INTRODUCTION
Portal hypertension in the setting of malignancy could arise from different mechanisms: intraluminal obstruction of portal vein (either due to tumor thrombus[1-3] or as a result of deep vein thrombosis due to a paraneoplastic hypercoagulable state, extraluminal compression due to metastatic lymph nodes or tumor tissue, and acquired portal vein aneurysm[4]. Hepatocellular carcinoma and pancreatic adenocarcinoma are the commonest tumors reported in literature to present as variceal bleeding[5-10]. A case of ovarian cancer presenting similarly has been reported[11]. Gastric adenocarcinoma associated with portal venous thrombosis has been retrospectively recognized using imaging studies and post-mortem analysis[3] or encountered during the course of treatment of the primary tumor[12]. However, initial presentation as portal hypertension is rare and to our knowledge, has not been reported. We report a case of signet ring adenocarcinoma of the gastric cardia that presented as portal hypertension associated with upper gastrointestinal bleeding. The mechanism of portal hypertension was radiographically confirmed as due to a metastatic lymph node compressing the main and left portal veins.
CASE REPORT
An 80-year old man presented with 14-kg weight loss and melena for three weeks prior to hospital admission. He was pale, had bilateral pleural effusions, moderate ascites and guiac-positive melenic stool. Past medical history was significant for gastroesophageal reflux disease, systemic arterial hypertension and depression. There was no history of known liver disease or of alcohol consumption.
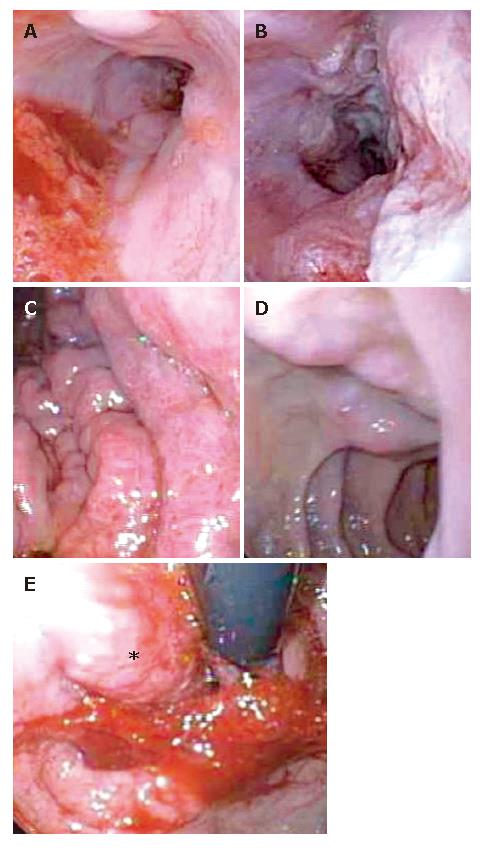
Laboratory studies confirmed the presence of normocytic anemia (hemoglobin 8.0 gm/dL), normal coagulation parameters, liver and chemistry panels. An esophagogastroduodenoscopy revealed two columns of grade 1 esophageal varices (Figure 1A and B), moderately severe portal hypertensive gastropathy (Figure 1C) and duodenal varices (Figure 1D). On retroflexed view we identified a nodular growth in the cardia of the stomach (Figure 1E, star) infiltrating into the distal esophagus (Figure 1B). Portal hypertensive gastropathy was felt to be the cause of gastrointestinal bleeding.
Figure 1 Esophagogastroduodenoscopy demonstratring grade 1 esophageal varices (A), tumor invasion of distal third of the esophagus (B), moderate portal hypertensive gastropathy (C), duodenal varices (D), retroflexed view of the nodular tumor in the gastric fundus (E).
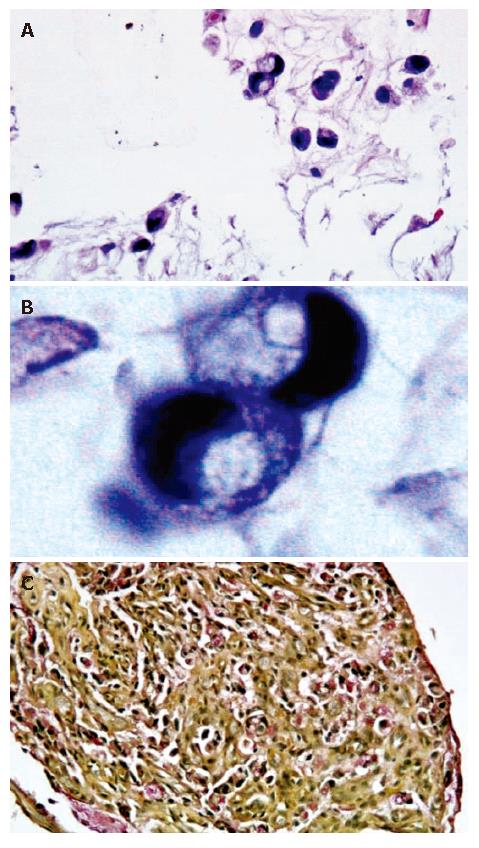
Histopathological examination of the biopsies obtained from the nodularity in the cardia revealed a poorly-differentiated infiltrative malignancy characterized by moderately-sized cells with abundant vacuolated cytoplasm, occasional signet ring cells (Figure 2A and B), nuclear pleomorphism and the presence of mitotic figures. Immunohistochemical staining for CK7 was positive in the malignant cells (not shown), while CK20 was negative. Mucicarmine stain showed cytoplasmic positivity (Figure 2C), differentiating these tumor cells from muciphages in the lamina propria.
Figure 2 Histology and immunohistochemistry of biopsies from gastric: Light microscopy with hematoxylin and eosin staining of tumor tissue at 40X and 100X with oil magnifications demonstrating moderately-sized cells with abundant vacuolated cytoplasm (A) and occasional signet ring cells (B), and mucicarmine stain demonstrating intracytoplasmic positive staining (C).
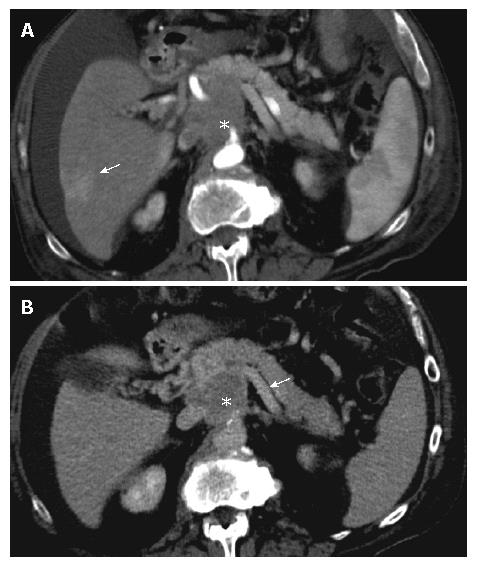
In the absence of other causes of portal hypertension, we postulated that the endoscopic appearance was best explained by portal venous obstruction. A color Doppler ultrasonography of the hepatic venous system demonstrated reversal of flow in the left portal vein with appropriate direction of flow in the right and main portal veins. The liver and hepatic arteries appeared normal. A computerized tomography of the abdomen after administration of intravenous contrast revealed a soft tissue mass (Figure 3A and B, star) measuring 5 cm in diameter displacing the pancreatic head and neck inferiorly. The superior mesenteric, splenic (Figure 3B, arrow) and main portal veins were all seen passing through this mass with severe attenuation of all three vessels. The presence of ascites and bilateral pleural effusions was confirmed by both studies.
Figure 3 Contiguous helical CT scan of the abdomen at 5 mm collimation with intravenous contrast captured in arterial phase (A) and portal venous phase (B) at the level of the pancreas.
A 5 cm soft tissue mass (star) was seen with severe attenuation of the splenic (B, arrow), main portal and superior mesenteric veins. An area of increased attenuation within the segment VI of the liver was visualized in arterial phase (A, arrow) concerning for metastasis.
Due to the advanced stage of the tumor carrying a poor prognosis in this elderly and frail patient, palliative surgery or systemic chemotherapy was considered counterproductive. He was discharged to hospice and subsequently passed away within three months from the time of diagnosis. At autopsy, metastatic disease to the segment VI of the liver was confirmed. A soft tissue mass was found encasing the spleno-portal venous system without vascular invasion or luminal thrombosis, correlating to that seen on CT image ante-mortem. Histopathologic characterization of this mass confirmed it as a lymph node metastasis from primary gastric adenocarcinoma almost replacing the entire normal architecture.
DISCUSSION
Advanced gastric cancer presenting as portal hypertension is unusual. Hepatocellular carcinoma is associated with tumor invasion of the portal and hepatic veins whereas pancreatic cancer affects the splenic vein with isolated left-sided portal hypertension. Alpha-feto protein producing hepatoid adenocarcinoma of the stomach also tends to invade the veins and metastasize to the liver[3]. In our patient serum level of alpha-feto protein was normal and not expressed within tumor cells. Gastric signet ring adenocarcinoma with metastasis to ovaries (Krukenberg tumors)[13,14], bones, meninges[15], colon, gingiva, tonsils, breasts, para-aortic lymph nodes and cervix has been reported in the literature.
Our case report not only adds to the variety of presentations of this type of cancer, but also provides an example of unusual clinical and endoscopic mimicry. The presence of esophageal and duodenal varices and absence of gastric varices suggested main portal trunk and left portal venous obstruction with effective decompression of the splenic venous system. The absence of splenomegaly, presence of an unusually enlarged inferior mesenteric vein (not shown), multiple perigastric collaterals indicated that indeed the left sided portal circulation was decompressed even though there was no obvious spleno-renal shunt. Esophageal varices usually arise due to increased pressure in the left gastric (coronary) vein that drains into the left portal vein, and less often into the main portal vein. Duodenal varices are a rare occurrence and the incidence is estimated to be 0.4% in the setting of portal hypertension[16]. The afferent vessel is usually the superior or inferior pancreaticoduodenal vein originating in the portal vein trunk or superior mesenteric vein. In our case, superior mesenteric as well as main portal veins were attenuated by encompassing metastatic mass, explaining the occurrence of esophageal and duodenal varices.
Signet ring adenocarcinoma is a rare, distinct type of gastric cancer. A retrospective analysis of this type of tumor has revealed an equal incidence in both genders: a younger age and larger tumor at presentation[17]. The histological type is commonly scirrhous and infiltrative. As in other gastric cancers, patients with early signet ring cell carcinoma have a good prognosis. However, these patients at the advanced stage have a poorer prognosis depending on the extent of vascular microinvasion and tumor location[17]. Pagetoid spread of the signet ring cells beneath the epithelial lining of gastric foveolae/glands is likely the cause of early lymphatic/vascular metastasis as in our case.