Published online Apr 14, 2008. doi: 10.3748/wjg.14.2284
Revised: February 18, 2008
Published online: April 14, 2008
Two patients with tuberculous abscess in the hepatoduodenal ligament were studied. Both patients underwent contrast-enhanced computed tomography (CT) scan. The abscess showed a low density with an irregular thick wall in the hepatoduodenal ligament on CT images, the margin was poorly defined. Contrast-enhanced CT images showed the contrast-enhanced thick wall, homogeneous and peripheral-enhanced lymph nodes. Although features of the tuberculous abscess in the hepatoduodenal ligament could be conspicuously shown with contrast-enhanced CT, further experience is needed to evaluate the potential value of CT in detecting early tuberculous abscess in relation to other entities in the hepatoduodenal ligament.
- Citation: Dong P, Wang B, Sun YQ. Tuberculous abscess in hepatoduodenal ligament: Evaluation with contrast-enhanced computed tomography. World J Gastroenterol 2008; 14(14): 2284-2287
- URL: https://www.wjgnet.com/1007-9327/full/v14/i14/2284.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.2284
The incidence of tuberculosis is increasing[1–4]. Abdominal tuberculosis can affect the gastrointestinal tract, peritoneum and lymph nodes. Lymphadenopathy is the most common manifestation of abdominal tuberculosis[56]. To our knowledge, there are no reports on the computed tomography (CT) appearance of tuberculous abscess in the hepatoduodenal ligament in the English radiologic literature. We describe in the paper the CT findings in a series of tuberculous abscesses in the hepatoduodenal ligament.
A 24-year-old man had weight loss, easy fatigability, night sweats, and obscure abdominal pains for three months, but no clinically palpable abdominal mass.
Contrast-enhanced CT was performed on a 16-detector spiral CT scanner (Siemens Sensation). The image protocol consisted of dual-phase CT scan. Medrad-100 power injector was used. Contrast material was Ultravist (Schering Germany, 300 mgI/mL). The range of CT scan covered the upper and middle abdomen. CT parameters were 120 KV, 165 eff mAs, 0.5 s/360°, 16 mm × 0.75 mm, 1 mm multi-planar reconstruction (MPR) slice width. CT scan was performed with intravenous contrast material administered as a bolus. Oral contrast material (1.2% angiografin) was administrated. Images were viewed at a window width setting of 400 HU and a window level setting of 50 HU.
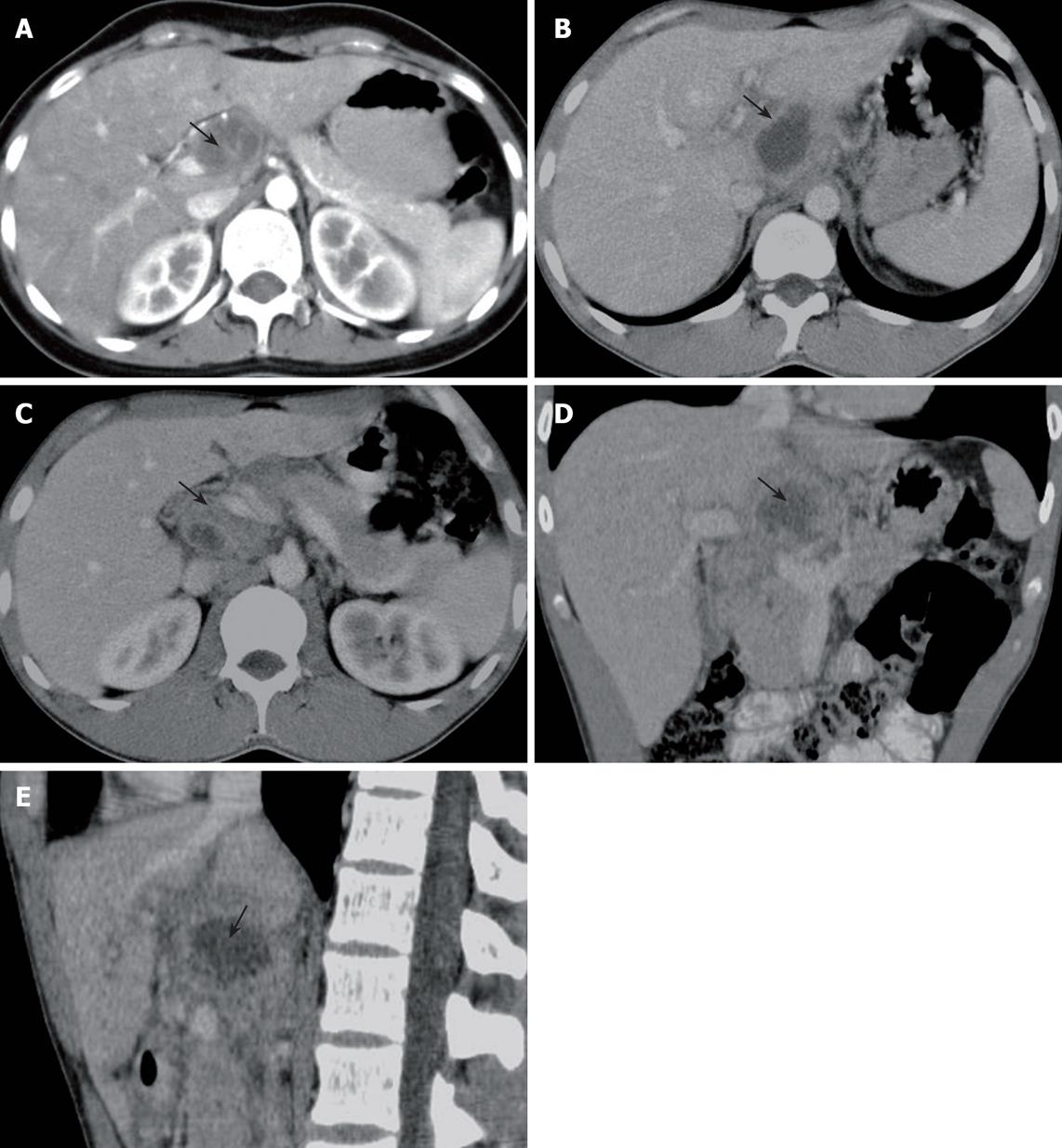
Contrast-enhanced CT showed a less dense mass with thick enhanced irregular walls in the hepatoduodenal ligament. The mass measured 3.9 cm × 2.8 cm with its margin poorly defined. The interface between the mass and around organs was not clear. Gas collection was not shown. Enlarged lymph nodes were detected in the portacaval space, gastrohepatic ligament, peripancreatic and upper paraaortic region. Some of them had peripheral enhancement and necrosis in the center (Figure 1A-E).
Operation on abdominal region was performed. Macroscopic pathological examination showed that the mass was tightly adherent to the hepatoduodenal ligament. Enlarged lymph nodes were found. Thirty mL of pus was aspirated from the mass. Microscopic examination revealed that the mass was inflammatory, and bacterial culture showed tuberculosis.
A 30-year-old man had fever and obscure abdominal pain for two months with no clinically palpable abdominal mass.
Contrast-enhanced CT was performed on a spiral CT scanner (Elscint HeliCAT Flash). The image protocol consisted of venous phase. Power injector (MCT Plus, Meddred, Pittsburg) was used. Contrast material was Ultravist (Schering Germany, 300 mgI/mL). The range of CT scan covered the upper and middle abdomen. CT parameters were 120 KV, 250 mA, pitch 1. CT scan was performed with intravenous contrast material administered as a bolus. Oral contrast material (1.2% angiografin) was administrated. Images were viewed at a window width setting of 400 HU and a window level setting of 50 HU.
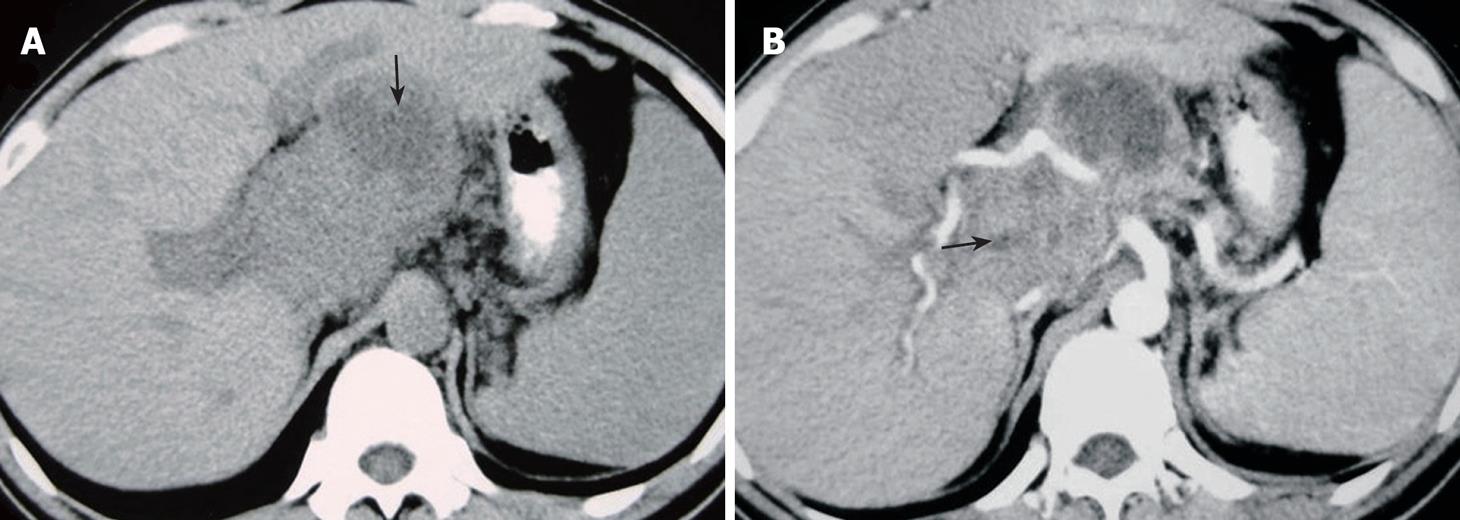
Contrast-enhanced CT showed a less dense mass with thick enhanced irregular walls in the hepatoduodenal ligament. The mass measured 4.1 cm × 2.7 cm with its margin poorly defined. The interface between the mass and surrounding organs was not clear. Gas collection was not shown. Enlarged lymph nodes were detected in the portacaval space, gastrohepatic ligament, which had peripheral enhancement (Figure 2A and B).
Operation on abdominal region was performed. Macroscopic pathological examination showed that the mass was tightly adhered to the hepatoduodenal ligament. Enlarged lymph nodes were found. Twenty mL of pus was aspirated from the mass. Microscopic examination revealed that the mass was tuberculosis.
Both patients gave their written informed consent.
Tuberculosis demonstrates a variety of clinical and radiologic features depending on the involved organ and has a known propensity for dissemination from its primary site. Thus, tuberculosis can mimic a number of other disease entities, and it is important to be familiar with the various radiologic features of tuberculosis to establish its diagnosis early and accurately[7].
Lymphadenopathy is the most common manifestation of abdominal tuberculosis[56]. Mesenteric, omental and peripancreatic lymph nodes are most commonly involved[5]. Abdominal tuberculosis may be transmitted by three major routes. The first is ingestion of material infected with tubercle bacilli which are carried from a lesion in the intestinal submucosal layer to the lymph nodes draining that segment of the bowel. Drainage is usually from lymphatics of the ileocecum, jejunum, ileum, and right side of colon to the peripancreatic and superior mesenteric lymph nodes. The second route of transmission is hematogenous spread. Bacteria are disseminated from a distant site of infection, usually the lungs, to the abdominal lymphatic system. Because this process is systemic, it may cause infection of mesenteric lymph nodes. In the third route of transmission, infection can spread directly to the abdominal lymph nodes from the serosa of adjacent infected structures[5]. In this study, two patients had non-disseminated tuberculosis and CT showed enlarged lymph nodes in the portacaval space, gastrohepatic ligament, peripancreatic and upper paraaortic region. So, the anatomic distribution of this disease closely parallels to the route of tuberculous infection.
The nodes are usually large and multiple, and most commonly demonstrate peripheral enhancement with central areas of low attenuation on contrast-enhanced CT images[5]. Pathologic findings from surgically obtained specimens of tuberculous lymphadenopathy indicate that caseation or liquefactive substances at the center of enlarged lymph nodes have a low attenuation that presumably results from insufficient blood supply, whereas peripheral inflammatory lymphatic tissue has a higher attenuation on enhanced CT that results from the preserved blood supply[8]. In this study, both cases were accompanied with enlarged lymph nodes, suggesting that the tuberculous abscess may be due to the coalescence of the involved lymph nodes.
Cystic lesions, including pseudocysts, necrotic tumors, and cysts of the pancreas and/or adjacent organs, must be differentiated from tuberculous abscess in the hepatoduodenal ligament. Pseudocyst is a unilocular, round mass with a uniform wall, and can be found in patients with clinical and laboratory evidence of pancreatitis. A well-defined rind suggests a pseudocyst or abscess, and gas bubbles suggest an abscess. CT demonstrates small calcification and fat in the teratomas located in the hepatoduodenal ligament area, and its border is round and sharp[9–11]. CT of extension of gastrointestinal stromal tumors displays extraluminal growth, inhomogeneous enhancement, absence of calcifications and lymph node metastases[12]. Congenital cysts (duplication, mesenteric, omental, or choledochal) may be localized to the hepatoduodenal ligament area. However, the history, clinical findings and the absence of enlarged lymph nodes do not suggest tuberculosis[11]. Serous and mucinous cystadenomas are encapsulated and lobulated masses, showing marked contrast-enhancement of the solid portion. Cystadenocarcinoma is seen as a multilobular, septate, thick-walled cyst or cystic neoplasm with multiple low-density areas. Dilatation of the main pancreatic duct may be seen[10]. The radiologic pattern of tuberculous lymphadenitis can also be seen with lymphoma[7]. The enhancement patterns of untreated lymphomas are homogeneous. In patients with lymphoma who have undergone therapy, central low attenuation may be found within nodes, simulating tuberculous lymphadenopathy. So, it is important to know the history[13–16].
It was reported that tuberculous lymphadenopathy has the following clinical characteristics[17]: (1) some patients have a history of TB and most of them come from areas with a high prevalence of active tuberculosis; (2) patients often suffer from epigastric pain, fever and weight loss; (3) ultrasound and CT scan show enlarged nodules, sometimes with focal calcification. In this study, a patient had weight loss, fatigability, night sweats, and obscure abdominal pains, while the other patient had fever and obscure abdominal pains. Both patients had no clinically palpable abdominal mass.
In summary, tuberculous abscess in the hepatoduodenal ligament is a less dense mass with thick enhanced irregular walls, its margin is poorly-defined, and the interface between the mass and around organs is not clear. It is important to show the peripheral enhanced lymph nodes for its early and accurate diagnosis.
| 1. | Goodman PC. Tuberculosis and AIDS. Radiol Clin North Am. 1995;33:707-717. |
| 2. | Collins FM. Tuberculosis: the return of an old enemy. Crit Rev Microbiol. 1993;19:1-16. |
| 3. | Cantwell MF, Snider DE Jr, Cauthen GM, Onorato IM. Epidemiology of tuberculosis in the United States, 1985 through 1992. JAMA. 1994;272:535-539. |
| 4. | Raviglione MC, Snider DE Jr, Kochi A. Global epidemiology of tuberculosis. Morbidity and mortality of a worldwide epidemic. JAMA. 1995;273:220-226. |
| 5. | Yang ZG, Min PQ, Sone S, He ZY, Liao ZY, Zhou XP, Yang GQ, Silverman PM. Tuberculosis versus lymphomas in the abdominal lymph nodes: evaluation with contrast-enhanced CT. AJR Am J Roentgenol. 1999;172:619-623. |
| 6. | Hulnick DH, Megibow AJ, Naidich DP, Hilton S, Cho KC, Balthazar EJ. Abdominal tuberculosis: CT evaluation. Radiology. 1985;157:199-204. |
| 7. | Harisinghani MG, McLoud TC, Shepard JA, Ko JP, Shroff MM, Mueller PR. Tuberculosis from head to toe. Radiographics. 2000;20:449-470; quiz 528-529, 532. |
| 8. | Griffith RC, Janney CG. Lymph nodes. Anderson's pathology, 9th ed. St. Louis: Mosby 1990; 1429-1492. |
| 9. | Dodds WJ, Foley WD, Lawson TL, Stewart ET, Taylor A. Anatomy and imaging of the lesser peritoneal sac. AJR Am J Roentgenol. 1985;144:567-575. |
| 10. | Itai Y, Moss AA, Ohtomo K. Computed tomography of cystadenoma and cystadenocarcinoma of the pancreas. Radiology. 1982;145:419-425. |
| 11. | Bowen B, Ros PR, McCarthy MJ, Olmsted WW, Hjermstad BM. Gastrointestinal teratomas: CT and US appearance with pathologic correlation. Radiology. 1987;162:431-433. |
| 12. | Da Ronch T, Modesto A, Bazzocchi M. Gastrointestinal stromal tumour: spiral computed tomography features and pathologic correlation. Radiol Med (Torino). 2006;111:661-673. |
| 13. | Pombo F, Rodriguez E, Caruncho MV, Villalva C, Crespo C. CT attenuation values and enhancing characteristics of thoracoabdominal lymphomatous adenopathies. J Comput Assist Tomogr. 1994;18:59-62. |
| 14. | Lee YY, Van Tassel P, Nauert C, North LB, Jing BS. Lymphomas of the head and neck: CT findings at initial presentation. AJR Am J Roentgenol. 1987;149:575-581. |
| 15. | Hopper KD, Diehl LF, Cole BA, Lynch JC, Meilstrup JW, McCauslin MA. The significance of necrotic mediastinal lymph nodes on CT in patients with newly diagnosed Hodgkin disease. AJR Am J Roentgenol. 1990;155:267-270. |
| 16. | Oliver TW Jr, Bernardino ME, Sones PJ Jr. Monitoring the response of lymphoma patients to therapy: correlation of abdominal CT findings with clinical course and histologic cell type. Radiology. 1983;149:219-224. |
| 17. | Xia F, Poon RT, Wang SG, Bie P, Huang XQ, Dong JH. Tuberculosis of pancreas and peripancreatic lymph nodes in immunocompetent patients: experience from China. World J Gastroenterol. 2003;9:1361-1364. |