Published online Oct 7, 2007. doi: 10.3748/wjg.v13.i37.5025
Revised: July 26, 2007
Accepted: July 30, 2007
Published online: October 7, 2007
AIM: To evaluate the value of 18F-DG PET/CT in detecting recurrence and/or metastasis of colorectal cancer (CRC).
METHODS: Combined visual analysis with semiquantitative analysis, the 18F-DG PET/CT whole-body imaging results and the corresponding clinical data of 68 postoperative CRC patients including 48 male and 20 female with average age of 58.1 were analyzed retrospectively.
RESULTS: Recurrence and/or metastasis were confirmed in 56 patients in the clinical follow-up after the PET/CT imaging. The sensitivity of PET/CT diagnosis of CRC recurrence and/or metastasis was 94.6%, and the specificity was 83.3%. The positive predictive value (PPV) was 96.4% and the negative predictive value (NPV) was 76.9%. PET/CT imaging detected one or more occult malignant lesions in 8 cases where abdominal/pelvic CT and/or ultrasonography showed negative findings, and also detected more lesions than CT or ultrasonography did in 30.4% (17/56) cases. Recurrence and/or metastasis was detected in 91.7% (22/24) cases with elevated serum CEA levels by 18F-DG PET/CT imaging.
CONCLUSION: 18F-DG PET/CT could detect the recurrence and/or metastasis of CRC with high sensitivity and specificity.
- Citation: Chen LB, Tong JL, Song HZ, Zhu H, Wang YC. 18F-DG PET/CT in detection of recurrence and metastasis of colorectal cancer. World J Gastroenterol 2007; 13(37): 5025-5029
- URL: https://www.wjgnet.com/1007-9327/full/v13/i37/5025.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i37.5025
Colorectal cancer (CRC) is the most common gastrointestinal malignancy, and its incidence and mortality is still rising in China[1,2]. Radical resection and postoperative chemotherapy remains to be the major management of CRC, but recurrence and/or metastasis occurs in 30%-50% of the patients after surgery[3-6]. An early diagnosis and accurate staging of postoperative metastasis is crucial for prescribing an optimal individualized chemotherapy regimen and thus elevating the survival rate. Combined positron emission tomography and computed tomography (PET/CT) is currently widely used in clinical diagnosis of cancer, showing great superiority in tumor staging[7-9]. In the present research, we investigated the diagnostic significance of fluorine 18 fluorodeoxyglucose (18F-DG) PET/CT in postoperative recurrence and/or metastasis of CRC by conducting a retrospective study of 68 patients.
A total of 68 postoperative CRC patients, 48 male and 20 female, examined in the PET/CT center of Jinling Hospital between August 2004 and August 2006 were included in the study cohort. The age of the patients ranged from 27 to 77 years, and the average was 58.1. A whole-body 18F-DG PET/CT was conducted in each case. The interval time between the operation and the examination ranged from 4 mo to 8 years, and the average was 2.5 years. The diagnosis of recurrence and/or metastasis was based on pathological evidence, colonoscopy findings, medical imaging results, and clinical follow-up outcome. The follow-up time ranged from 5 to 28 mo.
Biography sensation 16 PET/CT (Siemens, Germany) was used. 18F-DG was produced by TR19 cyclotron (EBCO, Canada) and automatic chemical synthesizer (Beijing Patborn Biotech, China). The synthesis efficiency was 701%, and the radiochemical purity was higher than 95%. Prior to the FDG injection, blood samples were drawn from all patients to assure fasting glucose levels to be less than 6.60 mmol/L. Afterwards, 296-444 MBq of FDG was administered intravenously, and patients waited 50-60 min before undergoing PET and CT scanning. PET emission images were obtained with a weight-based protocol for 5-7 bed positions, with 3 min of acquisition time per bed position. A delayed imaging of the region of interest (ROI) or suspicious lesion region was conducted 3 h later. High resolution CT (HRCT) was conducted if any lesion was detected in the lung. Traverse, sagital and coronary sections of CT, PET and combined PET/CT were obtained, with a section thickness of 5 mm, by reconstruction using an iterative algorithm, with CT-based attenuation correction applied.
Image interpretation had been individually performed by more than 2 experienced board-certified nuclear medicine physicians and radiologists. Visual assessment and semi-quantitative analysis were adopted in the image interpretation. ROI was determined at the section most clearly showing the hyper-intensive radioactivity, and the maximum standardized uptake value (SUVmax) was accessed. The diagnosis of a positive lesion was based on a SUVmax higher than 2.5 in the early imaging, while a typical positive lesion on a SUVmax higher than 2.5 and also SUVmax (ΔSUVmax = SUVmax,delayed-SUVmax, early) higher than 20% in the delayed imaging. The diagnosis of a malignancy lesion should be simultaneously based on the CT findings including the shape, size, intensity and distribution of the lesion, which could differentiate the physiological uptake.
Among the 68 examinees, recurrence and/or metastasis were later diagnosed in 56 patients, including 8 recurrences, 46 metastases, and 2 recurrence and metastases. The sensitivity of PET/CT diagnosis of CRC recurrence and/or metastasis was 94.6%, and the specificity was 83.3%. The positive predictive value (PPV) was 96.4% and the negative predictive value (NPV) was 76.9%. In 8 cases which abdominal/pelvic CT and/or ultrasonography showed negative findings, PET/CT imaging detected one or more occult malignant lesions, resulting in altered clinical staging. In 30.4 % (17/56) cases, PET/CT imaging detected more lesions than CT and ultrasonography did, showing disseminated metastases. PET/CT imaging displayed a superior sensitivity in detecting stump recurrence, local and distant metastasis compared with non-contrast CT scanning. Metastases were commonly detected in liver (18/56, 32.1%), lung (15/56, 26.8%), abdominal cavity and mesentery (14/56, 25%), retroperitoneum and psoas major (11/56, 19.6%). Others included bone, mediastinum lymph node, peritoneum, adrenal gland, ovary and brain. Liver and lung were the preferred metastasis foci, and blood metastasis was the major route of metastasis, followed by lymph node metastasis.
The treatment plans of 11 cases (11/68, 16.2%) were altered based on the 18F-DG PET/CT findings. Local metastasis focus was detected in the liver or lung in 3 cases, and surgical resections were conducted instead of intravenous chemotherapy and biotherapy. Conversely, disseminated metastases were detected in 6 cases, thus intravenous or oral chemotherapy was prescribed instead of surgery. Elevated serum carcinoembryonic antigen (CEA) level was detected in 2 cases while no specific lesion was found, as a result, intravenous chemotherapy was about to be prescribed. With the 18F-DG PET/CT imaging however, the treatment plan was subsequently changed. In one case, PET/CT detected a local recurrence, so a reoperation was preformed in time. In the other case, metastases were detected in both the lung and bone, hence intravenous chemotherapy and local radiotherapy were performed. Second primary cancer was found in another 2 postoperative CRC cases. In one case of colon cancer, 18F-DG PET/CT detected a rectal cancer as the second primary cancer. In the other case, rectal cancer was the first primary cancer while hyper-intensive ileocecal radioactivity was detected in the 18F-DG PET/CT imaging, and colon cancer was confirmed after the reoperation.
Elevated serum CEA level (363.7-863.2 μg/L, average 185.9 μg/L) was found in 24 cases, and recurrence and/or metastasis was detected in 22 of them by 18F-DG PET/CT imaging with specific lesion observed. Diagnoses of recurrence and/or metastasis were confirmed in all of the 22 cases during the clinical follow-up. However, the negative findings of PET/CT in the remained 2 cases were concluded to be false negative in clinical follow-up. Multiple nodi and small metastasis focus were detected in the mesentery and vagina respectively, both with the diameter around 1 cm, and postoperative pathological evidence confirmed the diagnosis of metastasis. As a result, the positive rate of recurrence and/or metastasis detection with PET/CT in postoperative CRC patients with elevated serum CEA levels was 91.7%.
The prognosis of CRC is closely related to the histological type, intestinal wall invasion, malignant lymph node, operation manner and postoperative recurrence and/or metastasis. An emphasis of the postoperative follow-up is the local recurrence and distant metastasis, which could not be detected by traditional imaging techniques such as CR, magnetic resonance imaging (MRI) and ultronography until the lesion reaches a considerable size. Monitoring by tumor markers such as CEA and CA19-9 was not always accurate, and could not provide an orientation indication of the possible lesion either. PET/CT imaging provides whole-body overview at one examination, and could detect abnormal glucose metabolism before the morphological change of a lesion could be identified. Consequently, it has become an efficient and accurate noninvasive examination technique in the postoperative follow-up of CRC[10]. In the present study, PET/CT imaging showed high sensitivity (94.6%), specificity (83.3%) and PPV (96.4%) in the diagnosis of the recurrence and/or metastasis of CRC. These findings are consistent with the Meta-analysis results of Huebner et al[10]. It is suggested that application of PET/CT imaging to detect recurrence and/or metastasis of CRC is appropriate. It is commonly recognized that PET has become en effective technique in detecting postoperative recurrence and/or metastasis of CRC. The sensitivity and specificity reported were over 90% and 70% respectively, both higher than that of traditional imaging techniques.
18F-DG PET/CT imaging is more accurate than traditional imaging in detecting hepatic metastases. Kinkel et al[11] performed a meta-analysis to compare current noninvasive imaging methods in the detection of hepatic metastases from colorectal, gastric, and esophageal cancers. In studies with a specificity higher than 85%, the mean weighted sensitivity was 55% (95% CI: 41, 68) for ultrasonography, 72% (95% CI: 63, 80) for CT, 76% (95% CI: 57, 91) for MRI, and 90% (95% CI: 80, 97) for FDG PET. Thus they demonstrated a greater sensitivity of FDG PET than ultrasonography (P = 0.001), CT (P = 0.017), and also MRI (P = 0.055). Delbeke et al[12] demonstrated in their study on the effect of PET on management that PET helped clarify the final diagnosis misinterpreted on CT and/or CT portography in 28% of the patients (n = 17), leading to a change in surgical management. PET helped to plan surgery in 6 patients by identifying a resectable site of recurrence and helped to avoid unnecessary surgery in 11 patients by identifying unresectable disease.
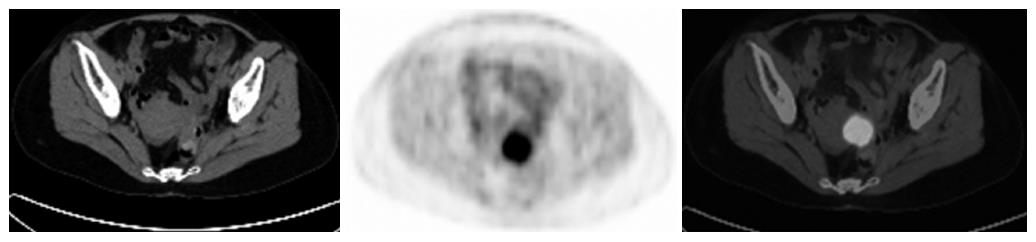
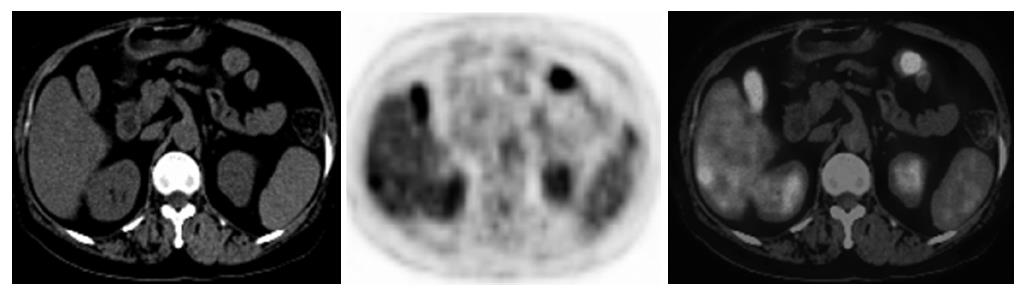
In our study, PET/CT imaging detected one or more occult malignant lesions in 8 cases where abdominal/pelvic CT and/or ultrasonography showed negative findings, resulting in altered clinical staging. PET/CT imaging also detected more lesions than CT and ultrasonography did in 30.4 % (17/56) cases, showing disseminated metastases and hence resulting in altered clinical treatment plans. PET/CT imaging increases the accuracy and certainty of locating lesions in colorectal cancer. The fused imaging of PET and CT is especially important for identifying lesions in abdominal and pelvic cavity. PET itself is insufficient to identify anatomic structures clearly and also incapable to interpret the nonspecific uptake of the gastrointestinal and muscles and the execration of the urinary system. CT provides an attenuation correction, and its morphologic imaging is helpful to differentiate among physiological uptake, anastomosis inflammation, and the cancer recurrence. It also helps to detect tumors which showed a negative uptake of 18F-DG in PET imaging. Cohade et al[13] compared the diagnostic roles of 18F-FDG PET and PET/CT in a population of patients with colorectal cancer. The frequency of equivocal and probable lesion characterization was reduced by 50% (50 to 25) with PET/CT, in comparison with PET. The frequency of definite lesion characterization was increased by 30% (84 to 109) with PET/CT. The number of definite locations was increased by 25% (92 to 115) with PET/CT. Overall correct staging increased from 78% to 89% with PET/CT on a patient-by-patient analysis. Our study also shows the superiority of combined PET and CT imaging in detecting recurrent and isolated hepatic metastasis of CRC (Figures 1 and 2).
When local recurrence and/or distant metastasis are diagnosed and the reoperation is planned, PET/CT imaging is greatly helpful in preoperative staging and evaluating the feasibility of the operation. It could detect the unresectable and additional occult lesions, and thus avoid unnecessary surgical resections and also economic expenditures. It could also provide further information regarding the surgical resection details based on the imaging findings in those cases which reoperation is needed. A better decision of clinical management based on preoperative PET/CT imaging results in better clinical outcome. Zubeldia et al[14] concluded that integration of FDG-PET into the presurgical evaluation of patients with hepatic metastases could substantially reduce overall costs and patients’ morbidity. This substantial net saving, 5269 dollars averagely, results from the unique ability of FDG-PET in excluding patients with extrahepatic disease, and avoiding unnecessary surgical expenses. In our study, unnecessary surgeries were avoided in 7 cases where multiple distant metastases were found in PET/CT imaging, accounting for 70% (7/10) of the cases where reoperation was planned before PET/CT imaging. These imaging findings directly resulted in decreased medical expenses. In those cases with elevated serum CEA levels, PET/CT is helpful in detecting recurrence and/or metastasis based on both functional and morphological imaging. In the study of Shen et al[15], whole-body FDG-PET was performed in 50 patients suspected of having recurrent colorectal cancer and asymptomatically increased serum level of CEA (> 5 μg/L), and the final diagnosis of recurrent colorectal cancer was established in 64 lesions of 45 patients. The diagnostic sensitivity and positive predictive value of FDG-PET was 95.3% on a patient-based analysis, and 96.9% on a lesion-based analysis. In our study, PET/CT detected one or more possibly malignant lesions in 91.7% (22/24) postoperative CRC patients with increased serum level of CEA. It was obvious that PET/CT is clinically significant in the detection of postoperative malignant lesions in CRC patients.
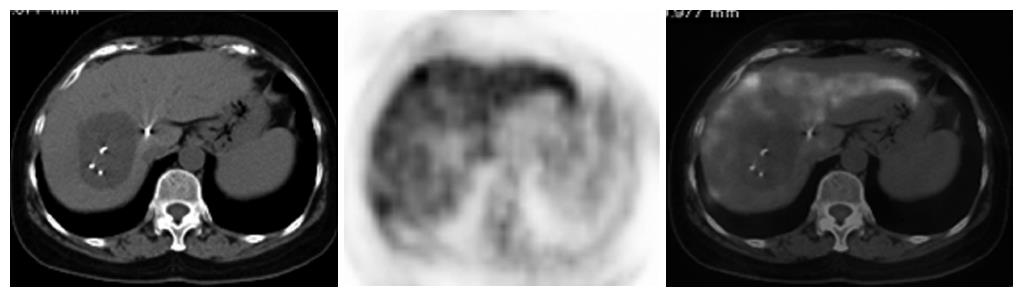
PET/CT could also be used in monitoring the treatment effect of local therapy of isolated liver and lung metastatic lesions. Local therapy approaches of hepatic metastasis include selective transcatheter arterial chemoembolization (TACE), radio frequency ablation (RFA), Argon-Helium cryoablation, gamma knife radiosurgery (GKS), 125I seeds brachytherapy, and so on. Traditional imaging techniques could not discriminate between tissue edema and tumor remnant, and could not exclude the interference of iodinated oil retention either. By contrast, PET provides a functional imaging of the metabolism levels within the suspected foci and also the whole-body, so it substantially helps the clinicians in recognizing tumor remnants and evaluating whole-body status, which are crucial in making treatment decisions. In our study, 7 patients underwent local therapy of isolated liver or lung metastasis. Figure 3 shows the typical PET/CT imaging of one case underwent 125I seeds brachytherapy of the localized hepatic metastasis.
In conclusion, our study demonstrated the superiority of 18F-DG PET/CT in the imaging diagnosis of postoperative recurrence and/or metastasis of CRC. It could detect not only recurrent tumor and/or occult metastasis in early stage, but also any other lesions showing abnormal metabolism level within the whole-body of postoperative CRC patients. The PPV was 96.4% and the negative NPV was 76.9%. The major causes of false positive were granulomatous inflammation at the anastomosis and inflammatory lymph node, while those of false negative were small lesion sizes (usually less than 1 cm in diameter). As a result, interpretation of 18F-DG PET/CT imaging should also be based on clinical findings in order to minimize the chance of misdiagnose.
Combined positron emission tomography and copmputed tomography (PET/CT) is currently widely used in clinical diagnosis of cancer, however, the value of PET/CT in detection of recurrence and/or metastasis of colorectal cancer (CRC) remains to be confirmed furtherly.
In the area of application of PET/CT in CRC, the research hotspot is to evaluate the value of this technique in pre-surgery staging, predicting therapy effects and detecting postoperative recurrence and/or metastasis of the disease.
In the present study, recurrence and/or metastasis were confirmed in 56 patients in the clinical follow-up after the PET/CT imaging. The sensitivity of PET/CT diagnosis of CRC recurrence and/or metastasis was 94.6%, and the specificity was 83.3%. The positive predictive value (PPV) was 96.4% and the negative predictive value (NPV) was 76.9%. PET/CT imaging detected one or more occult malignant lesions in 8 cases where abdominal/pelvic CT and/or ultrasonography showed negative findings, and also detected more lesions than CT or ultrasonography did in 30.4% (17/56) cases. Recurrence and/or metastasis was detected in 91.7% (22/24) cases with elevated serum CEA levels by 18F-DG PET/CT imaging.
18F-DG PET/CT imaging is a useful technique for detecting recurrence and/or metastasis of CRC with high sensitivity and specificity. It could detect not only recurrent tumor and/or occult metastasis in early stage, but also any other lesions showing abnormal metabolism level within the whole-body of postoperative CRC patients.
PET/CT: Combined the technologies of positron emission tomography and spiral copmputed tomography into a highly sensitive and quantitative molecular imaging modality. The “fused” image of PET and CT scan can provide complete information on the location, nature and extent of lesions.
This is a good article in which authors demonstrated the superiority of 18F-DG PET/CT in the imaging diagnosis of postoperative recurrence and/or metastasis of CRC by conducting a retrospective study of 68 patients. The result is valuable for choice of imaging techniques for detecting recurrence and/or metastasis of CRC.
S- Editor Ma N L- Editor Rampone B E- Editor Wang HF
| 1. | Lv W, Zhang C, Hao J. RNAi technology: a revolutionary tool for the colorectal cancer therapeutics. World J Gastroenterol. 2006;12:4636-4639. [PubMed] |
| 2. | Wang XL, Yuan Y, Zhang SZ, Cai SR, Huang YQ, Jiang Q, Zheng S. Clinical and genetic characteristics of Chinese hereditary nonpolyposis colorectal cancer families. World J Gastroenterol. 2006;12:4074-4077. [PubMed] |
| 3. | Benson AB. The hope for today--the promise for tomorrow: will oncologists meet the challenge? J Clin Oncol. 2007;25:2156-2158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Desch CE, Benson AB, Somerfield MR, Flynn PJ, Krause C, Loprinzi CL, Minsky BD, Pfister DG, Virgo KS, Petrelli NJ. Colorectal cancer surveillance: 2005 update of an American Society of Clinical Oncology practice guideline. J Clin Oncol. 2005;23:8512-8519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 391] [Cited by in RCA: 381] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 5. | Ariyan CE, Salem RR. Evolution in the treatment of metastatic colorectal carcinoma of the liver. World J Gastroenterol. 2006;12:3253-3258. [PubMed] |
| 6. | Fernandes LC, Kim SB, Saad SS, Matos D. Value of carcinoembryonic antigen and cytokeratins for the detection of recurrent disease following curative resection of colorectal cancer. World J Gastroenterol. 2006;12:3891-3894. [PubMed] |
| 7. | Jadvar H, Henderson RW, Conti PS. 2-deoxy-2-[F-18]fluoro-D-glucose-positron emission tomography/computed tomography imaging evaluation of esophageal cancer. Mol Imaging Biol. 2006;8:193-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Mochiki E, Kuwano H, Katoh H, Asao T, Oriuchi N, Endo K. Evaluation of 18F-2-deoxy-2-fluoro-D-glucose positron emission tomography for gastric cancer. World J Surg. 2004;28:247-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 171] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 9. | Gearhart SL, Frassica D, Rosen R, Choti M, Schulick R, Wahl R. Improved staging with pretreatment positron emission tomography/computed tomography in low rectal cancer. Ann Surg Oncol. 2006;13:397-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 111] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 10. | Huebner RH, Park KC, Shepherd JE, Schwimmer J, Czernin J, Phelps ME, Gambhir SS. A meta-analysis of the literature for whole-body FDG PET detection of recurrent colorectal cancer. J Nucl Med. 2000;41:1177-1189. [PubMed] |
| 11. | Kinkel K, Lu Y, Both M, Warren RS, Thoeni RF. Detection of hepatic metastases from cancers of the gastrointestinal tract by using noninvasive imaging methods (US, CT, MR imaging, PET): a meta-analysis. Radiology. 2002;224:748-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 436] [Cited by in RCA: 363] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 12. | Delbeke D, Vitola JV, Sandler MP, Arildsen RC, Powers TA, Wright JK, Chapman WC, Pinson CW. Staging recurrent metastatic colorectal carcinoma with PET. J Nucl Med. 1997;38:1196-1201. [PubMed] |
| 13. | Cohade C, Osman M, Leal J, Wahl RL. Direct comparison of (18)F-FDG PET and PET/CT in patients with colorectal carcinoma. J Nucl Med. 2003;44:1797-1803. [PubMed] |
| 14. | Zubeldia JM, Bednarczyk EM, Baker JG, Nabi HA. The economic impact of 18FDG positron emission tomography in the surgical management of colorectal cancer with hepatic metastases. Cancer Biother Radiopharm. 2005;20:450-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Shen YY, Liang JA, Chen YK, Tsai CY, Kao CH. Clinical impact of 18F-FDG-PET in the suspicion of recurrent colorectal cancer based on asymptomatically elevated serum level of carcinoembryonic antigen (CEA) in Taiwan. Hepatogastroenterology. 2006;53:348-350. [PubMed] |