INTRODUCTION
The term of undifferentiated connective tissue disease (UCTD) is used to define conditions characterized by the presence of signs and symptoms suggestive of a systemic autoimmune disease that do not satisfy the classification criteria for defined connective tissue diseases (CTD), such as systemic lupus erythematosus (SLE), Sjögren’s syndrome (SS), rheumatoid arthritis (RA) and others. Patients may present with systemic symptoms, such as fatigue, fever, or weight loss, preceding any organ involvement. The most common symptoms include arthralgias, unexplained or undifferentiated polyarthritis, Raynaud syndrome, mucocutaneous manifestations, and sicca symptoms. However, it is unusual for a patient with UCTD to have major organ involvement[1]. Here, we report a case of UCTD-related hepatic injury.
CASE REPORT
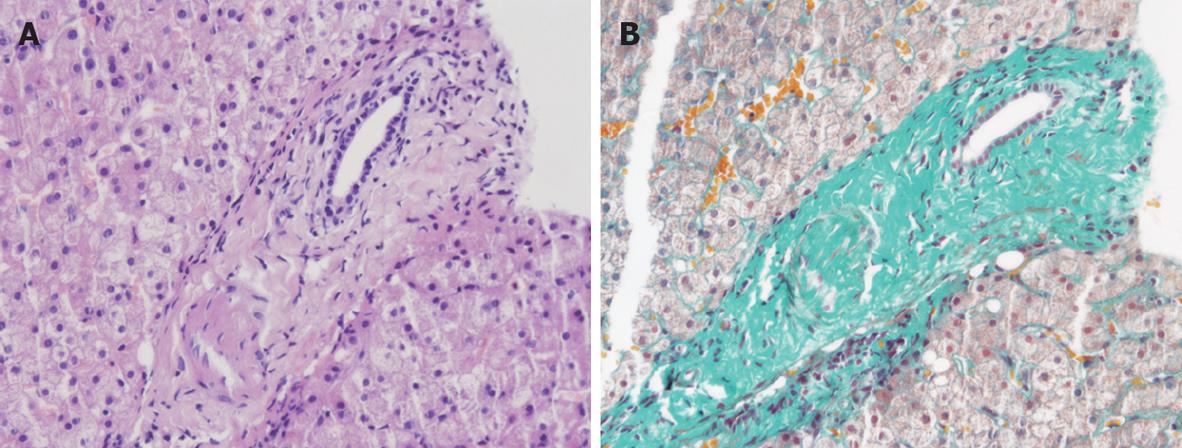
A 58-year-old woman was admitted to our hospital with chief complaints of fatigue, anorexia, low-grade fever and skin rashes for two months. At physical examination, she had a BP of 118/79 mmHg, a pulse of 82 beats/min, a respiratory rate of 16, and a temperature of 37.3°C. MI was 25.2. Red maculae and desquamation were found on her face, upper limbs and buttocks. Family history was negative for rheumatic or inherited liver disease. She had a past medical history of psoriasis, hypertension, acute hepatitis A and blood transmission, but no history of ethanol consumption, no exposure to possible hepatotoxic drugs. She accepted left knee joint replacement three years ago because of osteoarthritis. Abdominal ultrasonography revealed echo enhancement of the liver and mild splenomegaly, no ascites was detected. Chest CT examination revealed interstitial pneumonia and hydropericardium. Laboratory analysis revealed a white blood cell count of 9.86 × 109/L, eosinophile of 10.1%, hemoglobin of 108 g/L, ESR of 90 mm/h, aspartate aminotransferase level of 157 U/L, alanine aminotransferase level of 141 U/L, albumin of 27.1 g/L, globulin of 34.7 g/L, pre-albumin of 69 mg/L, seropositivity for antinuclear antibodies with a titer of 1:320. Total bilirubin, prothrombin time, renal function and urine routine test were within normal range. Investigations for the underlying cause of her hepatic injury including alfa-fetoprotein, CEA, thyroid function, cytomegalovirus, EB virus, adenovirus antineuritic cytoplasmic antibody, antibodies to liver/kidney microsome, smooth muscle antibodies, anti-neutrophil cytoplasmic antibody, immunoglobulin pattern, hepatitis B, C and E serology were all negative or within the normal range. Liver biopsy showed the features consistent with those of connective tissue diseases-related polyangitis (Figure 1). These findings suggested that she had UCTD-related hepatic injury. The patient was treated with a low dose of oral prednisone (40 mg/d) at the beginning. Three weeks later, the dose of oral prednisone was decreased to 30 mg/d. Her symptoms and laboratory tests improved markedly four weeks later. The levels of hemoglobin, albumin and pre-albumin were elevated to 107 g/L, 31.7 g/L and 158 mg/L, respectively. The levels of white blood cells, eosinophile, PLT, ESR, ALT and AST were decreased to 8.72 × 109/L, 6.4%, 356 × 109/L, 44 mm/h, 100 U/L, and 86 U/L, respectively. She was discharged on the 40th d. Twenty-eight days after discharge, follow-up laboratory tests showed that the levels of ESR and eosinophiles were decreased to their normal range. The levels of ALT and AST were also decreased to 60 U/L and 70 U/L, respectively.
Figure 1 Biopsy of the liver showing dense fibrosis of intrahepatic portal tracts with obliteration of portal vein channels, consistent with connective tissue diseases-related polyangitis with HE staining (A) and Massion trichrome staining (B).
DISCUSSION
The most characteristic symptoms of UCTD are arthritis, arthralgias, Raynaud’s phenomenon, and leukopenia. It is clear that the clinical profile of UCTD is characterized by the absence of major organ involvement. During follow-up, the symptoms may improve or mildly flare spontaneously. A positive ANA is common, with a positive rate ranging from 60%-100%, and a stable profile over time[2]. After reviewing the UCTD literature, Mosca et al[3] proposed that the preliminary classification criteria for UCTD include: (1) signs and symptoms suggestive of a connective tissue disease, but not fulfilling the criteria for any defined CTD, (2) positive antinuclear antibodies, and (3) a disease course of at least 3 years. As these are mild and benign conditions, only a small number of UCTD patients are treated. The most widely used drugs are NSAID (40%), corticosteroids (30%-50%) and antimalarials at a low dose (10%-30%)[45]. Our patient was treated with a low dose of prednisone. Four weeks later, both symptoms and laboratory findings were improved markedly. According to the above findings, the diagnosis of UCTD was established.
Our report was evaluated for hereditary (Wilson’s disease, α-1 antitrypsin deficiency, and genetic hemochromatosis), infections (hepatitis B, C and CMV, EBV), drinking history and drug-induced liver injury, some of which may have autoimmune features. These possible causes for liver damage can be excluded. Likewise, although echogram of the liver showed fatty change, histological findings did not show steatosis in hepatocytes. However, even after careful exclusion of the above stated etiologies, the question remains whether the patient should be diagnosed having a primary liver disease associated with autoimmune or clinical and laboratory features and liver involvement should be considered manifestations of UCTD. The main pathogenetic dilemma is autoimmune hepatitis (AIH) and UCTD-related hepatic injury, although they have some common features of autoimmune syndrome. In this paper, we present a case of a patient with hepatic injury. UCTD is a systemic autoimmune condition characterized by a mild clinical profile and a simplified autoimmune repertoire. Although UCTD is generally benign, it may progress to CTD and changes in the disease course may occur. A small number of patients presenting with an undifferentiated profile will develop CTD during the first year follow-up. However, an average of 75% patients will maintain an undifferentiated clinical course. These patients may be defined having a stable UCTD. Bodolay et al[6] followed up 665 Hungarian patients with UCTD and found that most of the UCTD patients do not develop a definite CTD, but have new clinical and serological manifestations during the follow-up period and UCTD progresses to different types of specific CTD in one-third of them. Margaret et al[7] reviewed 11 patients meeting the diagnostic criteria for AIH. Of these 11 patients, three with a definitive diagnosis of AIH developed systemic CTD, one developed systemic lupus erythematosus (SLE) with vasculitis and peripheral neuropathy, 2 developed limited scleroderma, and 3 developed UCTD and interstitial lung disease. There appears to be a shared susceptibility of alleles to AIH and CTD in addition to the shared positive autoantibodies. Therefore, it is necessary to exclude the possibility of AIH if the definite diagnosis of UCTD-related hepatic injury is made. In the present case, the possibility of a diagnosis of AIH should be considered. The criteria for the diagnosis of AIH in adult patients have been established by the International Autoimmune Hepatitis Group (IAIHG)[8]. The diagnosis of UCTD-related hepatic injury is based on the presence of characteristic laboratory and liver histology features and the exclusion of conditions that resemble AIH. Interface hepatitis is the hallmark of AIH[9]. However, the liver biopsy did not show interface hepatitis, which is essential for the diagnosis of AIH. Therefore, the diagnosis of AIH cannot be established. Instead, the diagnosis of UCTD- related hepatic injury can be established. Laing et al[10] reported that potential risk factors for UCTD are found in women implanted medical devices, of which, non-silicone-containing devices, non-silicone-containing artificial joints (OR = 5.01, 95% CI =1.60-15.71) and orthopedic metallic fixation devices (OR = 1.95, 95% CI = 1.05-3.60) are associated with UCTD. Laing et al[10] have also reviewed the intervals between surgical implantation of artificial joints and diagnosis of UCTD (mean, 4.5 years; range, 3.0-6.9 years). Our patient received left knee joint replacement because of a 3-year history of osteoarthritis. Whether this plays a role in the pathogenesis of UCTD needs further study.
Just as most of other connective-tissue diseases, the pathogenesis of UCTD is unclear. Like most connective-tissue diseases, the theory and research have been concentrated on genetically susceptible hosts, T- and B-cell abnormalities, and environmental triggers, such as ultraviolet light or infection. In general, activities are not restricted unless specific functional limitations, such as interstitial lung disease, associated with UCTD are present[11]. Therefore, UCTD-related hepatic injury is an auto-reactive tissue injury which may arise via either the TH1 pathway (leading to cell-mediated cytotoxic reactions) or the TH2 pathway (resulting in antibody-mediated cell damage). These processes are under a certain form of immunoregulatory control which normally maintains self-tolerance by “switching off” the autoimmune response, although whether this involves discrete subsets of “suppressor” T lymphocytes is still controversial[12]. Whether the above factors induce UCTD-related hepatic injury is uncertain, in part because the pathogenetic mechanism underlying the development of these two conditions is poorly understood.
In conclusion, we report this case for its unusual hepatic injury after UCTD. UCTD-related hepatic injury should be considered in the differential diagnosis of connective tissue diseases with abnormal liver function tests. Low-dose prednisone can effectively improve both symptoms and laboratory findings of UCTD.