Published online Nov 28, 2007. doi: 10.3748/wjg.v13.i44.5954
Revised: August 31, 2007
Accepted: October 23, 2007
Published online: November 28, 2007
To date, antegrade intussusception involving a Roux-en-Y reconstruction has been reported only once. We report a case of acute bowel obstruction due to an intussusception involving two Roux-en-Y limbs in a 40-year-old woman with a history of chronic pancreatitis due to pancreas divisum. Four years preceding this event, the patient had undergone a Whipple procedure, and three years prior to that, a Puestow operation. The patient was successfully treated with bowel resection and a side-to-side anastomosis between the most distal aspect of the bowel and the most distal Roux-en-Y reconstruction, which preserved both Roux-en-Y reconstructions.
- Citation: Gigena M, Villar HV, Knowles NG, Cunningham JT, Outwater EK, Leon Jr LR. Antegrade bowel intussusception after remote Whipple and Puestow procedures for treatment of pancreas divisum. World J Gastroenterol 2007; 13(44): 5954-5956
- URL: https://www.wjgnet.com/1007-9327/full/v13/i44/5954.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i44.5954
It is a well known fact that intussusception is most often seen in children[1]. Intussusception in adults however is relatively rare, with about 17% of intussusception cases in large reported series having occurred in adults[1]. Surgical sutures or staples along an anastomosis are, among other factors, well-known lead points for the development of intussusception, therefore making abdominal surgical interventions recognized risk factors for the occurrence of this complication[2-6]. Intestinal tract reconstructive surgery involving the pancreas however, has been very rarely linked to the development of intussusception[7]. We report the case of a middle-aged woman who developed intussusception after two major operations that were remotely performed for the therapy of symptomatic pancreas divisum. A brief discussion of the available literature is also presented.
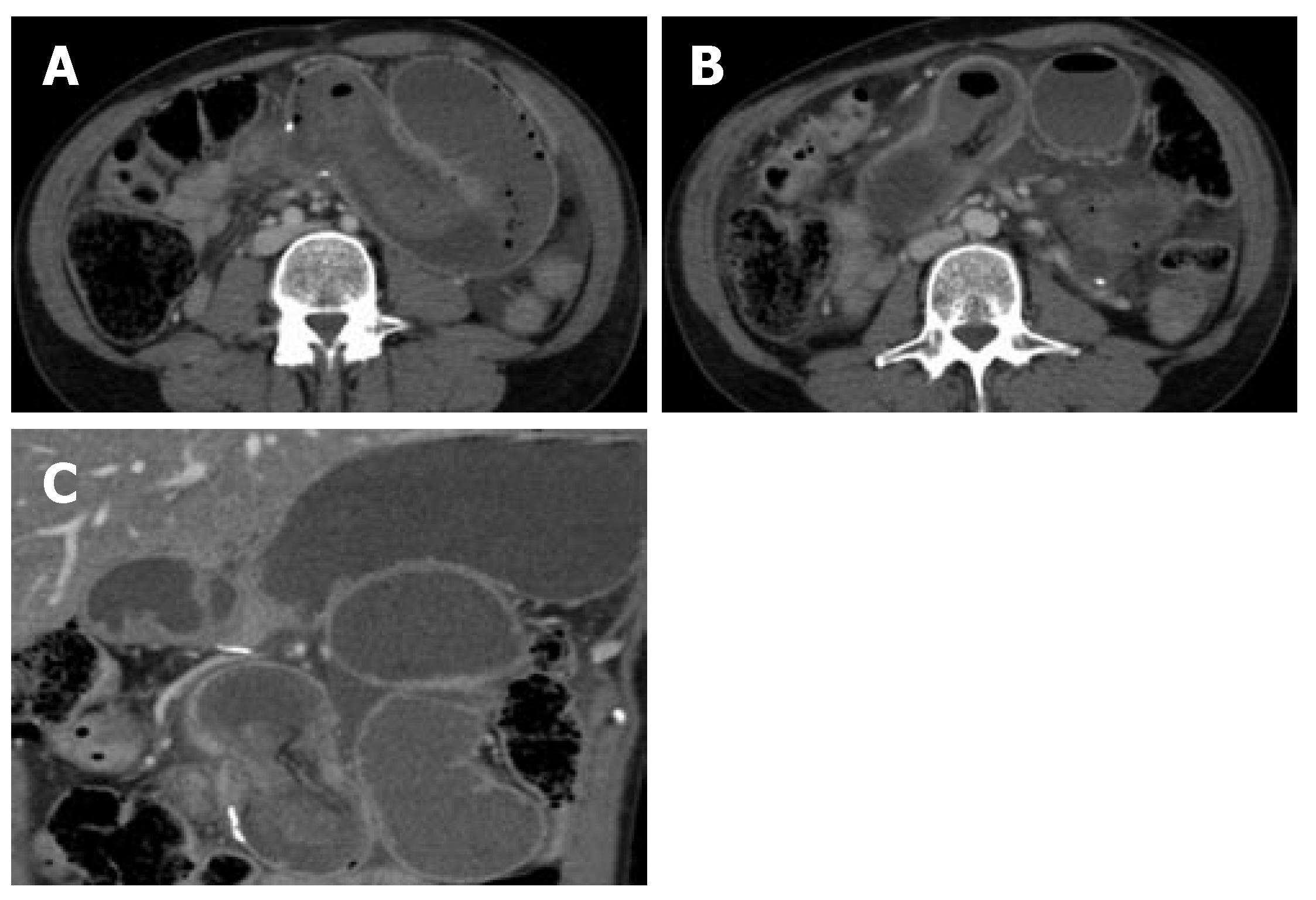
A 40-year-old woman presented with abdominal pain, nausea and vomiting of 24 h duration. She was afebrile and normotensive but had tachycardia. Her upper abdomen was visibly distended and a palpable epigastric mass could be felt. The abdomen was severely tender to palpation and peritoneal signs were elicited. Her past history was significant for pancreas divisum and chronic pancreatitis. Four years prior, she underwent a Whipple procedure as therapy for her pancreatic abnormalities. This required surgical revision 1 year later with a Puestow operation, due to stricture of the previously performed pancreatico-intestinal anastomosis. Ever since, she experienced intermittent abdominal pain, for which she was prescribed strong analgesics, with only partial symptomatic relief. Her white blood cell count was 17000 cells/mm3. A computed tomography (CT) scan of the abdomen was obtained, which demonstrated jejunal intussusception, with findings suggesting bowel ischemia (Figure 1).
After fluid resuscitation, the patient was subjected to an exploratory laparotomy. A small amount of ascites was encountered. Two loops of dilated small bowel were found inferior to the transverse mesocolon, each measuring about 10 cm in maximal diameter. These loops were identified to be part of the previously performed Roux-en-Y and Puestow procedures, going towards the stomach, bile duct and the pancreatico-jejunostomy reconstruction. Upon further exploration, an intussusception just distal to the most distal Roux-en-Y connection was found, and about 30 cm of non-perforated necrotic small bowel was identified. The intussusception occurred in an antegrade fashion, which obstructed both Roux-en-Y reconstructions. With care, the intussuscepted intestine was reduced. The necrotic bowel was then resected, and a side-to-side anastomosis between the most distal aspect of the bowel and the Roux-en-Y reconstruction that was directed towards the Puestow procedure was performed.
Due to the massive mesenteric vascular engorgement caused by the intussusception, there was an area of bleeding emanating from a bowel mesentery tear. This was localized and controlled. The abdomen was lavaged and closed. Postoperatively, the patient developed clinical evidence of abdominal compartment syndrome and required emergent re-exploration and blood transfusion. The mesenteric tear was again found to be the source of massive bleeding, and was repaired with additional stitches. Temporary skin closure of the abdomen was performed. Final closure was performed 3 d after the first intervention, and she was discharged without complications 8 d later.
Pancreas divisum is an anomaly of the pancreatic ducts, which represents the most common congenital variant of the pancreas. It results from the absence of embryological fusion of the dorsal and ventral pancreatic ducts, each keeping their drainage autonomy[8]. The correlation of this abnormality with pancreatic disease is very controversial[9]. Several techniques have been suggested for therapy, including endoscopic papillotomy, open surgical accessory sphincteroplasty, or a Puestow procedure[10]. As a result of the underlying duct anomalies and significant pancreatic head changes, some have suggested treatment with duodenum-preserving pancreatic head resection (Beger's pancreatectomy)[10]. With good patient selection, the outcome of surgical therapy has been shown to be acceptable.
Our patient underwent a Whipple procedure for chronic pancreatitis, which did not achieve symptomatic relief. This was likely due to stenotic involvement of the entire pancreatic duct, and not only the head portion, as well as due to a stricture at the pancreatico-intestinal anastomosis. This was recorded in the patient’s old medical records. In consequence, a Puestow operation was subsequently performed, which resulted in symptomatic improvement but incomplete relief. The latter procedure would have likely been a better first modality of therapy for this patient upon her initial presentation, together with a papillotomy of the minor papilla. However, endoscopic retrograde cholangiopancreatography images were not available to us, and it is therefore impossible to give an accurate opinion about her initial treatment.
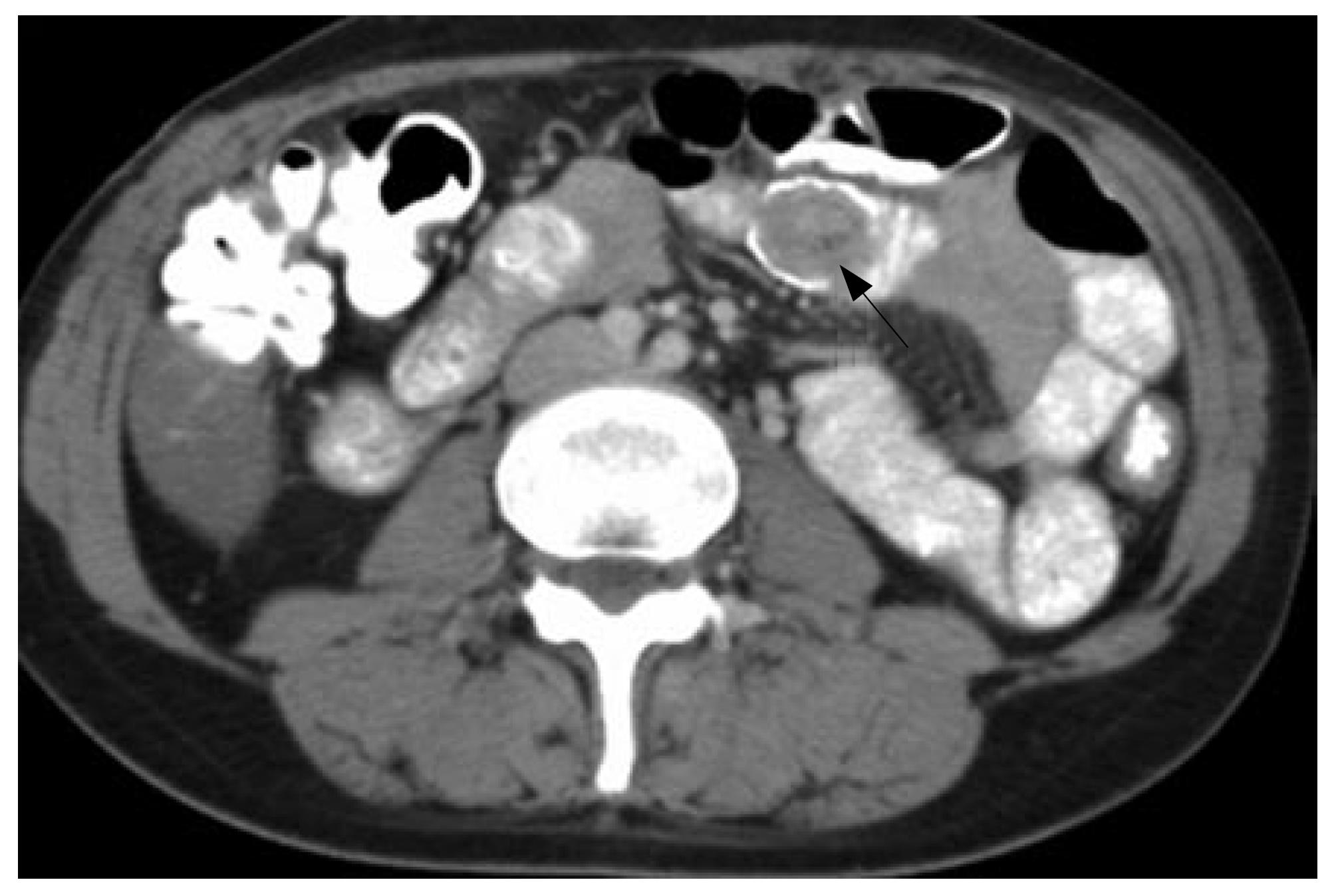
The chronic nature of our patient’s symptoms made her diagnosis challenging. This was due to the fact that she had recurrent symptoms of abdominal pain, nausea and vomiting after both interventions, and that she required large doses of analgesics and antidepressants due to chronic pain. In fact, previously performed CT scans revealed milder degrees of small bowel intussusception in prior hospital visits (Figure 2), which were thought to represent transient short bowel segment intussusceptions.
It has been suggested that altered intestinal motility may contribute to the development of intussusception[2]. In fact, this complication may be an extreme form of the so-called Roux-en-Y stasis syndrome[3]. It has been shown that the myoelectric activity of the Roux limb is often dysfunctional, split and retrograde, and of high amplitude (> 120 mmHg). Therefore it is possible that the intussusception seen in our patient was the result of severe disruption of the normal pacemaker activity in the intestines[3]. This is even more likely given the fact that we did not identify any intraluminal, extraluminal or intramural lesions. Her current presentation with necrotic bowel did not allow us to perform further imaging studies (i.e., small bowel follow through or gastric emptying studies) to demonstrate altered motility and peristaltic motion, and, rather, mandated emergent exploration.
Cases of small bowel intussusception in adults without a lead point have rarely been reported. They are most often seen after gastric bypass is performed for morbid obesity[4,5], but also have been reported exceptionally after biliary reconstruction for choledochal cysts[6], or associated with Vibrio infection in a patient with diabetic ketoacidosis[11]. Intussusception occurring after pancreatic duct reconstruction is extremely rare. It was reported for the first time after a pancreatico-jejunostomy in 2003[7]. The latter case reported retrograde intussusception of the efferent limb into the anastomosis of a revised Roux-en-Y bypass of the pancreas, similar to our case. Our patient represents the second reported case of an antegrade intussusception that occurred after pancreatic reconstruction. The retrograde case that was reported by Whipple and colleagues[7], occurred after a Roux-en-Y revision for an antegrade intussusception after a Puestow procedure performed for chronic pancreatitis.
A lead point is identified in approximately 80% of intussusception cases[7]. In the current case, we were not able to identify a lead point. Interestingly, neither was this noted in the case reported by Whipple et al[7].
Our patient unfortunately developed abdominal compartment syndrome due to massive hemoperitoneum. The massive intestinal dilatation accounted for the friability of the bowel mesentery, which, together with an elevated venous pressure caused by blood flow obstruction in the caval-mesenteric veins, due to the mass effect produced by the bowel obstruction, may explain the large amount of bleeding. Permanent abdominal closure after our second intervention was precluded because of bowel edema and disseminated intravascular coagulation after massive resuscitation, due to the large amount of blood loss.
In conclusion, antegrade intussusception in adults after pancreatic duct reconstruction is extremely rare. Our case represents the second report in the literature of such an occurrence. This patient had previous episodes of abdominal pain, nausea and vomiting, which suggests that altered intestinal motility may have contributed to her current presentation. Bowel intussusception should be always considered in cases of small bowel obstruction in adults after pancreatic reconstruction.
S- Editor Liu Y L- Editor Kerr C E- Editor Yin DH
| 1. | Agha FP. Intussusception in adults. AJR Am J Roentgenol. 1986;146:527-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 168] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 2. | Hocking MP, McCoy DM, Vogel SB, Kaude JV, Sninsky CA. Antiperistaltic and isoperistaltic intussusception associated with abnormal motility after Roux-en-Y gastric bypass: a case report. Surgery. 1991;110:109-112. [PubMed] |
| 3. | Gerst PH, Iyer S, Murthy RM, Albu E. Retrograde intussusception as a complication of Roux-en-Y anastomosis. Surgery. 1991;110:917-919. [PubMed] |
| 4. | Edwards MA, Grinbaum R, Ellsmere J, Jones DB, Schneider BE. Intussusception after Roux-en-Y gastric bypass for morbid obesity: case report and literature review of rare complication. Surg Obes Relat Dis. 2006;2:483-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 44] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Ver Steeg K. Retrograde intussusception following Roux-en-Y gastric bypass. Obes Surg. 2006;16:1101-1103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Li M, Jin Q, Feng J. Early postoperative complications of choledochal cyst excision and reconstruction of biliary tract. Zhonghua WaiKe ZaZhi. 2001;39:686-689. [PubMed] |
| 7. | Whipple OC, Stringer EF, Senkowski CK, Hartley M. Retrograde intussusception of the efferent limb after a pancreaticojejunostomy. Am Surg. 2003;69:353-355. [PubMed] |
| 8. | Mulholland MW, Moosa AR, Liddle RA. Pancreas: anatomy and structural anomalies. Textbook of Gastroenterology. Philadelphia, PA: JB Lippin8473-1-Bcott; 1995; . |
| 9. | Spicak J, Poulova P, Plucnarova J, Rehor M, Filipova H, Hucl T. Pancreas divisum does not modify the natural course of chronic pancreatitis. J Gastroenterol. 2007;42:135-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Varshney S, Johnson CD. Surgery for pancreas divisum. Ann R Coll Surg Engl. 2002;84:166-169. [PubMed] |
| 11. | Koh JS, Hahm JR, Jung JH, Jung TS, Rhyu SS, Moon SW, Kang MY, Ahn YJ, Kim SJ, Chung SI. Intussusception in a young female with Vibrio gastroenteritis and diabetic ketoacidosis. Intern Med. 2007;46:171-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |