Published online Feb 14, 2007. doi: 10.3748/wjg.v13.i6.921
Revised: November 15, 2006
Accepted: December 25, 2006
Published online: February 14, 2007
AIM: To evaluate different types of treatment for sigmoid volvulus and clarify the role of endoscopic intervention versus surgery.
METHODS: A retrospective review of the clinical presentation and imaging characteristics of 33 sigmoid volvulus patients was presented, as well as their diagnosis and treatment, in combination with a literature review.
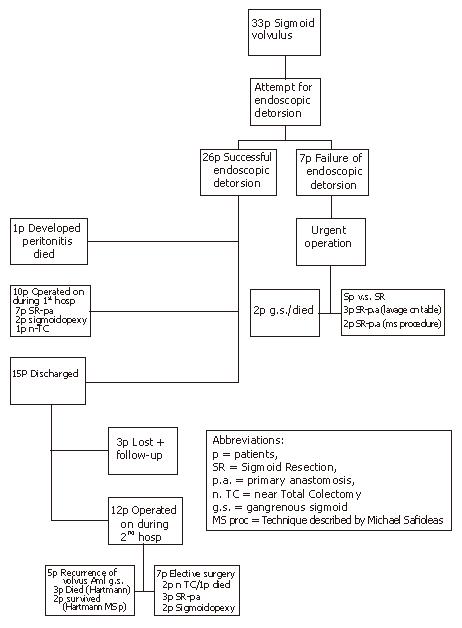
RESULTS: In 26 patients endoscopic detorsion was achieved after the first attempt and one patient died because of uncontrollable sepsis despite prompt operative treatment. Seven patients had unsuccessful endoscopic derotation and were operated on. On two patients with gangrenous sigmoid, Hartmann’s procedure was performed. In five patients with viable colon, a sigmoid resection and primary anastomosis was carried out. Three patients had a lavage “on table” prior to anastomosis, while in the remaining 2 patients a diverting stoma was performed according to the procedure of the first author. Ten patients were operated on during their first hospital stay (3 to 8 d after the deflation). All patients had viable colon; 7 patients had a sigmoid resection and primary anastomosis, 2 patients had sigmoidopexy and one patient underwent a near-total colectomy. Two patients (sigmoidectomy-sigmoidopexy) had recurrences of volvulus 43 and 28 mo after the initial surgery. Among 15 patients who were discharged from the hospital after non-operative deflation, 3 patients were lost to follow-up. Of the remaining 12 patients, 5 had a recurrence of volvulus at a time in between 23 d and 14 mo. All the five patients had been operated on and in four a gangrenous sigmoid was found. Three patients died during the 30 d postoperative course. The remaining seven patients were admitted to our department for elective surgery. In these patients, 2 subtotal colectomies, 3 sigmoid resections and 2 sigmoidopexies were carried out. One patient with subtotal colectomy died. Taken together of the results, it is evident that after 17 elective operations we had only one death (5.9%), whereas after 15 emergency operations 6 patients died, which means a mortality rate of 40%.
CONCLUSION: Although sigmoid volvulus causing intestinal obstruction is frequently successfully encountered by endoscopic decompression, however, the principal therapy of this condition is surgery. Only occasionally in patients with advanced age, lack of bowel symptoms and multiple co-morbidities might surgical repair not be considered.
- Citation: Safioleas M, Chatziconstantinou C, Felekouras E, Stamatakos M, Papaconstantinou I, Smirnis A, Safioleas P, Kostakis A. Clinical considerations and therapeutic strategy for sigmoid volvulus in the elderly: A study of 33 cases. World J Gastroenterol 2007; 13(6): 921-924
- URL: https://www.wjgnet.com/1007-9327/full/v13/i6/921.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i6.921
Although sigmoid volvulus is uncommon in Western Europe, it nevertheless constitutes the third leading cause of large bowel obstruction in adults[1]. The main predisposing factor to sigmoid volvulus is a long, redundant sigmoid colon with an elongated mesentery, which is prone to twisting on itself. Sigmoid volvulus is an abdominal emergency occurring more commonly in the elderly, particularly in individuals with dementia or a psychiatric illness[1,2] and has a high mortality rate up to 50% in each episode[3]. In elderly patients who have no signs of peritonitis or bowel gangrene an initial attempt with non-operative reduction is justified. After a successful non-operative reduction, an elective resection of the sigmoid colon is recommended as the risks of elective surgery are less compared with those associated with recurrent volvulus. We report the results of a series of 33 adult patients with a mean follow-up of 4.5 year (range 2-18 year) supporting this assumption.
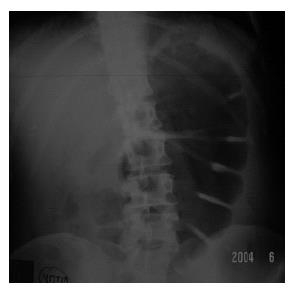
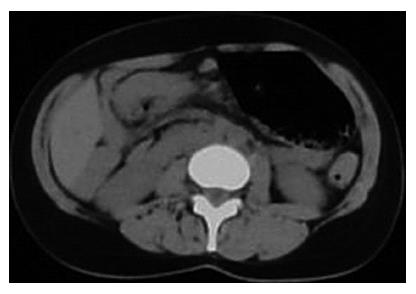
In the period of 1984-2003, 33 patients (18 males and 15 females) ranging in age between 58 and 89 year, were treated for sigmoid volvulus at the 2nd Department of Propaedeutic Surgery, Medical School, Athens University, Laiko General Hospital in Greece. The hospital records of these thirty three patients were retrospectively reviewed. All patients were admitted to our department on an emergency basis due to abdominal pain, vomiting and abdominal distention. Among these patients, 7 were institutionalized. Abdominal radiographs and CT scans were indicative of sigmoid volvulus (Figures 1 and 2), showing marked bowel dilatation and fluid levels, while the outline of twisted loop was evident.
All patients were actively resuscitated by means of nasogastric suction and correction of fluid-electrolyte imbalance, while broad-spectrum antibiotics were started immediately after admission. Subsequently, all patients, without signs of peritonitis, underwent sigmoidoscopy post bowel preparation with edema. In 26 patients detorsion was achieved after the first attempt. However, one patient developed septic peritonitis four days after detorsion and even though he was immediately operated on, he passed away.
Seven patients had unsuccessful endoscopic derotation and were operated on within 48 h after their admission. In two patients with gangrenous sigmoid, Hartmann’s procedure was performed, however, one patient died. In five patients with viable colon, sigmoid resection and primary anastomosis were carried out (Figure 3). Three patients had a lavage “on table” prior to anastomosis, while in the remaining 2 patients a diverting stoma according to the technique of the first author (MS) was used (Figure 4).
Ten patients were operated on during their first hospital stay (3 to 8 d after the deflation). All patients had viable colon; 7 patients had a sigmoid resection and primary anastomosis, 2 patients had sigmoidopexy and one patient underwent a near-total colectomy. Two patients (sigmoidectomy-sigmoidopexy) had recurrences of volvulus 43 and 28 mo after the initial surgery. Among 15 patients who were discharged from the hospital after the non-operative deflation, 3 patients were lost to follow-up. Of the remaining 12 patients, 5 had a recurrence of volvulus at a time in between 23 d and 14 mo. All the five patients had been operated on and in four a gangrenous sigmoid was found. Three patients died during the 30 d postoperative course. The remaining seven patients were admitted to our department for elective surgery. In these patients, 2 subtotal colectomies, 3 sigmoid resections and 2 sigmoidopexies were carried out. One patient with subtotal colectomy died. Taken together of the results, it is evident that after 17 elective operations we had only one death (mortality rate: 5.9%), whereas after 15 emergency operations 6 patients died (mortality rate: 40%). In Figure 5 the course of 33 patients is schematically depicted.
Sigmoid volvulus is the most common cause of strangulation of the colon and is also the cause for 1% to 7% of all intestinal obstructions in Western countries[4]. Many patients with sigmoid volvulus have clinical findings indicating a disorder of bowel movement[5,6], such as constipation and abdominal distention long before the development of a sigmoid volvulus. Some researchers have claimed that sigmoid volvulus might be one of the disorders allied with Hirschsprung’s disease[7]. It is also a fact that patients undergoing sigmoidectomy for sigmoid volvulus frequently suffer from elongation and dilatation of the remaining colon and some even require surgery for revolvulus[8]. The disease is rare in children[9]; however, if it occurs, it may result in acute intestinal obstruction, unlike in adults where the obstruction may be subacute and progressive[10]. In our series 19 patients had a history of undetermined abdominal pain during the period of 3 to 9 mo. Moreover, besides chronic constipation and despite the use of laxatives[2,11], other risk factors that predispose to sigmoid volvulus are considered as follows: (1) a course with high fiber diet, (2) pregnancy, (3) pelvic tumors or cysts, (4) previous abdominal surgery. Concerning the last factor, the presence of a band attaching the sigmoid colon to the abdominal wall can act as an axis for volvulus. Furthermore, it is supposed that the loss of ganglion cells is only a consequence, not a cause, since the exact cause leading to sigmoid volvulus is not clear[12].
All these conditions may produce a large, redundant sigmoid colon, in association with mesocolon, long and narrow at its parietal attachment, resulting in the two ends of the loop being close together, under which condition, the bowel is capable of becoming torted around its central mesenteric axis.
Although sigmoid volvulus has been well studied for many decades, its treatment appears to be still evolving[3]; however, over the past two decades, resection and primary anastomosis has emerged as the preferable treatment for this disease[13]. Whether endoscopic deflation is feasible to perform prior to surgery is an optimal choice. Unfortunately endoscopic detorsion is not always successful. In Western countries a 30% failure has been reported[14-16].
In our department, since 1995, we have always followed such a strategy. Initially, we attempt an endoscopic deflation and if it is unsuccessful we proceed to an emergency operation; while if detorsion has been achieved the operation is performed after 3 to 8 d by a semi-elective or elective way. In the majority of cases resection of the involved sigmoid colon is carried out, in which case primary anastomosis is the goal, either after “on table” lavage, or applying a diverting stroma[17].
In the presence of megacolon, a near-total colectomy is required. Furthermore, various procedures have been adopted for sigmoid volvulus in adult patients, such as mesosigmoidoplasty, sigmoidopexy, tube sigmoid colostomy or mesocoloplasty. In patients with sigmoid resection a recurrence is possible in approximately 25% to 35% cases[5,13,18]. The mortality rate ranges from 1% to 9% for viable colon[15,19], and 25% for gangrenous volvulus[15]. Colonic resection for non-gangrenous sigmoid volvulus has an acceptably low rate of complications, particularly when it is done as a semi-elective procedure, i.e., subsequent to endoscopic detorsion and deflation[20]. Finally, recurrent volvulus after resection has been reported at an incidence rate ranging from 24% to 33% of cases[5,18].
In conclusion, even though sigmoid volvulus causing intestinal obstruction is frequently encountered in endoscopic decompression, this condition should be definitely treated by surgery; and only occasionally in patients with advanced age, lack of bowel symptoms, having multiple co-morbidities might surgical repair not be considered.
S- Editor Liu Y L- Editor Zhu LH E- Editor Lu W
| 1. | Grossmann EM, Longo WE, Stratton MD, Virgo KS, Johnson FE. Sigmoid volvulus in Department of Veterans Affairs Medical Centers. Dis Colon Rectum. 2000;43:414-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 66] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 2. | Dülger M, Cantürk NZ, Utkan NZ, Gonullu NN. Management of sigmoid colon volvulus. Hepatogastroenterology. 2000;47:1280-1283. [PubMed] |
| 3. | Madiba TE, Thomson SR. The management of sigmoid volvulus. J R Coll Surg Edinb. 2000;45:74-80. [PubMed] |
| 5. | Morrissey TB, Deitch EA. Recurrence of sigmoid volvulus after surgical intervention. Am Surg. 1994;60:329-331. [PubMed] |
| 6. | Strom PR, Stone HH, Fabian TC. Colonic atony in association with sigmoid volvulus: its role in recurrence of obstructive symptoms. South Med J. 1982;75:933-936. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Tomita R, Ikeda T, Fujisaki S, Tanjoh K, Munakata K. Hirschsprung's disease and its allied disorders in adults' histological and clinical studies. Hepatogastroenterology. 2003;50:1050-1053. [PubMed] |
| 8. | Furuya Y, Yasuhara H, Yanagie H, Naka S, Takenoue T, Shinkawa H, Niwa H, Kikuchi T, Nagao T. Role of ganglion cells in sigmoid volvulus. World J Surg. 2005;29:88-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Campbell JR, Blank E. Sigmoid volvulus in children. Pediatrics. 1974;53:702-705. [PubMed] |
| 10. | Hinshaw DB, CARTER R. Surgical management of acute volvulus of the sigmoid colon; a study of 55 cases. Ann Surg. 1957;146:52-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 47] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Khanna AK, Kumar P, Khanna R. Sigmoid volvulus: study from a north Indian hospital. Dis Colon Rectum. 1999;42:1081-1084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 30] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Collure DW, Hameer HR. Loss of ganglion cells and marked attenuation of bowel wall in cecal dilatation. J Surg Res. 1996;60:385-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Ballantyne GH. Review of sigmoid volvulus: history and results of treatment. Dis Colon Rectum. 1982;25:494-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 70] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Sinha RS. A clinical appraisal of volvulus of the pelvic colon with special reference to aetiology and treatment. Br J Surg. 1969;56:838-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Mishra SB, Sahoo KP. Primary resection and anastomosis for volvulus of sigmoid colon. J Indian Med Assoc. 1986;84:265-268. [PubMed] |
| 16. | Faranisi CT. An approach to the management of volvulus of the sigmoid colon. Cent Afr J Med. 1990;36:31-33. [PubMed] |
| 17. | Safioleas MC, Moulakakis KG, Stamatakos MK. A new therapeutic surgical method in patients with left-sided colonic emergencies. Int J Colorectal Dis. 2006;21:186-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Chung YF, Eu KW, Nyam DC, Leong AF, Ho YH, Seow-Choen F. Minimizing recurrence after sigmoid volvulus. Br J Surg. 1999;86:231-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 51] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Degiannis E, Levy RD, Sliwa K, Hale MJ, Saadia R. Volvulus of the sigmoid colon at Baragwanath Hospital. S Afr J Surg. 1996;34:25-28. [PubMed] |