Published online Dec 21, 2007. doi: 10.3748/wjg.v13.i47.6444
Revised: October 10, 2007
Accepted: November 17, 2007
Published online: December 21, 2007
Eosinophilic enteritis, a relatively rare entity, usually involves gastric antrum or proximal small bowel. Our case is rarer in its involvement of the distal small bowel and presents unusually as intussusception. The disease if diagnosed in the initial stages responds well to medical treatment but if associated with complications or misdiagnosed, surgical modality is the treatment of choice. In our case, the patient presented with acute intestinal obstruction due to intussusception and emergency laparotomy with ileoileal anastomosis was done. Histopathology confirmed the diagnosis as eosinophilic enteritis. This case with such a presentation is discussed here.
- Citation: Kshirsagar AY, Jagtap SV, Kanojiya RP, Langade YB, Shinde SL, Shekhar N. Eosinophilic enteritis presenting as a rare cause for ileo-ileal intussusception. World J Gastroenterol 2007; 13(47): 6444-6445
- URL: https://www.wjgnet.com/1007-9327/full/v13/i47/6444.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i47.6444
Eosinophilic enteritis is a rare, poorly understood condition presenting with a bizarre spectrum of unexplained symptoms mimicking any other acute abdominal conditions. Diagnosis initially is based on exclusion of other abdominal conditions though ultimately histopathology is definitive. The majority of patients respond to medical treatment but if associated with complications like obstruction, perforation, intussusception etc., surgical intervention is necessary. We present a case of eosinophilic enteritis of the distal ileum with intussusception.
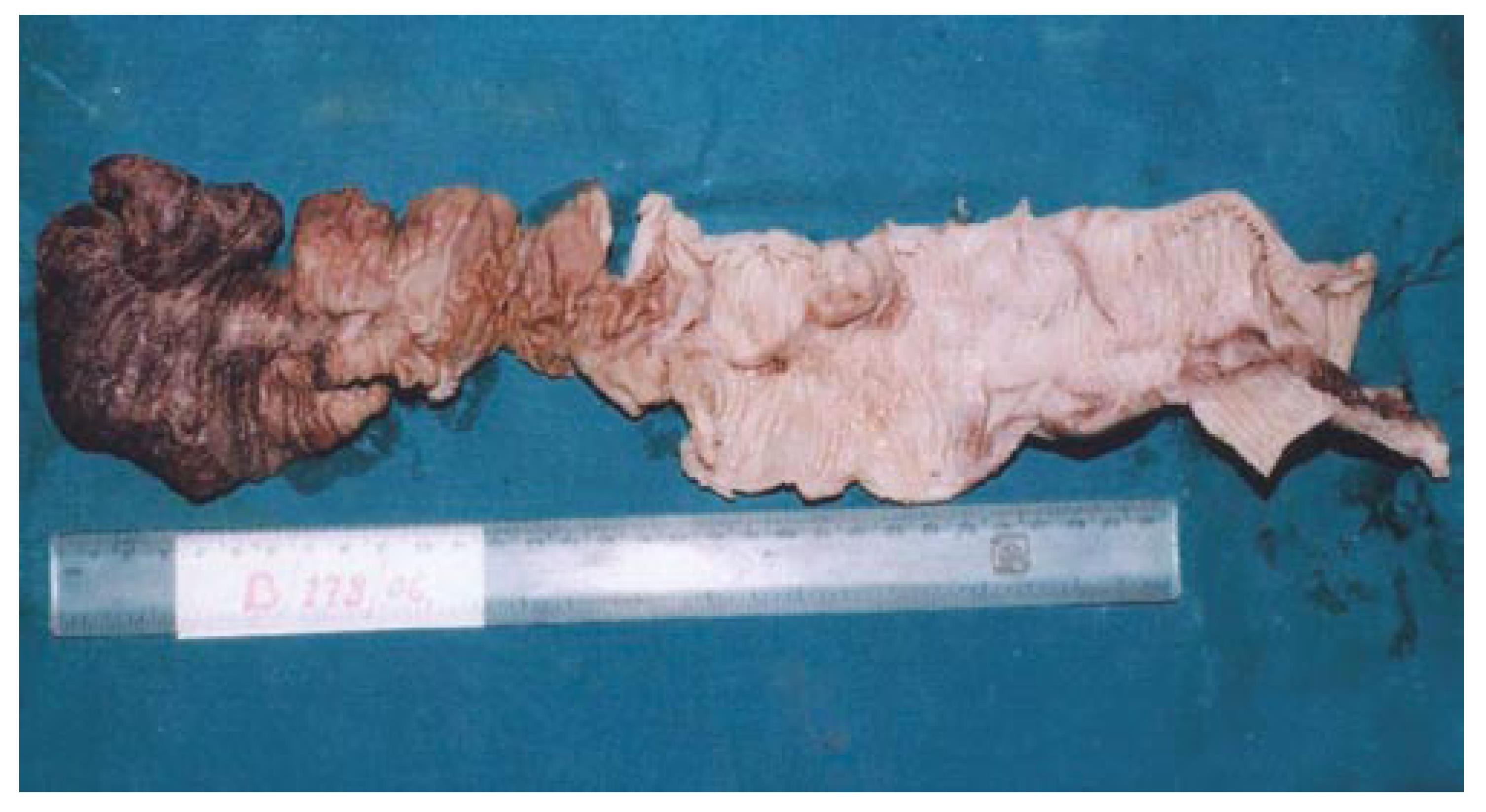
A 40-year-old man was admitted to the emergency department of our hospital for severe colicky upper abdominal pain and vomiting. He had a history of mild colicky abdominal pain a month ago but no history of food sensitization, allergic disease, asthma, parasitic infestations or any abdominal surgery. Physical examination revealed generalized distention with tenderness all over the abdomen. Per rectal examination was unremarkable. Blood investigations revealed 117 g/L hemoglobin, 8700/mm3 white blood cells with 67% neutrophils, 36% lymphocytes and 3% eosinophils. The rest of haematological investigations were within normal limits. Abdominal radiograph revealed multiple air-fluid levels suggestive of small bowel obstruction. Ultrasonography revealed intussusception of the distal small bowel. Emergency laparotomy revealed ileo-ileal intussusception with gangrenous changes, about 15 cm proximal to the ileo-caecal junction. Resection with ileo-ileal anastomosis was done.
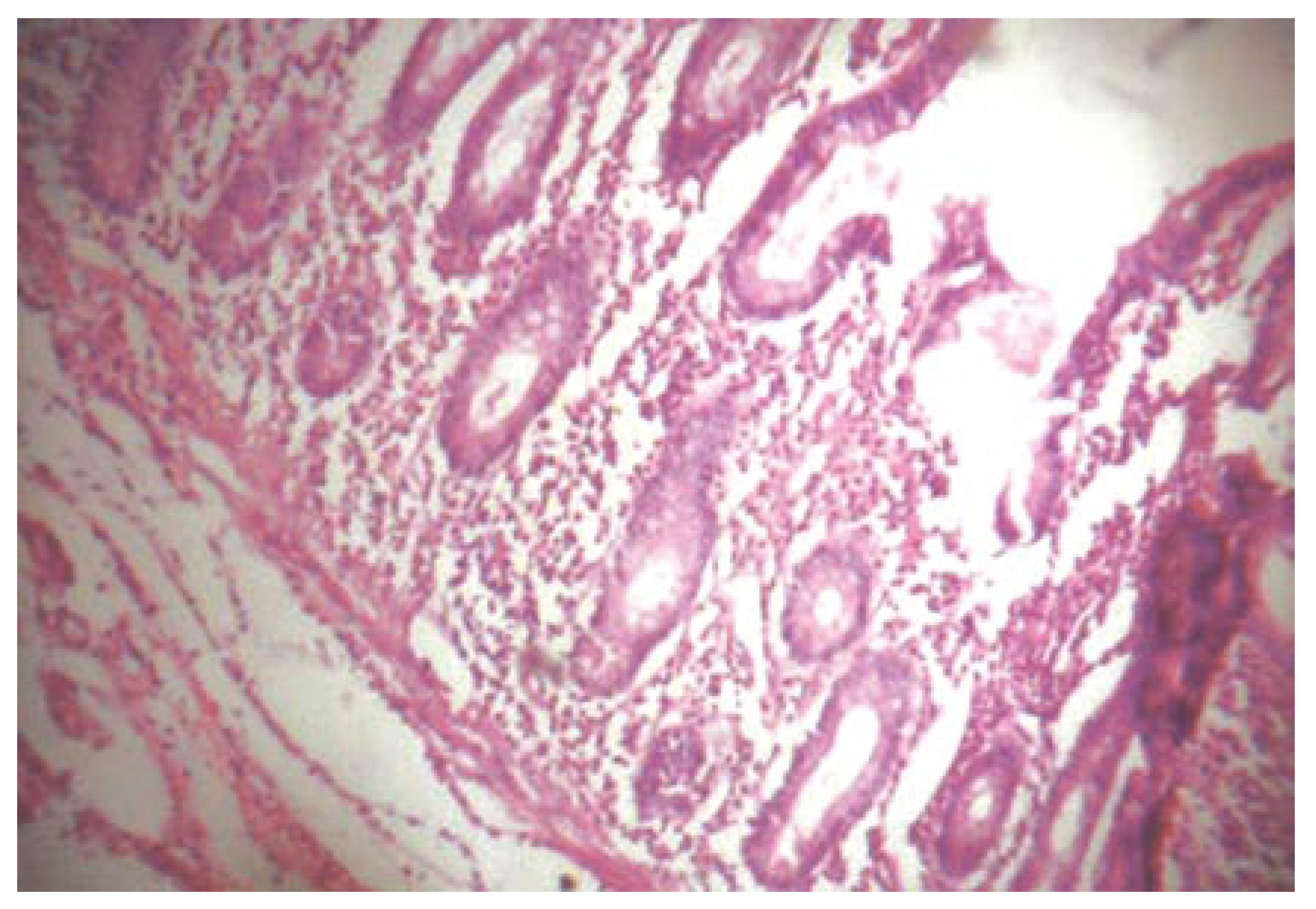
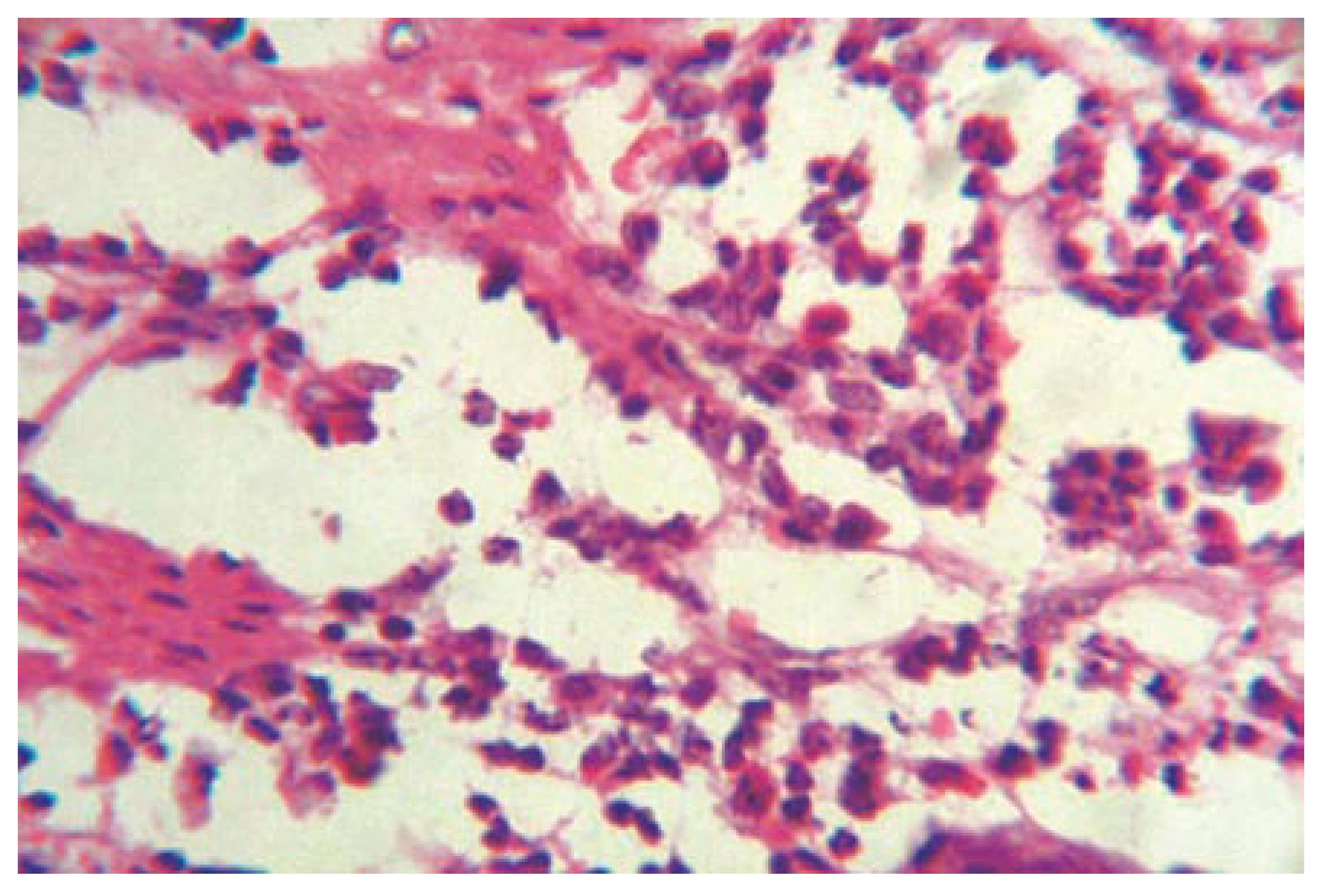
Histopathology revealed the surrounding mucosa and submucosa. Muscular layers were heavily infiltrated by eosinophils (50-60/Hpf) along with polymorphonuclear cells, lymphocytes and few plasma cells. Intestinal wall was thickened with areas of necrosis suggestive of eosinophilic enteritis with gangrene. No evidence of malignancy was found. The patient was asymptomatic, his follow-up serum immunoglobulin E levels were within normal limits, and repeated peripheral smears did not show eosinophilia (Figures 1, 2 and 3).
Eosinophilic gastroenteritis is one of the rare conditions and its etiology is poorly understood. It usually involves the gastric antrum and proximal small bowel, but rarely involves the distal gut. In about 85% of cases it is associated with eosinophilia. Classification of eosinophilic enteritis is based upon the presence of eosinophilia or eosinopenia[1]. Clinical features depend upon the most prominent layer of visceral wall involvement by eosinophils, i.e., mucosal, muscular or serosal[2-6]. Involvement of muscularis results in obstructive symptoms and serosal involvement produces ascites. Evaluation of immunoglobulin E levels may help to detect an allergic cause. Despite all clinical factors, definitive diagnosis can only be made by histopathology confirming eosinophilic involvement of the affected area. In cases of intussusception, malignancy should always be ruled out[7].
At present, laparoscopic full thickness biopsy can be definitive in suspected cases[8]. Corticosteroid therapy is the mainstay of medical treatment. Long term follow-up is required as there are always chances of recurrence[9].
The authors thank Dr. HR Tata, Head of the Department of Surgery and Medical Director, for allowing us to publish the data and Mrs. MC Deshingkar for her secretariat support in preparing this paper.
S- Editor Ma N L- Editor Wang XL E- Editor Liu Y
| 1. | O'Neill T. Eosinophilic granuloma of the gastro-intestinal tract. Case report and suggested classification. Br J Surg. 1970;57:704-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Lee CM, Changchien CS, Chen PC, Lin DY, Sheen IS, Wang CS, Tai DI, Sheen-Chen SM, Chen WJ, Wu CS. Eosinophilic gastroenteritis: 10 years experience. Am J Gastroenterol. 1993;88:70-74. [PubMed] |
| 3. | Talley NJ, Shorter RG, Phillips SF, Zinsmeister AR. Eosinophilic gastroenteritis: a clinicopathological study of patients with disease of the mucosa, muscle layer, and subserosal tissues. Gut. 1990;31:54-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 506] [Cited by in RCA: 514] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 4. | Lee M, Hodges WG, Huggins TL, Lee EL. Eosinophilic gastroenteritis. South Med J. 1996;89:189-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 47] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Klein NC, Hargrove RL, Sleisenger MH, Jeffries GH. Eosinophilic gastroenteritis. Medicine (Baltimore). 1970;49:299-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 434] [Cited by in RCA: 407] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 6. | Kraft SC, Kirsner JB. Immunology in gastroenterology. 4th ed. Philadelphia: WB Saunders 1985; 4487-4524. |
| 7. | Corman ML. Carcinoma of colon. 3rd ed. Philadelphia: JB Lippincott Co 1993; 487-595. |
| 8. | Edelman DS. Eosinophilic enteritis. A case for diagnostic laparoscopy. Surg Endosc. 1998;12:987-989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Naylor AR. Eosinophilic gastroenteritis. Scott Med J. 1990;35:163-165. [PubMed] |