Published online Feb 28, 2007. doi: 10.3748/wjg.v13.i8.1303
Revised: December 28, 2006
Accepted: January 8, 2007
Published online: February 28, 2007
Eosinophilic gastroenteritis is a rare gastrointestinal disorder with eosinophilic infiltration of the gastrointestinal wall and various gastrointestinal dysfunctions. Diagnosis requires a high index of suspicion and exclusion of various disorders that are associated with peripheral eosinophilia. We report a case of eosinophilic gastroenteritis, which had features of the predominant subserosal type presenting with ascites and hepatic dysfunction, and which responded to a course of low-dose steroid.
- Citation: Zhou HB, Chen JM, Du Q. Eosinophilic gastroenteritis with ascites and hepatic dysfunction. World J Gastroenterol 2007; 13(8): 1303-1305
- URL: https://www.wjgnet.com/1007-9327/full/v13/i8/1303.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i8.1303
Eosinophilic gastroenteritis, first reported by Kaijser in 1937, is a rare gastrointestinal disorder that can present with various gastrointestinal manifestations, depending on the specific site of the affected gastrointestinal wall. Klein et al[1] have demonstrated that this disorder could be pathologically classified into three major types: predominant mucosal layer, predominant muscle layer, and predominant subserosal layer. However, its clinical features, etiology, and treatment have not yet been definitely established. We report a case of eosinophilic gastroenteritis with features of the predominant subserosal type, including ascites and liver dysfunction.
In July 2006, a 33-year-old man presented with mild upper abdominal pain and, three days later, with abdominal distention, frequency of bowel motion and fever. His temperature was 38.5°C. He had no past history of ulcer pain and never had any abdominal operation. There had been no weight loss and neither blood nor mucus was present in the stool. The patient denied taking any drugs or herbal medicine. There was a history of allergy to levofloxacin. Chest examination showed no abnormality. Abdominal examination revealed a soft, mildly tender abdomen, and shifting abdominal dullness.
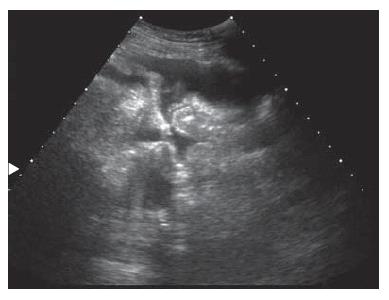
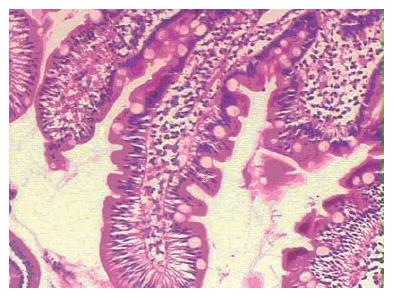
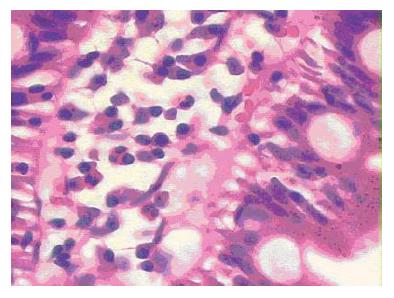
The patient was admitted to the Second Affiliated Hospital of Zhejiang University in July 2006. The hemoglobin level was 13.0 g/L( normal range, male, 11-16 g/L) and white cell count was 13.6 × 109/L, with 41.1% neutrophils, 27.9% lymphocytes, 8% monocytes and 22.5% eosinophils. The platelet count was 138 × 109/L, and the sedimentation rate was 8 mm/h. The tests for antinuclear factor, rheumatoid factor, serum hepatitis B surface antigen and serum hepatitis A, C, E antibodies gave negative results. The alanine aminotransferase level was 337 U/L (normal range, 0-50 U/L) and the aspartate aminotransferase was 223 U/L (normal range, 0-40 U/L). The anti-amoebic titer was negative and stool microscopy for ova and cysts was negative. Ultrasonography of the abdomen revealed a moderate amount of ascites (Figure 1). Gastroscopy showed mild antral gastritis. Biopsy of gastric antrum and proximal duodenum revealed inflammation with marked eosinophilic infiltration (Figure 2 and Figure 3). Colonoscopy showed mild proctitis and sigmoid colitis.
After excluding the possibilities of a malignancy, parasitic disease, and autoimmune disease, eosinophilic gastroenteritis was diagnosed. This diagnosis was supported by the presence of peripheral eosinophilia and eosinophilic infiltration of the serosa and subserosa of the gastric antrum and proximal duodenum. A small daily dose of steroid (prednisolone 20 mg) was given. Four days later, the patient recovered from his symptoms. The white cell count was 9.5 × 109/L, with 49.1% neutrophils, 27.2% lymphocytes, 7.7% monocytes and 15% eosinophils. Seven days later, the alanine aminotransferase level was 128 U/L and the aspartate aminotransferase was 38 U/L. Ultrasonography of the abdomen revealed no ascites. Steroid treatment was gradually tapered and eventually terminated after 4 wk.
The important feature in this case of eosinophilic gastroenteritis is the extremely high eosinophil count in the peripheral blood and the serosa and subserosa of the gastric antrum and proximal duodenum. The diagnosis of eosinophilic gastroenteritis was confirmed after the exclusion of other disorders that have similar features, such as gut lymphoma, parasitic infection, carcinoma, inflammatory bowel disease, and allergy.
Eosinophilic gastroenteritis is a rare disease, which was first reported by Kaijser in 1937. In 1970, Klein demonstrated that this disorder could be pathologically classified into three major types: predominant mucosal, predominant muscle layer, and predominant subserosal. The involvement of different layers usually gives rise to different clinical manifestations. Mucosal disease generally presents with bleeding, protein-losing enteropathy, or malabsorption. Involvement of the muscle layer may cause bowel wall thickening and subsequent intestinal obstruction. The subserosal form usually presents with peritonitis and eosinophilic ascites, which was the case in this patient.
Eosinophilic gastroenteritis can involve any part of the gastrointestinal tract from the esophagus down to the rectum. The stomach and duodenum, however, are the most common sites of involvement[2-5]. The etiology of eosinophilic gastroenteritis is currently unknown. Allergies to certain foods or immunological abnormalities have been speculated as its etiology[6-8]. On the other hand, some investigators[9,10]have demonstrated that the etiology of this disorder is not associated with allergic reactions. In our case, there was a past history of levofloxacin allergy. However, the patient denied taking any drugs or herbal medicine. The finding of high eosinophil count in the peripheral blood suggested allergic disorder or parasitic disorders, or abdominal lymphoma. The likelihood of parasitic disorders and abdominal lymphoma was remote because of the history of the patient’s illness, the physical findings, and the findings on gastroscopy, colonoscopy and ultrasonography.
In the mucosal form of eosinophilic gastroenteritis, multiple biopsies must be taken during endoscopy, because mucosal involvement is often patchy in nature. When there is a submucosal disease, biopsy of the mucosal layer sometimes fails to expose eosinophilic gastroenteritis. Laparotomy or laparoscopy is often required to make a diagnosis in such cases.
Treatment with a steroid is the mainstay in the management of eosinophilic gastroenteritis. Clinical improvement usually is seen after treatment with a low dose of steroid. Surgical intervention may sometimes be required for patients with complicating obstruction or when performing a full thickness intestinal biopsy to establish the diagnosis.
S- Editor Liu Y L- Editor Zhu LH E- Editor Zhou T
| 1. | Klein NC, Hargrove RL, Sleisenger MH, Jeffries GH. Eosinophilic gastroenteritis. Medicine (Baltimore). 1970;49:299-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 434] [Cited by in RCA: 407] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 2. | Liacouras CA. Eosinophilic esophagitis: treatment in 2005. Curr Opin Gastroenterol. 2006;22:147-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Straumann A, Simon HU. Eosinophilic esophagitis: escalating epidemiology? J Allergy Clin Immunol. 2005;115:418-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 285] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 4. | Repiso Ortega A, Alcántara Torres M, González de Frutos C, de Artaza Varasa T, Rodríguez Merlo R, Valle Muñoz J, Martínez Potenciano JL. Gastrointestinal anisakiasis. Study of a series of 25 patients. Gastroenterol Hepatol. 2003;26:341-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Caldwell JH. Eosinophilic Gastroenteritis. Curr Treat Options Gastroenterol. 2002;5:9-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Liacouras CA. Eosinophilic esophagitis in children and adults. J Pediatr Gastroenterol Nutr. 2003;37 Suppl 1:S23-S28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 69] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 7. | Kweon MN, Kiyono H. Eosinophilic gastroenteritis: a problem of the mucosal immune system? Curr Allergy Asthma Rep. 2003;3:79-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Cordero Miranda MA, Blandón Vijil V, Reyes Ruiz NI, Avila Castañón L, del Río Navarro BE, García Aranda JA, Blanco Rodríguez G, Sienra Monge JJ. Eosinophilic proctocolitis induced by foods. Report of a case. Rev Alerg Mex. 2002;49:196-199. [PubMed] |
| 9. | Seibold F. Food-induced immune responses as origin of bowel disease? Digestion. 2005;71:251-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Barbie DA, Mangi AA, Lauwers GY. Eosinophilic gastroenteritis associated with systemic lupus erythematosus. J Clin Gastroenterol. 2004;38:883-886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 30] [Article Influence: 1.4] [Reference Citation Analysis (0)] |