Published online Oct 28, 2007. doi: 10.3748/wjg.v13.i40.5400
Revised: August 14, 2007
Accepted: August 29, 2007
Published online: October 28, 2007
We present a female patient with sigmoid colon endome-triosis who was diagnosed correctly preoperatively and underwent minimally invasive surgery. She was admitted to our hospital with rectal bleeding and constipation. We performed several workups. Colonoscopy and endoscopic ultrasonography showed sigmoid colon stenosis caused by submucosal tumor, and magnetic resonance imaging revealed a sigmoid colon tumor displaying signal hy-pointensity on both T1- and T2-weighted imaging. However, colonoscopic ultrasonography-assisted needle aspiration biopsy could not specify tumor characteristics. From these examinations, the lesion was diagnosed as sigmoid colon endometriosis and laparoscopy-assisted sigmoidectomy was performed. Pathological diagnosis from the resected specimen was identical to preoperative diagnosis, i.e., colonic endometriosis. Since differential diagnosis of intestinal endometriosis seems difficult, a cautious preoperative diagnosis is required to select treatments including minimally invasive surgery.
- Citation: Yoshida M, Watanabe Y, Horiuchi A, Yamamoto Y, Sugishita H, Kawachi K. Sigmoid colon endometriosis treated with laparoscopy-assisted sigmoidectomy: Significance of preoperative diagnosis. World J Gastroenterol 2007; 13(40): 5400-5402
- URL: https://www.wjgnet.com/1007-9327/full/v13/i40/5400.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i40.5400
Endometriosis is a common benign disease among women of reproductive age, and affects the intestinal tract in 15%-37% of all patients with pelvic endometriosis[1]. The disease is thus comparatively common, but preoperative diagnosis is reportedly difficult[2-4]. Herein, we report a case of sigmoid colon endometriosis that was diagnosed preoperatively using magnetic resonance imaging (MRI) and then treated by minimally invasive surgery.
A 43-year-old woman was admitted to our hospital with chronic constipation and decreased stool caliber for 3 mo before admission. Rectal bleeding was also reported, but was not associated with her menstrual cycle. She did not have any other symptoms, including abdominal pain. She was 14-years-old at first menstruation and her cycle was irregular at every 27-50 d, lasting 7-12 d. The patient was nulliparous and had not had an abortion.
Physical examination revealed no specific findings, including abdominal pain or palpable masses in the abdomen.
Laboratory examination showed an elevation of cancer antigen (CA) 125 level to 90.5 IU/mL, but other values were within normal limits.
Gynecological examination revealed a normal vagina, uterus and uterine cervix. Transvaginal ultrasonography revealed multiple myomas with diameters of 1-2 cm in the uterine wall, but no abnormality in either ovary.
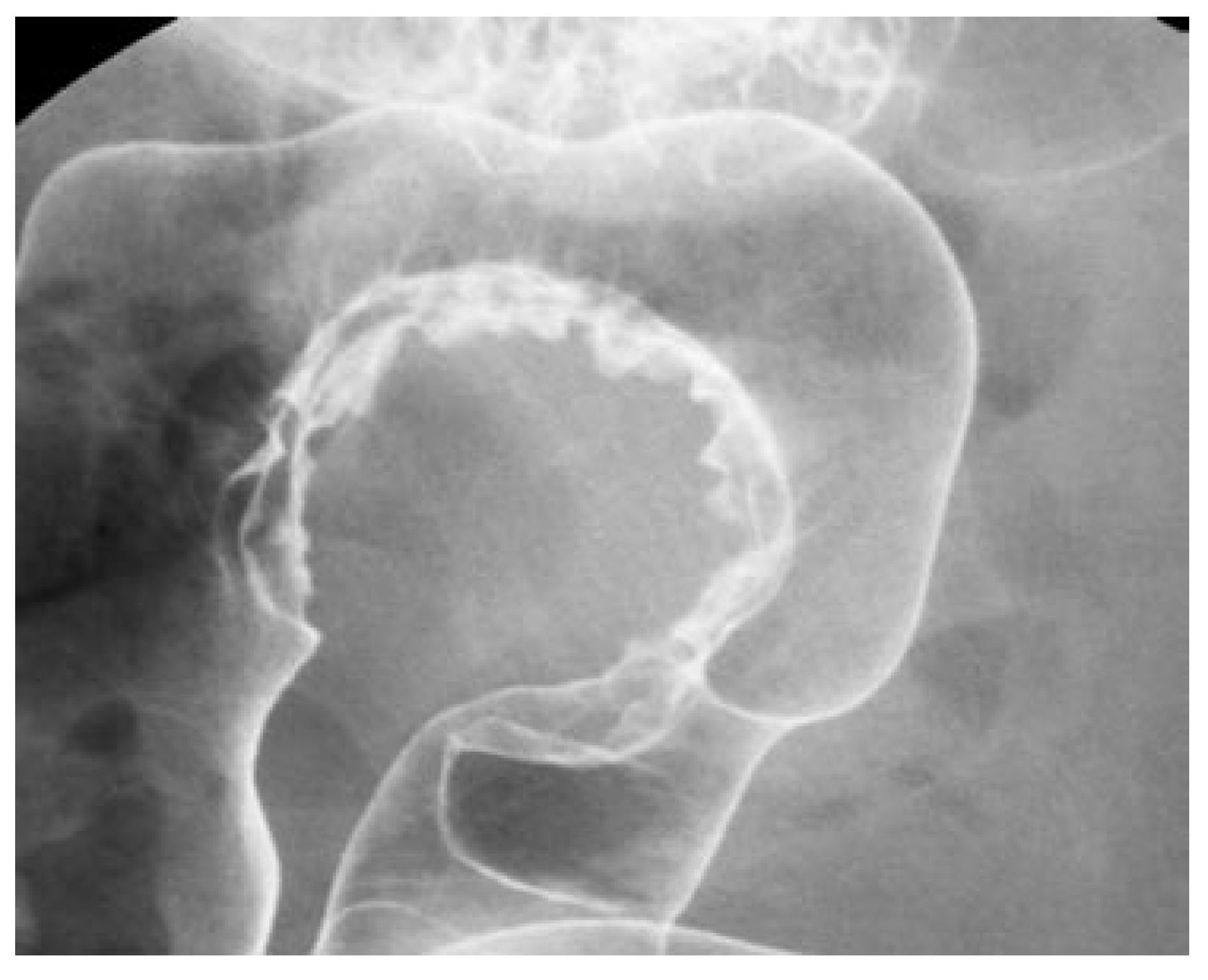
Barium enema showed stenosis of the sigmoid colon caused by tumor, but the mucous membrane was smooth (Figure 1).
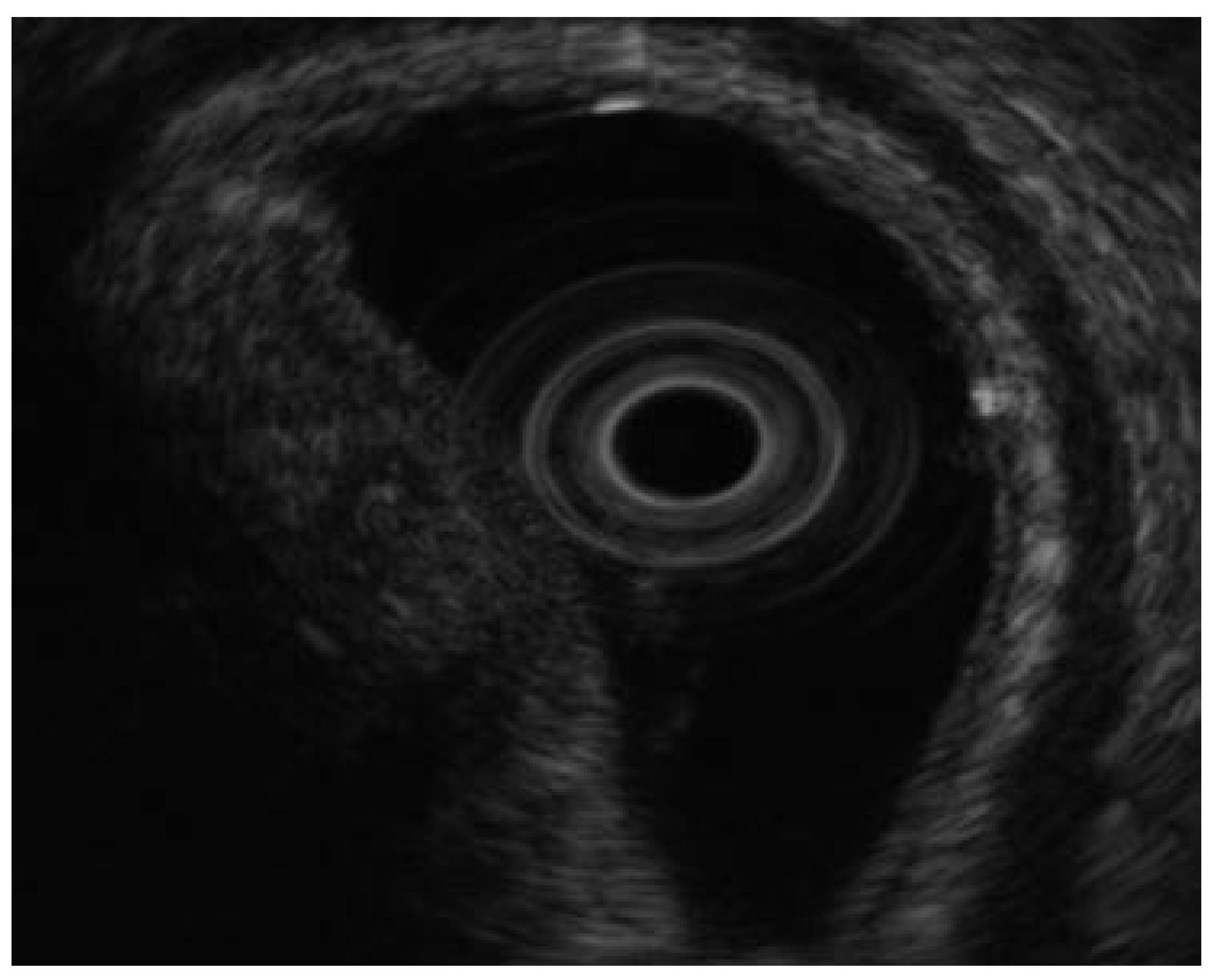
Colonoscopy also revealed sigmoidal stenosis with a smooth mucosal surface. Endoscopic ultrasonography was performed at the same time and revealed an iso- to high-echoic lesion in the 3rd echoic layer (submucosal layer) (Figure 2). In addition, endoscopic ultrasonography-guided fine needle aspiration biopsy (EUS-FNAB) was attempted, but sufficient specimens could not be obtained due to severe stenosis of the sigmoid colon.
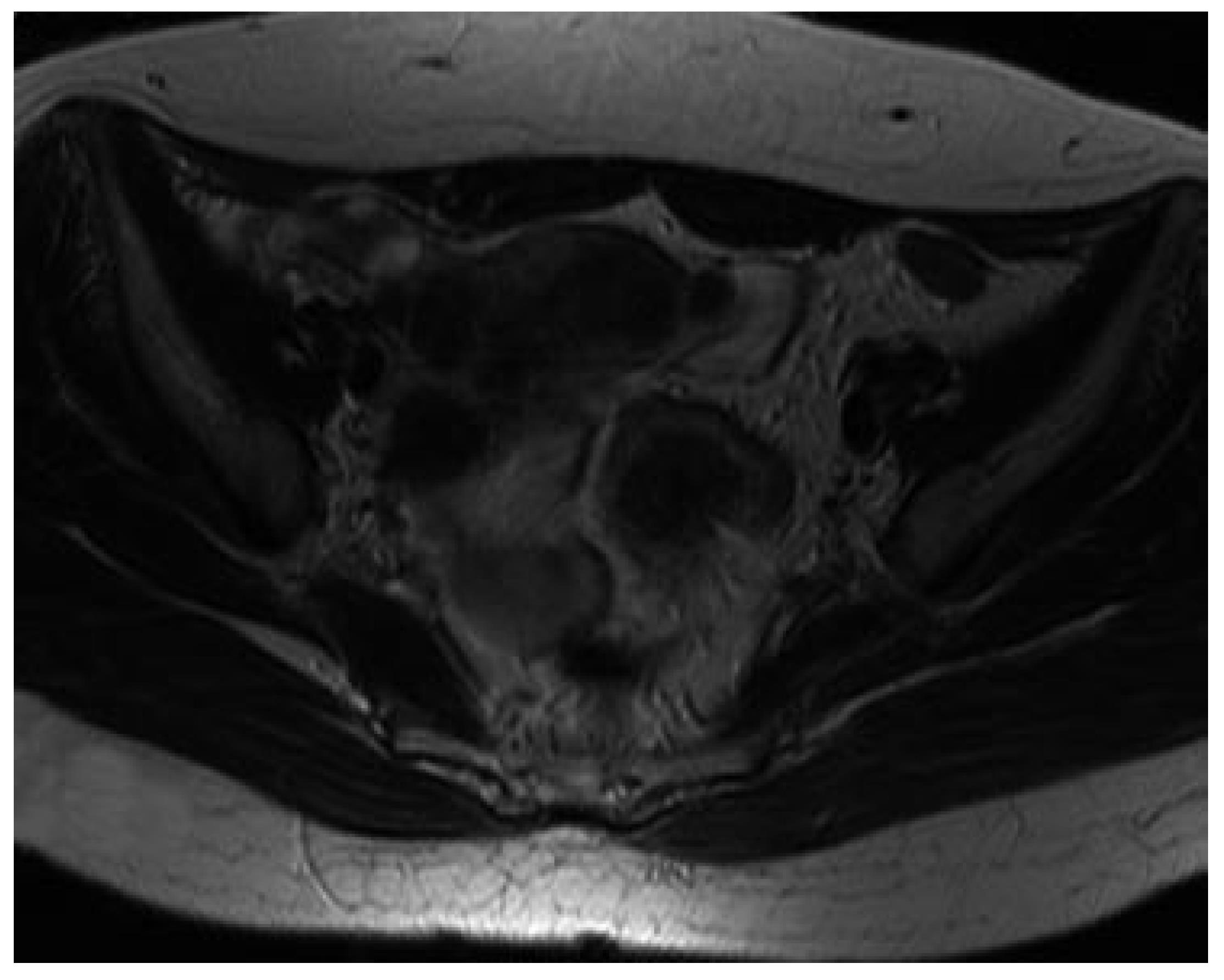
MRI was performed for evaluation and differential diagnosis of the submucosal tumor, revealing a tumor 3 cm in diameter in the sigmoid colon with signal hypointensity on both T1- and T2-weighted imaging (Figure 3; T2-weighted image only). Several small myomas were also seen in the uterus.
The sigmoid tumor was diagnosed as intestinal endometriosis from these examinations, for the following reasons: (1) the patient was a woman of reproductive age; (2) tumor was located in the sigmoid colon; (3) a submucosal tumor containing muscle and/or fibrous components was detected on MRI. As stenosis of the colon was severe and the patient wanted to have children in the near future, we selected sigmoid resection by laparoscopy-assisted sigmoidectomy with a minimal skin incision to prevent postoperative abdominal adhesions. Surgery was performed after informed consent was obtained from the patient.
Three trocars, including a 5-mm laparoscope, were introduced and a 4-cm minilaparotomy was performed in the left lower abdomen to retrieve the resected specimen and anastomose the colon. The operation was successful and she was discharged uneventfully 7 d after surgery.
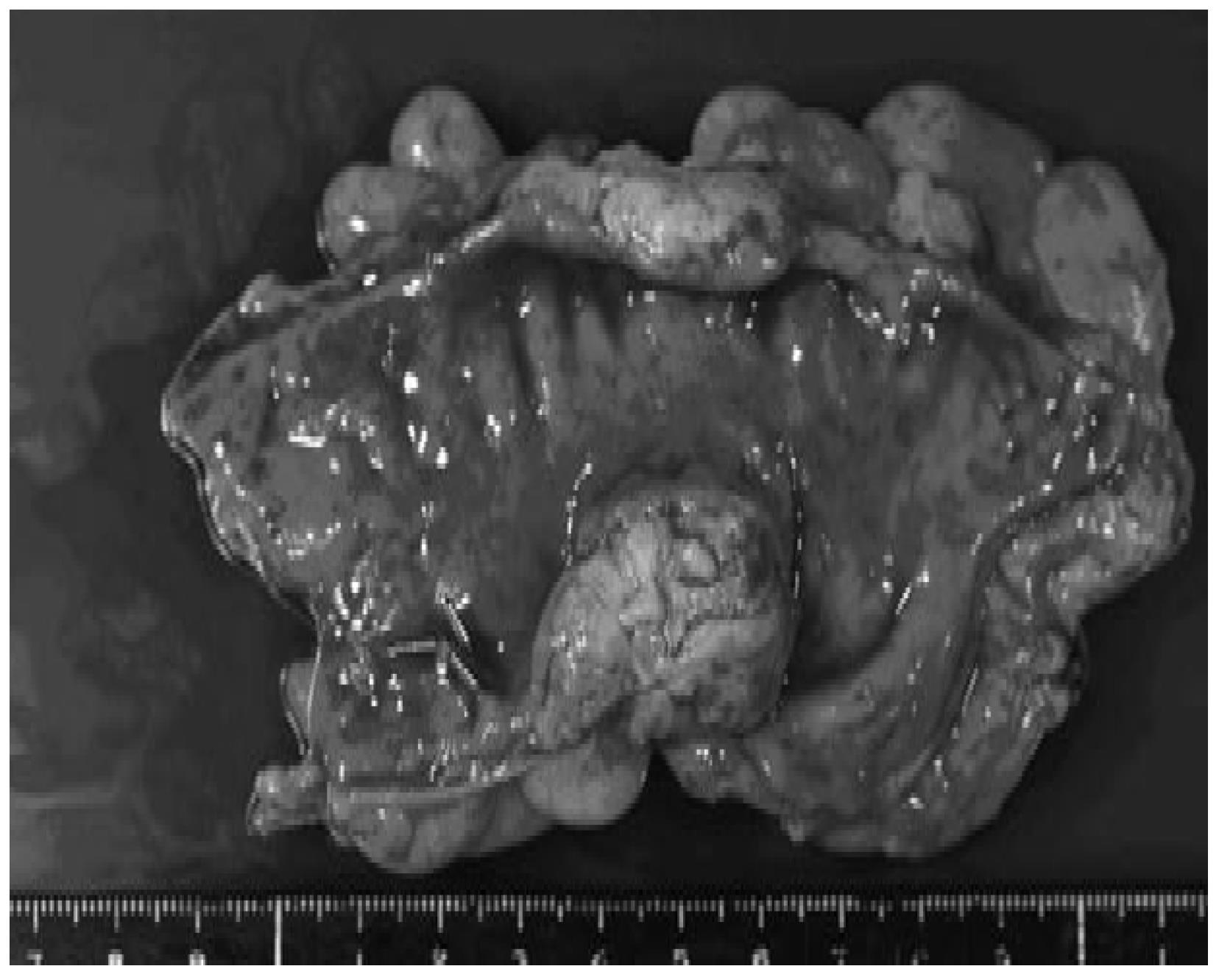
Gross examination of the resected specimen revealed a 30 mm × 20 mm × 15 mm hard submucosal mass, and the serous membrane of this site was indented to the tumor (Figure 4). No abnormality in the mucosal surface was identified.
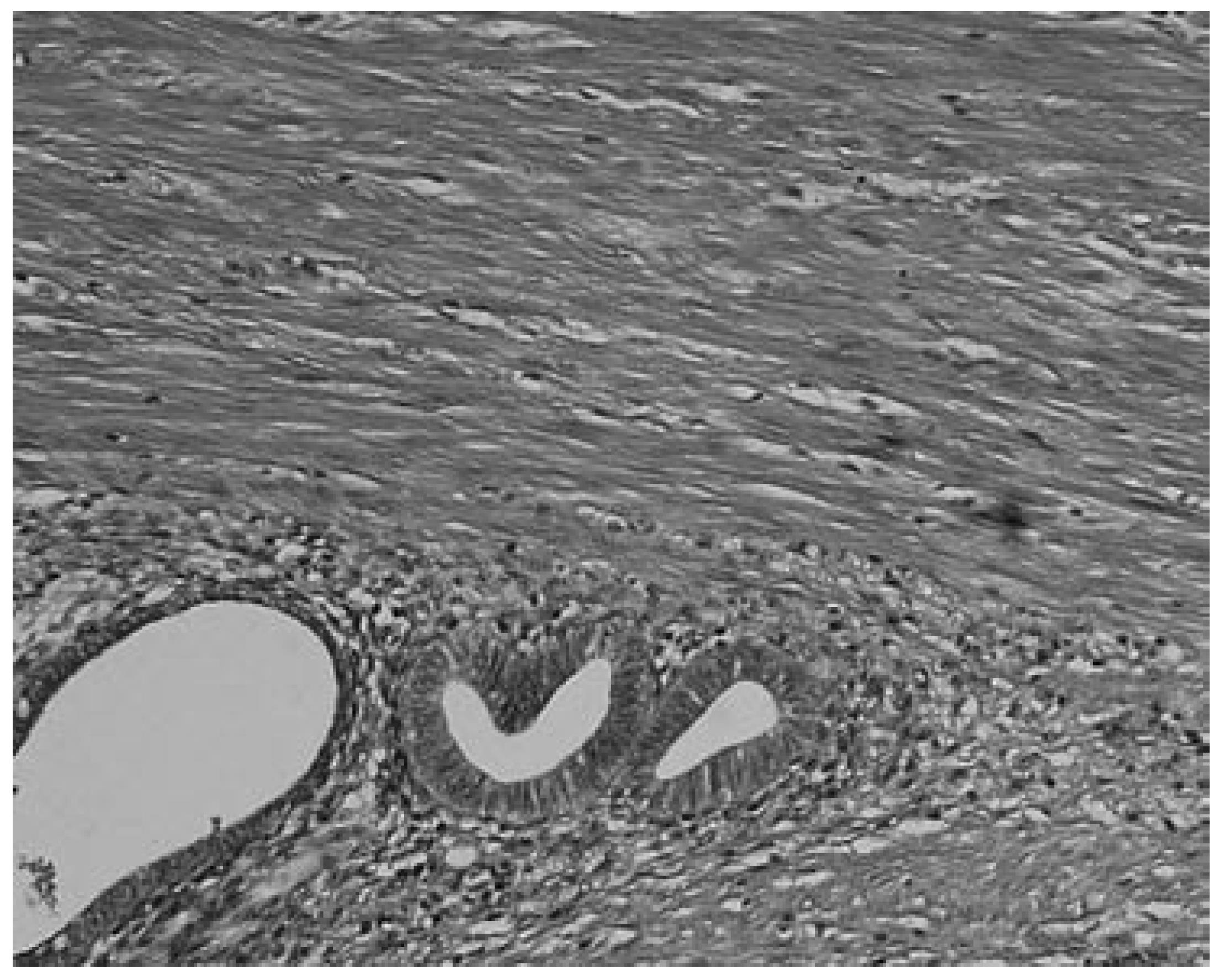
Histological examination revealed a mixture of smooth muscle cells and endometrial glands, without atypical cells and goblet cells, so the diagnosis of sigmoid endometriosis was confirmed (Figure 5).
Endometriosis is histologically defined as the presence of endometrial-like tissue outside the uterus[5]. This condition is thought to affect the intestinal tract in 15%-37% of patients with pelvic endometriosis[1]. The disease is not particularly rare among women of childbearing age, but many authors have reported that correct preoperative diagnosis is difficult[2-4]. This is because the symptoms such as abdominal pain, hemostool and decreased stool caliber are not specific for this disease, and hemostool or rectal bleeding are thought to result from mucosal injury during passage of stools through the narrowed intestinal lumen[2]. Some patients reportedly display symptoms associated with the menstrual cycle[2,4], but these patients represent only about 40% of all patients with endometriosis[6]. In addition, some reports have described aggravation of inflammatory bowel disease and irritable bowel syndrome during menstruation[7]. Symptoms alone are thus not helpful for differential diagnosis, and a similar situation is seen for laboratory examination of the blood. Mol et al[8] reported a systematic review of the diagnosis of endometriosis, and concluded that serum CA125 level may be elevated in endometriosis, but this measurement had no value as a diagnostic tool compared to laparoscopy.
Imaging examination is thus essential for the preo-perative diagnosis of intestinal endometriosis, but some reports have described preoperative confusion between this disease and cancer according to colonoscopy and CT with barium enema, particularly in patients with lesions involving the mucosal surface[3,4]. In such patients, MRI is helpful for differential diagnosis. In a typical endometrial lesion, MRI showed signal hyperintensity on T1-weighted imaging and signal hypointensity on T2-weighted imaging[9]. However, smooth muscle components are reportedly recognized frequently in endometrial lesions[10]. In such lesions, as seen in the present case, MRI indicates signal hypointensity on both T1- and T2-weighted imaging, and differential diagnosis from other diseases such as cancer and gastrointestinal stromal tumor is thus difficult. In fact, Chapron et al[11] reported that MRI specificity for deeply infiltrating endometriosis was 97.9%, but sensitivity was only 76.5%.
Endoscopic ultrasonography is also a useful and noninvasive examination for the diagnosis of intestinal endometriosis. Sensitivity and specificity are reportedly about 97% for the diagnosis of rectal involvement in patients with known pelvic endometriosis[12]. In addition, EUS-FNAB provides accurate tissue and may be the only procedure for correct preoperative diagnosis of intestinal endometriosis, but the overall specificity, sensitivity and accuracy of EUS-FNA for neoplasms of the gastrointestinal tract are reportedly 88%, 89% and 89%, respectively[13].
Biscaldi et al[14] reported the usefulness of multislice CT combined with distention of the colon by rectal enteroclysis for intestinal endometriosis. The sensitivity was 98.7% and specificity was 100% in identifying women with intestinal endometriosis. This method is thought to be very helpful for diagnosing intestinal endometriosis, but requires bowel preparation, such as the need for a low-residue diet for 3 d, drinking of 4-6 doses of a granular powder dissolved in 500 mL of water per dose and intravenous administration of iodinated contrast medium. This technique is thus inappropriate for patients with obstructive symptoms or allergy to iodinated contrast medium.
Among these examinations, we consider MRI and EUS (and/or EUS-FNAB) are the most useful examinations for intestinal endometriosis. However, it is important to perform valuable examinations for diagnosis of intestinal endometriosis, including radiological, histological and etiological examinations, as the condition basically involves a benign lesion requiring minimally invasive treatment. This disease should also be considered in the differential diagnosis for women of childbearing age presenting with gastrointestinal tract symptoms.
S-Editor Liu Y L-Editor Ma JY E- Editor Li HY
| 1. | Yantiss RK, Clement PB, Young RH. Endometriosis of the intestinal tract: a study of 44 cases of a disease that may cause diverse challenges in clinical and pathologic evaluation. Am J Surg Pathol. 2001;25:445-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 162] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 2. | Bartkowiak R, Zieniewicz K, Kamiński P, Krawczyk M, Marianowski L, Szymańska K. Diagnosis and treatment of sigmoidal endometriosis--a case report. Med Sci Monit. 2000;6:787-790. [PubMed] |
| 3. | Chu PW, Su HY, Ko CS. Endometriosis of the colon and rectum mimicking colon cancer. Int J Gynaecol Obstet. 2004;87:167-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Dimoulios P, Koutroubakis IE, Tzardi M, Antoniou P, Matalliotakis IM, Kouroumalis EA. A case of sigmoid endometriosis difficult to differentiate from colon cancer. BMC Gastroenterol. 2003;3:18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 45] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Kennedy S, Bergqvist A, Chapron C, D'Hooghe T, Dunselman G, Greb R, Hummelshoj L, Prentice A, Saridogan E. ESHRE guideline for the diagnosis and treatment of endometriosis. Hum Reprod. 2005;20:2698-2704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 992] [Cited by in RCA: 1002] [Article Influence: 50.1] [Reference Citation Analysis (0)] |
| 6. | Jubanyik KJ, Comite F. Extrapelvic endometriosis. Obstet Gynecol Clin North Am. 1997;24:411-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 127] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 7. | Kane SV, Sable K, Hanauer SB. The menstrual cycle and its effect on inflammatory bowel disease and irritable bowel syndrome: a prevalence study. Am J Gastroenterol. 1998;93:1867-1872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 109] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 8. | Mol BW, Bayram N, Lijmer JG, Wiegerinck MA, Bongers MY, van der Veen F, Bossuyt PM. The performance of CA-125 measurement in the detection of endometriosis: a meta-analysis. Fertil Steril. 1998;70:1101-1108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 195] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 9. | Puglielli E, Di Cesare E, Masciocchi C. Rectal endometriosis: MRI study with rectal coil. Eur Radiol. 2004;14:2362-2363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Anaf V, Simon P, Fayt I, Noel J. Smooth muscles are frequent components of endometriotic lesions. Hum Reprod. 2000;15:767-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 123] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 11. | Chapron C, Vieira M, Chopin N, Balleyguier C, Barakat H, Dumontier I, Roseau G, Fauconnier A, Foulot H, Dousset B. Accuracy of rectal endoscopic ultrasonography and magnetic resonance imaging in the diagnosis of rectal involvement for patients presenting with deeply infiltrating endometriosis. Ultrasound Obstet Gynecol. 2004;24:175-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 104] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 12. | Doniec JM, Kahlke V, Peetz F, Schniewind B, Mundhenke C, Löhnert MS, Kremer B. Rectal endometriosis: high sensitivity and specificity of endorectal ultrasound with an impact for the operative management. Dis Colon Rectum. 2003;46:1667-1673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Vander Noot MR, Eloubeidi MA, Chen VK, Eltoum I, Jhala D, Jhala N, Syed S, Chhieng DC. Diagnosis of gastrointestinal tract lesions by endoscopic ultrasound-guided fine-needle aspiration biopsy. Cancer. 2004;102:157-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 140] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 14. | Biscaldi E, Ferrero S, Fulcheri E, Ragni N, Remorgida V, Rollandi GA. Multislice CT enteroclysis in the diagnosis of bowel endometriosis. Eur Radiol. 2007;17:211-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 101] [Article Influence: 5.3] [Reference Citation Analysis (0)] |