Published online Jan 28, 2007. doi: 10.3748/wjg.v13.i4.585
Revised: November 4, 2006
Accepted: December 25, 2006
Published online: January 28, 2007
AIM: To compare rigid proctoscope and flexible endoscope for elastic band ligation of internal hemorrhoids.
METHODS: Patients between 18 and 80 years old, with chronic complaints (blood loss, pain, itching or prolapse) of internal hemorrhoids of grade I-III, were randomized to elastic band ligation by rigid proctoscope or flexible endoscope (preloaded with 7 bands). Patients were re-treated every 6 wk until the cessation of complaints. Evaluation by three-dimensional anal endosonography was performed.
RESULTS: Forty-one patients were included (median age 52.0, range 27-79 years, 20 men). Nineteen patients were treated with a rigid proctoscope and twenty two with a flexible endoscope. Twenty-nine patients had grade I hemorrhoids, 9 patients had grade II hemorrhoids and 3 patients had grade III hemorrhoids. All patients needed a minimum of 1 treatment and a maximum of 3 treatments. A median of 4.0 bands was used in the rigid proctoscope group and a median of 6.0 bands was used in the flexible endoscope group (P < 0.05). Pain after ligation tended to be more frequent in patients treated with the flexible endoscope (first treatment: 3 vs 10 patients, P < 0.05). Three-dimensional endosonography showed no sphincter defects or alterations in submucosal thickness.
CONCLUSION: Both techniques are easy to perform, well tolerated and have a good and fast effect. It is easier to perform more ligations with the flexible endoscope. Additional advantages of the flexible scope are the maneuverability and photographic documentation. However, treatment with the flexible endoscope might be more painful and is more expensive.
- Citation: Cazemier M, Felt-Bersma R, Cuesta M, Mulder C. Elastic band ligation of hemorrhoids: Flexible gastroscope or rigid proctoscope? World J Gastroenterol 2007; 13(4): 585-587
- URL: https://www.wjgnet.com/1007-9327/full/v13/i4/585.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i4.585
The initial treatment of symptomatic internal hemorrhoids is conservative and consists of a fiber enriched diet, increased fluid intake, prevention of straining and local hygiene, which may be combined with local anesthetic and antiphlogistic medication[1,2]. Over 90% of patients with symptomatic hemorrhoids can be treated conservatively or by rubber band ligation. Infrared coagulation and cryotherapy are also options, but are no longer commonly applied[3]. Surgery is reserved for the most severe cases. Since the early sixties the treatment of choice for persisting internal hemorrhoids is elastic band ligation by means of a rigid proctoscope (Barron ligation)[4,5]. Wrobleski et al[6] reported results of long term follow up (mean of 60 mo) of 266 patients; 80% had fewer symptoms and 69% had no symptoms. The procedure is usually safe and can be easily repeated[7]. Some studies evaluated the use of a flexible endoscope equipped with a ligation cap, normally used for ligation of esophageal varices, in treating hemorrhoids[8-11].A flexible endoscope could have some advantages such as more maneuverability, a wider view and photographic documentation. The present prospective randomized trial was performed to compare both techniques in effectiveness. Additionally we used a three-dimensional endosonography to evaluate changes in the submucosa and sphincter defects.
Patients between 18 and 80 years old, with chronic complaints (blood loss, pain, itching or prolapse) of internal hemorrhoids grade I-III, were randomized by computer software to elastic band ligation by rigid proctoscope or gastroscope (Olympus Excera®). Patients were re-treated every 6 wk till the cessation of complaints.
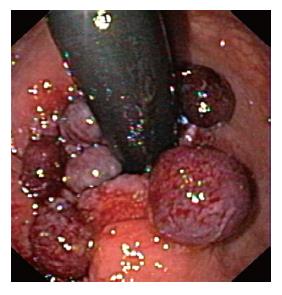
The rigid proctoscope was gently introduced and then elastic bands were applied using a standard elastic band applicator in anterograde fashion. For endoscopic ligation, a single-use multiband ligator device (Sevenshooter®, Boston Scientific, USA) was attached to the end of a gastroscope. The device can only be attached to a gastroscope. The Sevenshooter is provided with 7 bands. The hemorrhoids were suctioned into the ligation cap in either retrograde or antegrade fashion. The number of bands applied depended on the amount of hemorrhoidal tissue present. All treatments were performed in an outpatient setting.
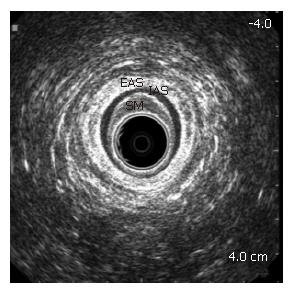
A three-dimensional anal endosonography was made before the first treatment and 6 wk after the last treatment. Endosonography was performed, using a three dimensional diagnostic ultrasound system (Hawk type 2102, B-K Medical) with a 16 MHz rotating endoprobe (type 1850, focal range 2 to 4.5 cm) covered by a hard sonolucent cone (diameter 1.7 cm) filled with water, producing a 360° view. Three dimensional anal endosonography was performed according to a standard procedure. The endoprobe was covered with a lubricated condom which was filled with ultrasound gel. The probe was then introduced into the rectum and a recording was made of the distal part of the rectum, the puborectalis muscle and the anal canal. After the endosonography, images were reconstructed to three dimensional images by computer software. The Medical Ethical Committee granted approval for this study.
Data are presented as a median with range. Differences between groups were assessed with a Mann-Whitney test, Chi square test or Fischer’s exact test when appropriate. P < 0.05 was taken as significant.
Detailed demographic and clinical data are shown in Table 1. Forty-one patients (median age 52, range 27-79 years, 20 men) with recurrent rectal bleeding, pain, itching or prolapse underwent ligation. Nobody had been treated previously. All procedures were easy to perform. Sometimes, in patients treated with the flexible endoscope, a rectal enema was needed when the rectum was not clean.
| Proctoscope | Gastroscope | |
| n | 19 | 22 |
| Age [median (range)] | 53 (27-75) | 50.5 (33-79) |
| Male/Female | 7/12 | 13/9 |
| Hemorrhoids grade I | 15 | 14 |
| Hemorrhoids grade II | 4 | 5 |
| Hemorrhoids grade III | 0 | 3 |
| No of treatments [median (range)] | 1.0 (1-3) | 1.0 (1-3) |
| No of total ligations [median (range)] | 4.0 (2-10) | 6.0 (1-15)a |
| Pain after treatment | 3 | 10a |
| Cost | 3 euro | 150 euro |
Nineteen patients were treated with a rigid proctoscope and twenty two with a flexible endoscope. Twenty-nine, 9, and 3 patients had grade I, II and III hemorrhoids, respectively.
Patients treated with a proctoscope needed a median of 1 treatment (range 1-3) and patients treated with an endoscope also needed a median of 1 treatment (range 1-3, P = 0.664).
A median of 4 bands (range 2-10) was used in the rigid proctoscope group and a median of 6 bands (range 1-15) was used in the flexible endoscope group (P < 0.05) (Figure 1).
In the group treated with a rigid proctoscope, 5 patients needed 1 re-treatment and 1 patient needed 2 re-treatments. In the group treated with a flexible endocope, 2 patients needed 1 re-treatment and 1 patient needed 2 re-treatments.
Two patients were excluded from follow up: One patient had a rupture of an abdominal aortic aneurysm and 1 patient developed an anal fissure.
Pain after ligation was more frequent in patients treated with the flexible endoscope (first treatment: 3 vs 10 patients, P < 0.05). The single-use ligation device (Sevenshooter®) costs approximately 150 euro for one set (2005). One elastic band for the rigid proctoscope costs approximately 0.50 euro. Further costs (cleaning of the gastroscope and proctoscope, personnel costs) did not substantially differ between both techniques.
With three-dimensional endosonography 30 patients were evaluated before and after treatment. Hemorrhoidal tissue was clearly visible in all patients. No sphincter defects were found before and after treatment and there was no significant change in submucosa thickness after endoscopic/proctoscopic treatment (Figure 2). After one year follow up, 5 patients needed re-treatment (2 proctoscope, 3 gastroscope).
Hemorrhoids are a major health problem; the community-wide prevalence in the Western World is reported to be around 4%. Adequate intake of fluids and fiber, use of suppositories, stool softeners and topical creams are important in the treatment of hemorrhoids, especially in grade I disease. When conservative treatment fails, there are still options, including surgical therapy.
Rubber band ligation with a proctoscope is very effective and inexpensive. Since 2005, it has been the treatment of choice. Studies have been undertaken investigating effectiveness and new techniques[12-14].
There have been 4 studies that analyzed the use of a flexible endoscope for hemorrhoidal elastic band ligation[8-11]. These studies conclude that it is a safe and efficient method with some advantages, although costs are still a major drawback. Only one study compared endoscopic band ligation (reusable) with the conventional rubber band ligation through a rigid proctoscope[10].
In our pilot study we found that both techniques were easy to perform, well tolerated and had a good and fast effect. It was easier to perform more ligations with the flexible endoscope. No serious adverse events were reported. Additional advantages of the flexible scope were the maneuverability and photographic documentation.
However, treatment with the flexible endoscope seemed to be more painful and was more expensive. More pain sensation can be explained by the learning curve we had to deal with and that more bands could be applied. In contrast, Wehrmann et al[10] found no significant difference in pain and reported that the total number of bands applied was significantly lower in the group treated with the endoscope.
So far as we know, this is the first study that evaluated with three-dimensional endosonography the presence of possible sphincter defects and changes in the submucosa. Poen et al[15] already found, with two-dimensional endosonography, no difference in appearance of the anal configuration after treatment with either rubber band ligation or infrared coagulation. In our study no significant alterations or sphincter defects were found and these endosonographic findings confirmed that band ligation is a safe technique.
When costs can be reduced the endoscopic treatment of hemorrhoids can be a good alternative for ligation with the rigid proctoscope.
In summary, endoscopic ligation is an effective, safe treatment and is comparable with proctoscopic ligation. However, the treatment is more expensive.
S- Editor Liu Y L- Editor Zhu LH E- Editor Bi L
| 1. | Poen AC, Felt-Bersma RJ, Cuesta MA, Devillé W, Meuwissen SG. A randomized controlled trial of rubber band ligation versus infra-red coagulation in the treatment of internal haemorrhoids. Eur J Gastroenterol Hepatol. 2000;12:535-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 30] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Johanson JF, Sonnenberg A. The prevalence of hemorrhoids and chronic constipation. An epidemiologic study. Gastroenterology. 1990;98:380-386. [PubMed] |
| 3. | Madoff RD, Fleshman JW. American Gastroenterological Association technical review on the diagnosis and treatment of hemorrhoids. Gastroenterology. 2004;126:1463-1473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 127] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 4. | Blaisdell PC. Office ligation of internal hemorrhoids. Am J Surg. 1958;96:401-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 41] [Article Influence: 1.6] [Reference Citation Analysis (1)] |
| 5. | Barron J. Office ligation of internal hemorrhoids. Am J Surg. 1963;105:563-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 117] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 6. | Wrobleski DE, Corman ML, Veidenheimer MC, Coller JA. Long-term evaluation of rubber ring ligation in hemorrhoidal disease. Dis Colon Rectum. 1980;23:478-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 36] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Iyer VS, Shrier I, Gordon PH. Long-term outcome of rubber band ligation for symptomatic primary and recurrent internal hemorrhoids. Dis Colon Rectum. 2004;47:1364-1370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 96] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 8. | Trowers EA, Ganga U, Rizk R, Ojo E, Hodges D. Endoscopic hemorrhoidal ligation: preliminary clinical experience. Gastrointest Endosc. 1998;48:49-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Dickey W, Garrett D. Hemorrhoid banding using videoendoscopic anoscopy and a single-handed ligator: an effective, inexpensive alternative to endoscopic band ligation. Am J Gastroenterol. 2000;95:1714-1716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Wehrmann T, Riphaus A, Feinstein J, Stergiou N. Hemorrhoidal elastic band ligation with flexible videoendoscopes: a prospective, randomized comparison with the conventional technique that uses rigid proctoscopes. Gastrointest Endosc. 2004;60:191-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Fukuda A, Kajiyama T, Arakawa H, Kishimoto H, Someda H, Sakai M, Tsunekawa S, Chiba T. Retroflexed endoscopic multiple band ligation of symptomatic internal hemorrhoids. Gastrointest Endosc. 2004;59:380-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Takano M, Iwadare J, Ohba H, Takamura H, Masuda Y, Matsuo K, Kanai T, Ieda H, Hattori Y, Kurata S. Sclerosing therapy of internal hemorrhoids with a novel sclerosing agent. Comparison with ligation and excision. Int J Colorectal Dis. 2006;21:44-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 46] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 13. | Kwok SY, Chung CC, Tsui KK, Li MK. A double-blind, randomized trial comparing Ligasure and Harmonic Scalpel hemorrhoidectomy. Dis Colon Rectum. 2005;48:344-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 52] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 14. | Fukuda A, Kajiyama T, Kishimoto H, Arakawa H, Someda H, Sakai M, Seno H, Chiba T. Colonoscopic classification of internal hemorrhoids: usefulness in endoscopic band ligation. J Gastroenterol Hepatol. 2005;20:46-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Poen AC, Felt-Bersma RJF, Cuesta MA, Meuwissen SGM. Anal endosonography in haemorrhoidal disease: do anatomical changes have clinical implications? Colorectal Dis. 1999;1:146-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |