CASE REPORT
A 64-year-old man was admitted with an abrupt onset of pain in the left midsection of the abdomen. He began to feel sharp pain after dinner, which was accompanied with alcohol. The pain persisted for 8 h and became increasingly unbearable. Blood tests showed serum amylase (AMY) of 501 IU/L, lipase (LIP) 779 IU/L and hemoglobin (Hb) 171 g/L. He was diagnosed as acute necrotizing pancreatitis based on the blood tests and findings at computer tomography (CT) scan (Figure 1A). The patient was transferred to the Department of Integrated Traditional Chinese Medicine and Western Medicine for treatment of pancreatitis, which is a special expertise of this department. The next day, the patient experienced sudden pain without any precipitating factor, accompanied with dyspnoea. Blood tests revealed that the Hb level had dropped from 171 g/L to 40 g/L. From that point on, the patient began to deteriorate rapidly and developed features of hemorrhagic shock despite continuous transfusion of 2000 mL whole blood. Severe intra-abdominal bleeding was suspected as the principal cause of his symptoms. In view of the high mortality rate of such a complication, one group of surgeons recommended prompt surgical intervention. However, after consultation with the family members we arranged an emergent angiography to identify the bleeding source. During the procedure, a ruptured pseudoaneurysm of the superior mesenteric artery (SMA) was identified, with extravasation of contrast medium from the vessel (Figure 2A and B).
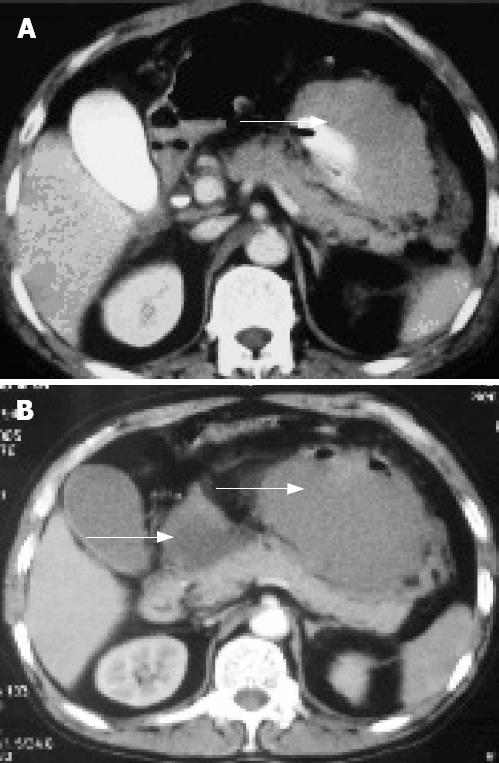
Figure 1 CT scan.
A: Presence of the postperitoneal hematoma (arrow); B: Increase in the size of postperitoneal hematoma and presence of a pseudocyst (arrows).
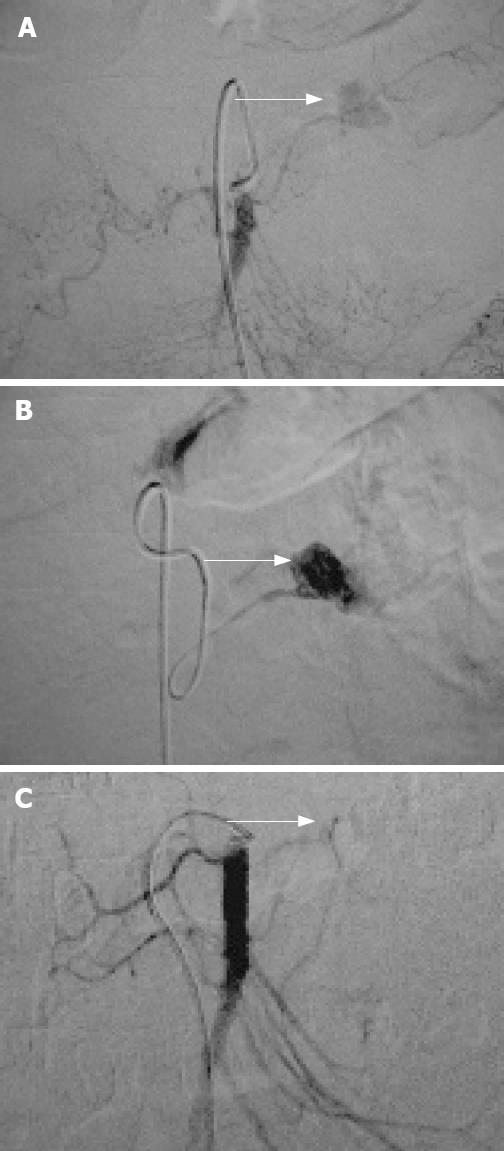
Figure 2 Angiography.
A: SMA angiography shows a pseudoaneurysm in a branch of the SMA with extravasation of the contrast (arrow); B: Subselective angiography illustrates extravasation of the contrast more clearly (arrow); C: After embolization of the damaged artery, there is cessation of extravasation of the contrast, with disappearance of the nidus (pseudoaneurysm) (arrow).
Gelatin sponge pieces were infused in order to embolize the ruptured artery, and the bleeding stopped (Figure 2C). After the interventional treatment and transfusion of 400 mL of fresh blood, the Hb increased to 93 g/L. The patient was transferred to the Intensive Care Unit. Six days later, the patient was in stable condition but experienced continuous dull abdomen pain. Repeat CT scan showed that the size of the postperitoneal hematoma had increased from 6 cm to 8 cm, and a 3 cm parapancreatic cyst was noted (Figure 1A and B). The patient was operated upon to evacuate the cyst, hematoma and the necrotic tissues. A communication was made with the jejunum to create a pancreaticojejunostomy. The patient recovered gradually and was discharged from the hospital 2 wk later.
DISCUSSION
Acute pancreatitis is an inflammatory condition, which leads to acinar cell damage, interstitial edema and hemorrhage. Some patients may develop severe acute pancreatitis accompanied with multiple organ dysfunction syndrome. Acute pancreatitis is initiated by the activation of pancreatic enzymes in the acinar cells. Local inflammation, caused by activation of trypsinogen to trypsin, is followed by the activation of inflammatory mediators. These mediators and the associated damage is not restricted to the pancreatic tissue, but may involve other organs, particularly the lungs, liver, and blood products, which are responsible for the systemic manifestations of this condition[1].
Rupture of a pancreatic pseudoaneurysm is a rare complication of pancreatitis, and is associated with poor prognosis. The mortality correlates with the severity of the pseudoaneurysm (acute pancreatitis), and the overall mortality of this complication (severe acute pancreatitis) is about 7.8%. Angiography is usually required for confirmation of the diagnosis. Non-invasive imaging techniques such as color Doppler ultrasound and contrast-enhanced CT with sagittal or coronal reconstruction are also useful in the diagnosis of pancreatic pseudoaneurysm associated with acute necrotizing pancreatitis. Despite the advent of other imaging modalities, CT is the most effective technique to evaluate the lesion after pancreatic surgery[2–5]. In addition, CT may demonstrate early (leakage of anastomosis, pancreatico-jejunal fistula, hemorrhage, acute pancreatitis of the remnant pancreas, peritonitis) and late (chronic fistula, abscess, aneurysms, anastomotic bilio-enteric stenosis, perianastomotic ulcers, biloma, and intra-abdominal bleeding) complications. Magnetic resonance is an alternative imaging modality when renal insufficiency or contrast sensitivity precludes the use of iodinated contrast material or when assessment of the biliary tree is the primary focus of the study. However, these imaging techniques do not obviate the need for diagnostic and therapeutic angiography[6].
With respect to therapeutic choices, endoscopic papillotomy and endoscopic removal of biliary stones is the gold standard in the treatment of gallstone-related acute pancreatitis[67]. For other causes of acute pancreatitis, medical treatment should be started as early as possible with intensive care management in patients with severe acute pancreatitis. The optimal treatment is controversial. Surgical and interventional treatments, either alone or as temporizing techniques with subsequent surgery are some of the therapeutic options. However, in patients with necrotizing pancreatitis, angiographic embolization has been found to be very useful[689], since surgical ligation or repair of the bleeding vessel is complicated by higher rebleeding rates (46%) compared to partial pancreatectomy (17%). In patients with infected pancreatic necrosis, hemorrhage or peritonitis, surgery is the only therapeutic option, while the role of surgical treatment in the presence of sterile pancreatic necrosis accompanied with multiple organ dysfunction syndrome, which is unresponsive to medical therapy, remains unclear. Complications such as bleeding and bowel perforation are seen mostly in patients who undergo several reoperations[10–12]. Surgery in patients with necrotizing pancreatitis carries a high mortality (about 21% for the operation[13–15]). Surgical procedures are extremely unsafe when such patients develop acute gastrointestinal bleeding. However, angiography is the gold standard therapeutic approach in such patients. More importantly, angiography does little harm and has the highest chance of stopping bleeding in situations such as that of our patient.
Our patient was already in shock despite rapid blood transfusions when he was brought to the angio-room. As soon as we succeeded in embolizing the feeding artery, the patient’s blood pressure began to improve and it was soon restored to the normal level. The subsequent treatment after embolism is as important as stopping the bleeding itself. In the present case, the patient required further surgery and intensive care treatment, resulting in gradual improvement of the patient’s condition.
In summary, the present case report demonstrates that interventional treatment is an effective treatment for patients with acute necrotizing pancreatitis complicated with intra-abdominal bleeding, especially in patients who are in poor condition and those who cannot tolerate laparotomy. We wish to emphasize that stopping the bleeding is only the first step in the treatment of such patients and a close cooperation between the physicians and surgeons is required for optimal results.