Published online May 21, 2008. doi: 10.3748/wjg.14.3092
Revised: April 17, 2008
Published online: May 21, 2008
We describe here a case of 51-year-old woman with a symptomatic hepatic cyst that was misdiagnosed as a gastric submucosal tumor (SMT) with endoscopic ultrasound (EUS) and CT scan. The patient presented with an epigastric pain for two months. On endoscopy, a submucosal tumor was found on the cardia of the stomach. Based on EUS and abdominal CT scan, the lesion was diagnosed as a gastric duplication cyst or a gastrointestinal stromal tumor (GIST). The operative plan was laparoscopic wedge resection for the GIST of the gastric cardia. A cystic mass arising from the left lateral segment of the liver was found at the laparoscopic examination. There was no abnormal finding at the gastric cardia. She was treated by laparoscopic hepatic wedge resection including the hepatic cyst using an endoscopic linear stapler.
- Citation: Park JM, Kim J, Kim HI, Kim CS. Hepatic cyst misdiagnosed as a gastric submucosal tumor: A case report. World J Gastroenterol 2008; 14(19): 3092-3094
- URL: https://www.wjgnet.com/1007-9327/full/v14/i19/3092.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.3092
Although submucosal tumor (SMT) is benign and asymptomatic, it should be evaluated by follow-up examinations. Certain gastric SMTs that are considered to be gastrointestinal stromal tumor (GIST) or symptomatic SMT require operative intervention because it is very difficult to confirm its malignant potential with endoscopic biopsy[1].
SMT is usually asymptomatic and most often discovered accidentally at surgery and autopsy or at performing diagnostic procedures. Unspecific symptoms, such as abdominal pain, obstruction, hemorrhage and intussusception, may occur. Two advanced tools have been generally accepted for the diagnosis and treatment of gastric SMTs. Endoscopic ultrasound (EUS) is one useful accurate diagnostic method, and the other is a laparoscopic procedure that allows minimally invasive treatment for SMTs.
Extragastric compression may mimic the symptoms and endoscopic findings of gastric SMTs. EUS and CT scan can accurately differentiate extragastric compression from true SMTs. However, cases may arise that cannot be differentiated even after various methods are used. We report here a case of hepatic cyst which was misdiagnosed as a gastric submucosal tumor in a patient undergone various diagnostic modalities, including endoscopy, EUS and abdominal CT scan.
A 51-year-old woman presented with epigastric pain for two months. Initial examination showed that she had tenderness in the epigastrium. The patient was taking no medications. Her past medical history and familial history were unremarkable. Routine laboratory data on admission did not show any abnormal findings.
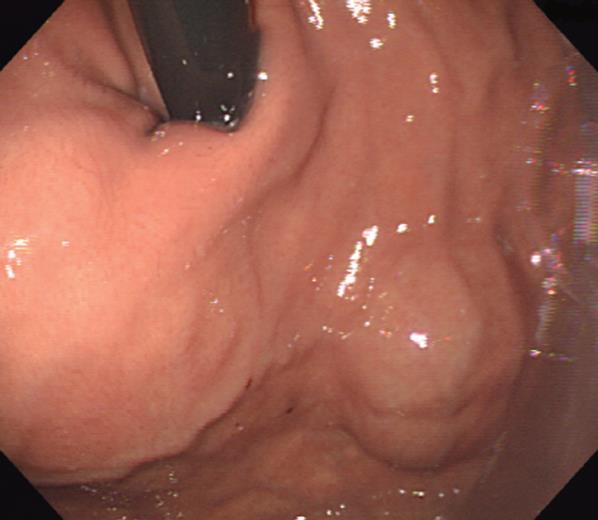
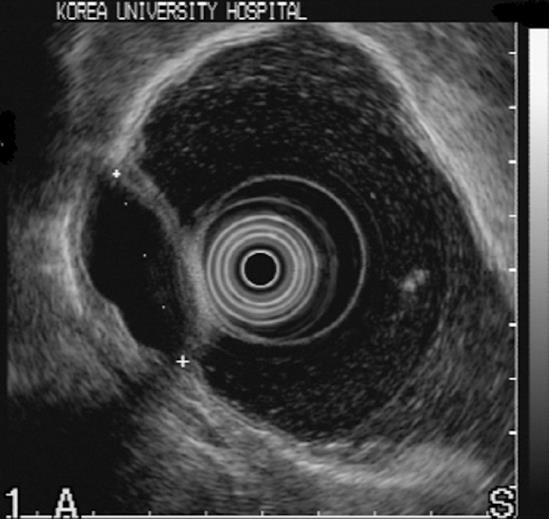
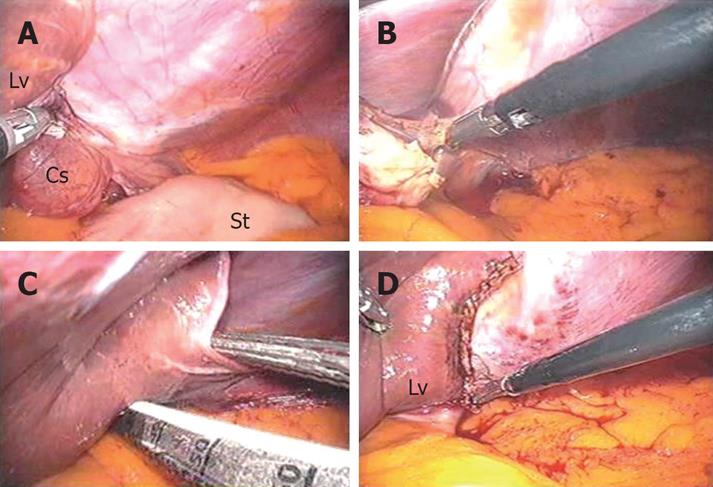
Gastrointestinal endoscopy revealed a submucosal tumor in the cardia of the stomach (Figure 1). On EUS, the lesion was a hypoechoic mass (3.6 cm in diameter) suggestive of a gastric duplication cyst or a GIST (Figure 2). Abdominal CT scan showed a cystic lesion at the submucosal layer of the gastric cardia, and the impression of the radiologist was a gastric duplication cyst or a GIST with necrosis (Figure 3). The operative plan was laparoscopic wedge resection for the GIST of the gastric cardia. Laparoscopic exploration was performed for the patient under general anesthesia. On the laparoscopic examination, a cystic mass arising from the left lateral segment of the liver was found (Figure 4A). There was no abnormal finding at the gastric cardia. After the triangular ligament was divided with electrocautery (Figure 4B), wedge resection of the left lateral segment of the liver, including the hepatic cyst, was performed using an endoscopic linear stapler (Figure 4C and D). There was no specific complication during the procedure. An oral diet was permitted on the 1st postoperative day. She was discharged from the hospital on the 3rd postoperative day. The mass was diagnosed as a simple hepatic cyst.
Hepatic cysts are usually asymptomatic and not associated with defective hepatic function. They are incidentally found at laparotomy or laparoscopy, and even at routine ultrasound or CT scan. However, they may become symptomatic if they grow. The symptoms depend on the size and location of the cyst. The patients may have a vague upper abdominal pain, a right upper quadrant abdominal mass, postprandial fullness, dyspnea and vomiting[2]. In our case, the hepatic cyst was located at the edge of the left lateral segment of the liver and caused epigastric pain by compressing the gastric cardia.
A left hepatic cyst may rarely mimic a SMT arising from the gastric cardia or fundus[3]. Various conditions can mimic gastric SMT due to extragastric compression. The most common source of extraluminal compression in the stomach is from the spleen and splenic vessels[45]. Other sources of extraluminal compression include normal abdominal organ structures such as liver and gallbladder, and pathologic lesions such as tumors, abscesses, pancreatic pseudocysts and enlarged lymph nodes.
Whether the lesion is due to intramural or extrinsic compression can be distinguished by changing the patient’s position to see if the location and appearance of the mass change. Also, a change in appearance of the mass with either air insufflation or deflation is helpful in determining if the lesion is due to extrinsic compression, yet it can be difficult to differentiate. It was reported that the sensitivity and specificity of endoscopy are 87% and 29%, respectively for distinguishing intramural lesion from extramural compression[6]. On the other hand, EUS is 100% accurate for differentiating extragastric compression from submucosal tumor and for identifying the compressing organ[7].
In our case, however, the hepatic cyst was misdiagnosed as a GIST although various diagnostic methods such as EUS and CT scan were used.
In the best of our knowledge, this is the first report of a patient with asymptomatic left hepatic cyst that was misdiagnosed as a GIST and treated by laparoscopic resection of the hepatic cyst.
Surgical treatment for hepatic cyst is indicated when the cyst causes complaints and the diameter is at least 5 cm or rapid growth is observed. Possible surgical treatments of the cyst include unroofing, extirpation or resection of the cyst. Conservative treatment (aspiration, sclerotherapy and percutaneous drainage) is not often recommended because of frequent relapse of the disease[28].
With the advances in minimally invasive surgery, laparoscopic unroofing is generally recommended for the treatment of hepatic cyst[8]. In our case, since the cyst was located at the left edge of the liver and relatively small, laparoscopic wedge resection of the hepatic cyst was easily performed by using an endoscopic linear stapler.
In conclusion, a left hepatic cyst may mimic a SMT arising from the gastric cardia and cause nonspecific abdominal symptoms. For such a case, laparoscopic procedure is a useful option for making the accurate diagnosis, and laparoscopic resection of the hepatic cyst is a minimally invasive treatment.
| 1. | Ponsaing LG, Hansen MB. Therapeutic procedures for submucosal tumors in the gastrointestinal tract. World J Gastroenterol. 2007;13:3316-3322. |
| 2. | Caetano-Junior EM, Linhares MM, Matos D, Schraibman V, Matone J, Saad SS. Laparoscopic management of hepatic cysts. Surg Laparosc Endosc Percutan Tech. 2006;16:68-72. |
| 3. | Park SS, Ryu WS, Kwak JM, Lee SI, Kim WB, Mok YJ, Choi JW, Park JJ, Bak YT. Gastric fundus impression caused by a hepatic cyst mimicking gastric submucosal tumor. South Med J. 2006;99:902-903. |
| 4. | Hwang JH, Kimmey MB. The incidental upper gastrointestinal subepithelial mass. Gastroenterology. 2004;126:301-307. |
| 5. | Rosch T, Lorenz R, von Wichert A, Classen M. Gastric fundus impression caused by splenic vessels: detection by endoscopic ultrasound. Endoscopy. 1991;23:85-87. |
| 6. | Rosch T, Kapfer B, Will U, Baronius W, Strobel M, Lorenz R, Ulm K. Accuracy of endoscopic ultrasonography in upper gastrointestinal submucosal lesions: a prospective multicenter study. Scand J Gastroenterol. 2002;37:856-862. |
| 7. | Motoo Y, Okai T, Ohta H, Satomura Y, Watanabe H, Yamakawa O, Yamaguchi Y, Mouri I, Sawabu N. Endoscopic ultrasonography in the diagnosis of extraluminal compressions mimicking gastric submucosal tumors. Endoscopy. 1994;26:239-242. |
| 8. | Szabo LS, Takacs I, Arkosy P, Sapy P, Szentkereszty Z. Laparoscopic treatment of nonparasitic hepatic cysts. Surg Endosc. 2006;20:595-597. |