Published online Oct 28, 2007. doi: 10.3748/wjg.v13.i40.5357
Revised: July 31, 2007
Accepted: August 14, 2007
Published online: October 28, 2007
AIM: To prospectively investigate serum CA 19-9 levels in type 2 diabetic patients in comparison with age- and gender-matched control subjects.
METHODS: We recorded duration of diabetes and examined fasting glucose levels, HbA1c levels and serum CA 19-9 levels in 76 type 2 diabetic patients and 76 controls. Abdominal CT was performed in order to eliminate abdominal malignancy in the diabetic and control groups.
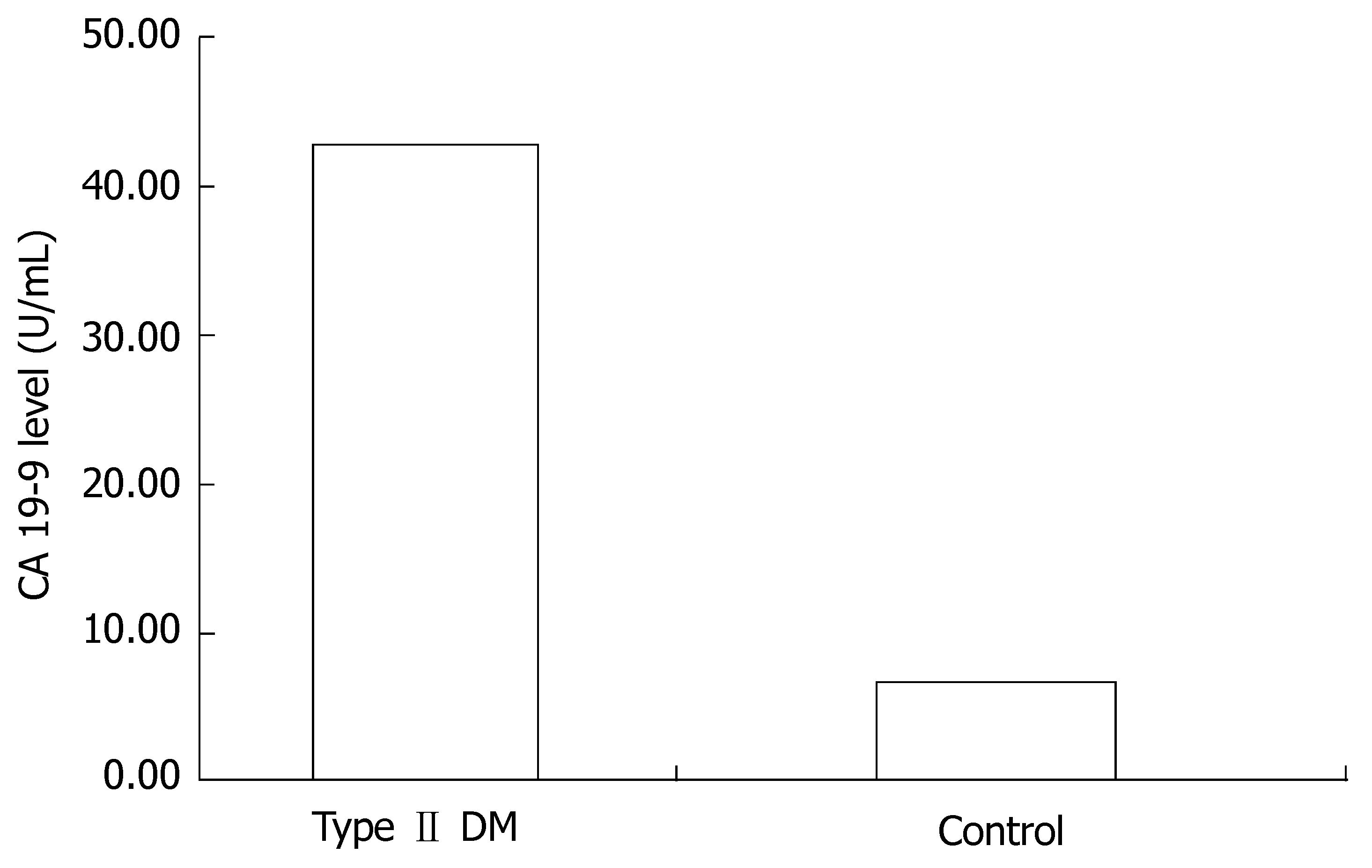
RESULTS: The average CA 19-9 level was 46.0 ± 22.4 U/mL for diabetic patients whereas it was 9.97 ± 7.1 U/mL for the control group (P < 0.001 ). Regression analysis showed a positive correlation between diabetes and CA 19-9 independent from age, gender, glucose level and HbA1c level (t = 8.8, P < 001 ). Two of the diabetic patients were excluded from the study because of abdominal malignancy shown by CT at the initial evaluation. For all patients, abdominal CT showed no pancreatic abnormalities.
CONCLUSION: CA 19-9 is a tumor-associated antigen, which is elevated in pancreatic, upper gastrointestinal tract, ovarian hepatocellular, and colorectal cancers, as well as in inflammatory conditions of the hepatobiliary system, biliary obstruction and in thyroid diseases. Diabetes has been claimed to be a risk factor for pancreatic cancer, which is increasing its incidence and has one of the lowest survival rates of all cancers. CA 19-9 is used in the diagnosis of pancreatic cancer but is also a marker of pancreatic tissue damage that might be caused by diabetes. We propose that a higher cut-off value of CA 19-9 should be used in diabetics to differentiate benign and malignant pancreatic disease, and subtle elevations of CA 19-9 in diabetics should be considered as the indication of exocrine pancreatic dysfunction.
- Citation: Uygur-Bayramiçli O, Dabak R, Orbay E, Dolapçıoğlu C, Sargın M, Kılıçoğlu G, Güleryüzlü Y, Mayadağlı A. Type 2 dıabetes mellıtus and CA 19-9 levels. World J Gastroenterol 2007; 13(40): 5357-5359
- URL: https://www.wjgnet.com/1007-9327/full/v13/i40/5357.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i40.5357
CA 19-9 is a tumor-associated antigen that was originally defined by a monoclonal antibody produced by a hybridoma prepared from murine spleen cells immunized with a human colorectal cancer cell line. CA 19-9 is elevated in pancreatic cancers, in cancers of the upper gastrointestinal tract, in ovarian cancer, hepatocellular cancer, colorectal cancer, as well as in inflammatory conditions of the hepatobiliary system and in thyroid diseases[1]. It may also be elevated in malignant and benign cases of biliary obstruction[2].
Diabetes has been claimed to be a risk factor for pancreatic cancer, which is increasing its incidence and has one of the lowest survival rates of all cancers[3].
The association between diabetes and pancreatic cancer remains controversial. A meta-analysis of 20 studies found a two-fold increased risk of pancreatic cancer among diabetic patients of 5 years duration, suggesting that diabetes is a risk factor for the tumor[4]. Other studies have concluded that cancer preceded and caused diabetes[5]. There are even some studies suggesting that diabetes protects against pancreatic cancer[6].
CA 19-9 is used in the diagnosis of pancreatic cancer but is also a marker of pancreatic tissue damage that might be caused by diabetes. Therefore it is necessary to define the normal range of CA 19-9 in type 2 diabetic patients in order to eliminate additional interventional approaches. In this study, we prospectively evaluated serum CA 19-9 levels in type 2 diabetic patients in comparison with age- and gender-matched control subjects.
76 consecutive, type 2 diabetic patients and 76 age- and gender-matched healthy controls comprised the study groups. We recorded duration of diabetes and examined fasting glucose levels, HbA1c and serum CA 19-9 levels. CA 19-9 was measured with a chemilluminecence immunoassay (Roche Diagnostics E 170 analyser). The normal range of CA 19-9 was defined as less than 27 U/mL. Abdominal CT was performed in order to eliminate abdominal malignities for the diabetic and control groups.
Characteristic features of the control and study groups are shown in Table 1. Two of the diabetic patients were excluded from the study because of abdominal malignancy found with CT at the initial evaluation (one had an adrenal mass and the other prostatic carcinoma).
| Sex | Mean age(yr) | ||
| Male | Female | ||
| Type II DM | 19 | 55 | 53.3 |
| Control | 17 | 59 | 52.5 |
Average CA 19-9 levels were 46.0 ± 22.4 U/mL in diabetic patients whereas it was found to be 9.97 ± 7.1 U/mL in the control group (P < 0.001). Regression analysis showed a positive correlation between diabetes and CA 19-9, independent from age, gender, glucose level and HbA1c level (t = 8.8, P < 001) (Figure 1). For all patients, abdominal CT showed no pancreatic abnormalities.
Diabetes mellitus is a chronic inflammatory disease of the pancreas. The mechanisms of glucose intolerance include insulin resistance and destruction of islet beta cells. Most of these conditions damage exocrine tissue and islet cells and both of these systems are anatomically and functionally related. There are no capsules or basement membranes around islets and there are cell-to-cell contacts between exocrine and endocrine cells. There are direct connections between the capillaries of islets and acini that underlie the regulatory connections between islet hormones and exocrine pancreatic secretion, or in other words the relation between parenchymal disease and beta-cell dysfunction[3].
Insulitis is a progressive phenomenon in diabetes mellitus. The United Kingdom Prospective Diabetes Study evaluated beta cell function in diabetes using the homeostasis model assessment and found that beta cell function was already reduced by 50% at diagnosis and that there was subsequent deterioration regardless of therapy[7]. Diabetes can even be described as the last step of chronic pancreatitis with the new developing concepts of pathogenesis[8].
On the other hand, patients with chronic pancreatitis often suffer from endocrine pancreatic dysfunction, which leads to a secondary form of diabetes. This form of diabetes accounts for < 1% of all diabetic cases[8]. Eighty percent of patients with chronic pancreatitis develop an overt diabetes mellitus in the long run and diabetes mellitus is an independent risk factor for mortality in patients with chronic pancreatitis[9,10]. Chronic pancreatitis is a risk factor for pancreatic cancer[11] and the same is also true for diabetes[3]. Therefore diabetic patients have to be followed up for pancreatic cancer.
CA 19-9 is a tumor marker used for the diagnosis of pancreatic cancer with a sensitivity of 70%-90% and a specificity of 68%-91%[12]. The main limitation of CA 19-9 is that it can also be elevated in patients with nonmalignant obstructive jaundice, thyroid disease and ovarian diseases resulting in impaired specificity of the marker. The solution to this problem was found with the use of higher cut-off values and a combination of tumor markers in differential diagnosis of gastrointestinal cancers. Lewis blood group status is also important for the interpretation of CA 19-9 because 10% of the Caucasian population who are Lewis genotype negative are unable to express CA 19-9[13]. Diabetes is also associated with an increased risk of hepatocellular carcinoma[14].
Taking the close relation between exocrine and endocrine pancreatic function into consideration, the use of CA 19-9 in diabetics is controversial. The relationship between diabetes mellitus and CA 19-9 has been studied by Benhamou et al[15] and they investigated the relationship between CA 19-9 and metabolic control of diabetes in 51 adult patients. They concluded that CA 19-9 in diabetic patients is raised in acute metabolic situations, which correlated very well with blood glucose concentration.
In contrast to Benhamou et al, 64 diabetic patients examined by Banfi et al[16] showed no correlation between CA 19-9 and biochemical markers of metabolic compensation in diabetes. In our study we also found that CA 19-9 levels were higher in diabetic patients in comparison to controls (P < 0.001 ). The elevation of CA 19-9 in diabetics was less than twice of the normal range. Regression analysis showed a positive correlation between diabetes and CA 19-9 independent from age, gender, glucose level and HbA1c level (t = 8.8, P < 001). We could not identify any pancreatic or gastrointestinal cancer in the diabetic patients with a high level of CA 19-9, which is consistent with the concept of exocrine pancreatic dysfunction in diabetes.
We propose that a higher cut-off value for CA 19-9 should be used for diabetics to differentiate benign and malignant pancreatic disease, and subtle elevations of CA 19-9 in diabetics should be considered as an indication of exocrine pancreatic dysfunction.
Ca 19-9 is a widely used antigen in the diagnosis of pancreatic and gastrointestinal cancers but its elevation might also be due to some nonspecific causes. Chronic inflammation such as diabetes mellitus can lead to pancreatic tissue damage and to a nonmalignant cause of high Ca 19-9 levels. Therefore the "normal" interval of Ca19-9 should be in defined in type 2 diabetic patients.
Insulitis is a progressive phenomenon in type 2 diabetes and United Kingdom Prospective Diabetes Study confirmed this entity.Chronic pancreatitis is a risk factor for diabetes and also for pancreatic cancer. The studies by Benhamou and Banfi found controversial data regarding the correlation between Ca 19-9 and diabetes.
Elevation of Ca 19-9 in type 2 diabetics has been associated with bad metabolic control in previous studies and no morphological studies was done. We performed abdominal CT in all the patients in order to exclude any pancreatic malignancy and found out that Ca 19-9 was elevated in all the diabetic patients.
We have to define a new cut-off value for Ca 19-9 level in type 2 diabetics in order to eliminate unnecessary investigations for pancreatic cancer in this subgroup.This article can lead to further study the effect of insulitis and chronic pancreatitis on Ca 19-9 expression in experimental and morphological studies.
Ca 19-9 is a tumor-associated antigen which is originally defined by a monoclonal antibody that has been produced by a hybridoma prepared from murine spleen cells immunized with a human colorectal cancer cell line.
This study has interesting scientific and innovative contents, and good readability.
S- Editor Liu Y L- Editor Lutze M E- Editor Li JL
| 1. | Locker GY, Hamilton S, Harris J, Jessup JM, Kemeny N, Macdonald JS, Somerfield MR, Hayes DF, Bast RC. ASCO 2006 update of recommendations for the use of tumor markers in gastrointestinal cancer. J Clin Oncol. 2006;24:5313-5327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1057] [Cited by in RCA: 1111] [Article Influence: 58.5] [Reference Citation Analysis (0)] |
| 2. | Murray MD, Burton FR, Di Bisceglie AM. Markedly elevated serum CA 19-9 levels in association with a benign biliary stricture due to primary sclerosing cholangitis. J Clin Gastroenterol. 2007;41:115-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Mohan V, Premalatha G, Pitchumoni CS. Pancreatic diseases and diabetes. Textbook of diabetes.Third edition. USA: Blackwell Publishing 2003; 28: 1-15. |
| 4. | Rosewicz S, Wiedenmann B. Pancreatic carcinoma. Lancet. 1997;349:485-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 202] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 5. | Everhart J, Wright D. Diabetes mellitus as a risk factor for pancreatic cancer. A meta-analysis. JAMA. 1995;273:1605-1609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 410] [Cited by in RCA: 376] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 6. | Gullo L. Diabetes and the risk of pancreatic cancer. Ann Oncol. 1999;10 Suppl 4:79-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | U.K. Prospective Diabetes Study 16. Overview of 6 years' therapy of type II diabetes: a progressive disease. U.K. Prospective Diabetes Study Group. Diabetes. 1995;44:1249-1258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1087] [Cited by in RCA: 1008] [Article Influence: 33.6] [Reference Citation Analysis (0)] |
| 8. | Göke FJM, Göke B. Optimal control of diabetes mellitus in pancreatitis. Pancreatitis: Advances in pathobiology, diagnosis and treatment. Dordrecht: Springer 2005; 226-232. |
| 9. | Malka D, Hammel P, Sauvanet A, Rufat P, O'Toole D, Bardet P, Belghiti J, Bernades P, Ruszniewski P, Lévy P. Risk factors for diabetes mellitus in chronic pancreatitis. Gastroenterology. 2000;119:1324-1332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 193] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 10. | Levy P, Milan C, Pignon JP, Baetz A, Bernades P. Mortality factors associated with chronic pancreatitis. Unidimensional and multidimensional analysis of a medical-surgical series of 240 patients. Gastroenterology. 1989;96:1165-1172. [PubMed] |
| 11. | Lowenfels AB, Maisonneuve P. Chronic pancreatitis: precursor of carcinoma? Pancreatitis: Advances in pathobiology, diagnosis and treatment. Dordrecht; The Netherlands: Springer 2005; 232-239. |
| 12. | Goonetilleke KS, Siriwardena AK. Systematic review of carbohydrate antigen (CA 19-9) as a biochemical marker in the diagnosis of pancreatic cancer. Eur J Surg Oncol. 2007;33:266-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 539] [Cited by in RCA: 611] [Article Influence: 32.2] [Reference Citation Analysis (1)] |
| 13. | Aoki Y, Yanagisawa Y, Ohfusa H, Kawa S, Oguchi H, Furuta S. Elevation of serum CA 19-9 in parallel with HbA1c in a diabetic female with the Lewis(a+b-) blood group. Diabetes Res Clin Pract. 1991;13:77-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | El-Serag HB, Hampel H, Javadi F. The association between diabetes and hepatocellular carcinoma: a systematic review of epidemiologic evidence. Clin Gastroenterol Hepatol. 2006;4:369-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 581] [Cited by in RCA: 601] [Article Influence: 31.6] [Reference Citation Analysis (0)] |
| 15. | Benhamou PY, Vuillez JP, Halimi S, Meffre G, Bachelot I. Influence of metabolic disturbances of diabetes mellitus on serum CA 19-9 tumor marker. Diabete Metab. 1991;17:39-43. [PubMed] |
| 16. | Banfi G, Ardemagni A, Bravi S, Pacchioni M, Bonini P. Are diabetic metabolic compensation and CA19.9 really correlated? Int J Biol Markers. 1996;11:207-210. [PubMed] |