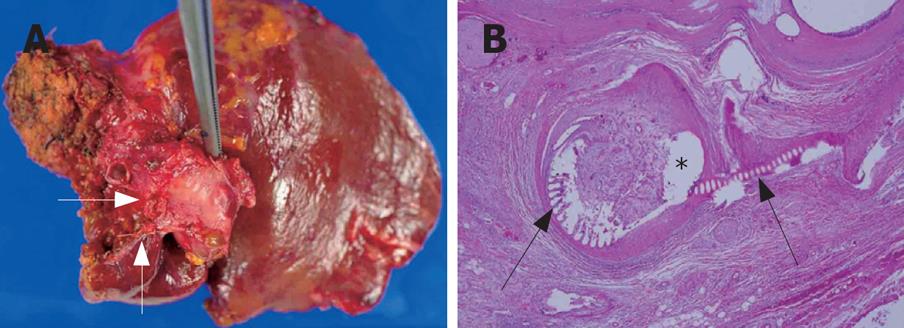
One month later, a left hepatectomy was performed with hepatic arterial resection. The tumor was located around the common, proper, anterior right and posterior right HA. Fortunately, the portal vein and bile duct were not resected because the tumor did not invade them. The operating time was 325 min. The operative blood loss was 1380 mL and no red blood cell transfusion was required. The serum concentration of aspartate aminotransferase and alanine aminotransferase one day after the operation was 381 U/L and 259 U/L, respectively, which returned to normal within 5 d. The maximum postoperative concentration of total serum bilirubin was 1.5 &mgr;mol/L. Fourteen days after the operation, a biloma from the cut margin of the liver was noticed and treated with percutaneous drainage. Thereafter, it improved and the patient was discharged 30 d after the operation without major complications.
The tumor measured 3.0 cm × 2.5 cm × 4.0 cm (Figure 5A). Histological examination of the resected specimen revealed tumor invasion of the HA (Figure 5B). Neural invasion also was observed. The radial margin was free of tumor. The histological diagnosis was mucinous adenocarcinoma compatible with metastasis of colon cancer.
Because hilar tumor approximates the HA, it easily spreads to it. It is necessary to excise the tumor with negative margins to cure it. A concomitant vascular resection could be employed whenever the tumor invades the HA supplying the remnant liver. It is necessary to preserve the hepatic arterial flow, as an interruption of the arterial flow can cause major complications, such as liver failure and liver abscess[89]. It was reported that arterial reconstruction using a microvascular anastomosis is useful[1–3]. However, the approach is difficult in cases in which the arterial diameter is small due to with multiple arterial stumps or the deep operative field is deep[4]. As an alternative, an arterioportal shunt has been reported with favorable results[67]. This procedure also requires vascular reconstruction with the possibility of fatal complications, including occlusion, aneurysm, or dissection[4–7].
Stepwise hepatic arterial embolization does not require a vascular surgical procedure, can eliminate the possibility of the above complications and decrease the complexity of the surgical procedure and the operating time. In addition, it makes possible to perform an en bloc resection of the tumor and lymph nodes around the proper and common HA. If an extra-hepatic bile duct resection with removal of the HA can sufficiently eradicate the tumor, an extensive hepatectomy would be unnecessary. Therefore, in regard to safety and potential cure, this approach is acceptable for a hilar tumor with hepatic arterial invasion.
Wachsberg et al[10] reported a case in which liver necrosis occurred after the right HA was occluded. it was reported that in most patients who undergo angiography within 1 or 2 wk after hepatic arterial ligation, collateral arteries are present and subsequent angiograms show progressive enlargement[11]. We scheduled embolization of the PRHA, ARHA, and proper HA at 2 week intervals. As a result, collateral pathways from ARHA to PRHA, IPA to PRHA, and SMA to ARHA were formed without complication.
This procedure also has some limitations. For example, whether collateral arteries form as expected. Takeuchi et al[12] reported that almost all patients have an extra-hepatic arterial supply from the IPA and SMA. Since intersegmental hepatic collateral arteries are formed after hepatic arterial embolization[13], collateral vessels should form as expected. However, if no collateral vessels are formed, an arterioportal shunt may be required.
Though this case involved a metastatic tumor, almost all cases of hilar tumor are associated with biliary cancer. Usually, the bile duct is excised and a bilioenteric anastomosis is performed. In the case of stepwise hepatic arterial embolization, the bile duct stump lacks of arterial blood flow via the hepatoduodenal ligament and is only supplied from collateral arteries through the liver. An impairment of the blood supply to the bile duct stump could cause disruption of the bilioenteric anastomosis. However, Plengvanit et al[11] showed that collateral vessels enter the liver peripherally after ligation of HA, and the blood fills the branches of HA to the occluded portion in a retrograde fashion. It is presumed that a breakdown of the bilioenteric anastomosis does not occur because sufficient arterial blood flow can reach the bile duct stump via the intrahepatic shunts which mainly come from the IPA. Because the left and right IPA contact the bare area of the liver segments 1, 2, and 7[14], this method is useful not only for the left trisegmentectomy with resection of the right hepatic artery but also for the right trisegmentectomy with resection of the left hepatic artery.
In conclusion, stepwise hepatic arterial embolization is one of the useful methods for performing resection of locally advanced hilar tumor invading HA, although the safety of the procedure needs to be confirmed in other cases.
| 1. | Yamanaka N, Yasui C, Yamanaka J, Ando T, Kuroda N, Maeda S, Ito T, Okamoto E. Left hemihepatectomy with microsurgical reconstruction of the right-sided hepatic vasculature. A strategy for preserving hepatic function in patients with proximal bile duct cancer. Langenbecks Arch Surg. 2001;386:364-368. |
| 2. | Yamamoto Y, Sugihara T, Sasaki S, Furukawa H, Furukawa H, Okushiba S, Nohira K. Microsurgical reconstruction of the hepatic and superior mesenteric arteries using a back wall technique. J Reconstr Microsurg. 1999;15:321-325. |
| 3. | Sakamoto Y, Sano T, Shimada K, Kosuge T, Kimata Y, Sakuraba M, Yamamoto J, Ojima H. Clinical significance of reconstruction of the right hepatic artery for biliary malignancy. Langenbecks Arch Surg. 2006;391:203-208. |
| 4. | Inomoto T, Nishizawa F, Sasaki H, Terajima H, Shirakata Y, Miyamoto S, Nagata I, Fujimoto M, Moriyasu F, Tanaka K. Experiences of 120 microsurgical reconstructions of hepatic artery in living related liver transplantation. Surgery. 1996;119:20-26. |
| 5. | Matsuda H, Yagi T, Sadamori H, Matsukawa H, Shinoura S, Murata H, Umeda Y, Tanaka N. Complications of arterial reconstruction in living donor liver transplantation: a single-center experience. Surg Today. 2006;36:245-251. |
| 6. | Kondo S, Hirano S, Ambo Y, Tanaka E, Kubota T, Katoh H. Arterioportal shunting as an alternative to microvascular reconstruction after hepatic artery resection. Br J Surg. 2004;91:248-251. |
| 7. | Iseki J, Noie T, Touyama K, Nakagami K, Takagi M, Ori T, Ooba N, Ito K. Mesenteric arterioportal shunt after hepatic artery interruption. Surgery. 1998;123:58-66. |
| 8. | Miyazaki M, Ito H, Nakagawa K, Ambiru S, Shimizu H, Yoshidome H, Shimizu Y, Okaya T, Mitsuhashi N, Wakabayashi Y. Unilateral hepatic artery reconstruction is unnecessary in biliary tract carcinomas involving lobar hepatic artery: implications of interlobar hepatic artery and its preservation. Hepatogastroenterology. 2000;47:1526-1530. |
| 9. | Tsuge H, Mimura H, Hamazaki K, Mori M, Kawata N, Orita K. Interruption of hepatic arterial blood flow after resection of pancreaticobiliary carcinoma. Hepatogastroenterology. 1995;42:966-974. |
| 10. | Wachsberg RH, Cho KC, Raina S. Liver infarction following unrecognized right hepatic artery ligation at laparoscopic cholecystectomy. Abdom Imaging. 1994;19:53-54. |
| 11. | Plengvanit U, Chearanai O, Sindhvananda K, Dambrongsak D, Tuchinda S, Viranuvatti V. Collateral arterial blood supply of the liver after hepatic artery ligation, angiographic study of twenty patients. Ann Surg. 1972;175:105-110. |
| 12. | Takeuchi Y, Arai Y, Inaba Y, Ohno K, Maeda T, Itai Y. Extrahepatic arterial supply to the liver: observation with a unified CT and angiography system during temporary balloon occlusion of the proper hepatic artery. Radiology. 1998;209:121-128. |
| 13. | Charnsangavej C, Chuang VP, Wallace S, Soo CS, Bowers T. Angiographic classification of hepatic arterial collaterals. Radiology. 1982;144:485-494. |
| 14. | Gwon DI, Ko GY, Yoon HK, Sung KB, Lee JM, Ryu SJ, Seo MH, Shim JC, Lee GJ, Kim HK. Inferior phrenic artery: anatomy, variations, pathologic conditions, and interventional management. Radiographics. 2007;27:687-705. |