Published online Sep 14, 2007. doi: 10.3748/wjg.v13.i34.4574
Revised: March 30, 2007
Accepted: March 31, 2007
Published online: September 14, 2007
AIM: To evaluate whether a higher prevalence of Giardia lamblia infection is associated with an increase in irritable bowel syndrome (IBS) prescriptions at the county level in Michigan.
METHODS: The Michigan Disease Surveillance System (MDSS) was used to ascertain both the numbers of Giardia lamblia infections as well as the total number of foodborne illnesses per population by county in Michigan during 2005. This was compared with Blue Cross Blue Shield (BCBS) of Michigan numbers of drug prescriptions for IBS per one thousand members per county in 2005. These data were also analyzed for associations with per capita income by county and the number of refugees entering each county in 2005.
RESULTS: There were a total of 786 confirmed cases of Giardia lamblia reported to MDSS in 2005. During the same time period, the number of prescriptions for IBS varied from 0.5 per 1000 members up to 6.0 per 1000 members per month. There was no trend towards higher numbers of IBS prescriptions in the counties with more Giardia lamblia infections. Per capita income was not associated with either IBS prescriptions or Giardiasis. There was a significant linear association between the number of refugees entering each county, and the number of Giardia lamblia cases per 100 000 population.
CONCLUSION: In this ecological study, there was no association found between BCBS prescriptions for IBS and Giardia lamblia infections in Michigan counties. Our findings may have been influenced by the disparate number of refugees admitted per county.
-
Citation: Penrose AS, Wells EV, Aiello AE. Infectious causation of chronic disease: Examining the relationship between
Giardia lamblia infection and irritable bowel syndrome. World J Gastroenterol 2007; 13(34): 4574-4578 - URL: https://www.wjgnet.com/1007-9327/full/v13/i34/4574.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i34.4574
Giardia lamblia is a multi-flagellate protozoa which can cause symptoms of abdominal discomfort, bloating, diarrhea and mucus, but not blood in the stools[1]. The cyst form is resistant to cold weather and chlorination[2]. It is spread by the fecal-oral route, and is most commonly diagnosed in young children, especially in day-care centers, where the prevalence has been found to be as high as 35%[1]. The incidence is also increased in men who have sex with men, and in immigrants from developing countries[3]. The FDA (Food and Drug Administration) estimates a probable 2% annual Giardiasis attack rate in the United States (US) population[4] although substantially fewer infections are diagnosed. The Center for Disease Control (CDC) recorded 18 126 infections in 2005 in the US as a whole[5], for an incidence of approximately 0.006%. This would imply that the vast majority of infections are asymptomatic, symptomatic but not brought to the attention of the medical community, or symptomatic and misdiagnosed.
Irritable bowel syndrome (IBS) is a diagnosis of exclusion. The Rome criteria specify three months of abdominal discomfort, unrelated to a physiologic or biologic cause, which can be associated with bloating, constipation, diarrhea or mucus[6]. These symptoms overlap with many other gastrointestinal illnesses, such as inflammatory bowel disease, lactose intolerance, gastrointestinal cancers and parasitic diseases[6], including Giardiasis, which also can become chronic.
By definition, patients with IBS do not have a physiologic cause for their illness, but some studies have shown that a significant number of patients who have been given the diagnosis of IBS do indeed have infection with Giardia lamblia[7-9]. Likewise, a study of 100 consecutive patients in an outbreak of Giardiasis in Italy found that 82% of these patients met the Rome criteria for IBS, including the chronicity of symptoms[10]. Other authors have described a syndrome of post-infectious IBS due to either bacterial or parasitic etiologies[11,12]. Recent research has shown a similar association between the initiation of celiac disease, and the number of previous rotavirus infections in children[13]. Further evidence of a possible connection between parasitic disease and IBS is that treatment with metronidazole, an anti-parasitic medication, has been shown to decrease symptoms of IBS[14-16].
The current study was undertaken to determine whether there might be a causal relationship between current or past Giardia lamblia infection and the prevalence of IBS. To test this, we assessed whether a higher county level prevalence of IBS prescriptions is associated with a higher incidence of Giardia lamblia infections in Michigan counties.
Michigan initiated an electronic surveillance system for communicable diseases in 2004, called the Michigan Disease Surveillance System (MDSS). Local health departments, the Michigan Bureau of Laboratories, and some of the larger private laboratories enter data directly into the system over the internet. Giardiasis is a reportable disease in Michigan, and the local health departments use MDSS to track their cases. This system ensures that MDSS captures all of the reported cases of Giardia lamblia in Michigan. The aggregate information is made available to the CDC, as well as to the local health departments. The number of cases can be analyzed by time, demographics and geographic location. The date of onset of illness was used for inclusion when available, and the date of referral was used when date of onset was not known. Only the confirmed, completed cases in 2005 were counted. The rate per 100 000 people was obtained by dividing the number of cases per county, by population in each county, obtained from the 2005 United States census estimates.
Blue Cross Blue Shield (BCBS) of Michigan maintains a record of all prescriptions filled for its members, which includes the address and county of each member. Information on the number of members over a particular time period is also available, broken down by county. This was used to obtain a rate of prescriptions per 1000 members per month in 2005. Three medications were included in this study, dicyclomine (Bentyl), tegaserod (Zelnorm) and alosetron (Lotronex). These three medications were chosen because their only approved indication is the treatment of IBS. Prescription information was used in lieu of IBS diagnoses because there is no current registry of IBS patients in Michigan.
Per capita income data were obtained from the US census for 2000. Refugee numbers were provided by the Office of Refugee Services of the Michigan Department of Human Services.
A database was constructed containing information on Giardia lamblia cases by county. This was linked with information on the population of each county, to obtain a rate per 100 000 people. Next, the IBS prescription rates by county were added to the database, followed by per capita income and numbers of refugees admitted. Finally, the rate of foodborne illness by county was placed in the database, which was then cleaned and coded.
Descriptive statistics were used to assess frequencies and distributions of variables. Univariate regression was performed to assess relationships between IBS prescriptions and foodborne illness, IBS prescriptions and per capita income, and between Giardia lamblia and IBS prescriptions, refugees, foodborne illness, and per capita income. SPSS version 11.5 was used for all data analyses.
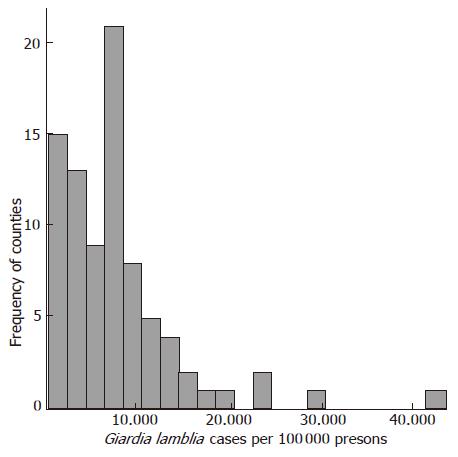
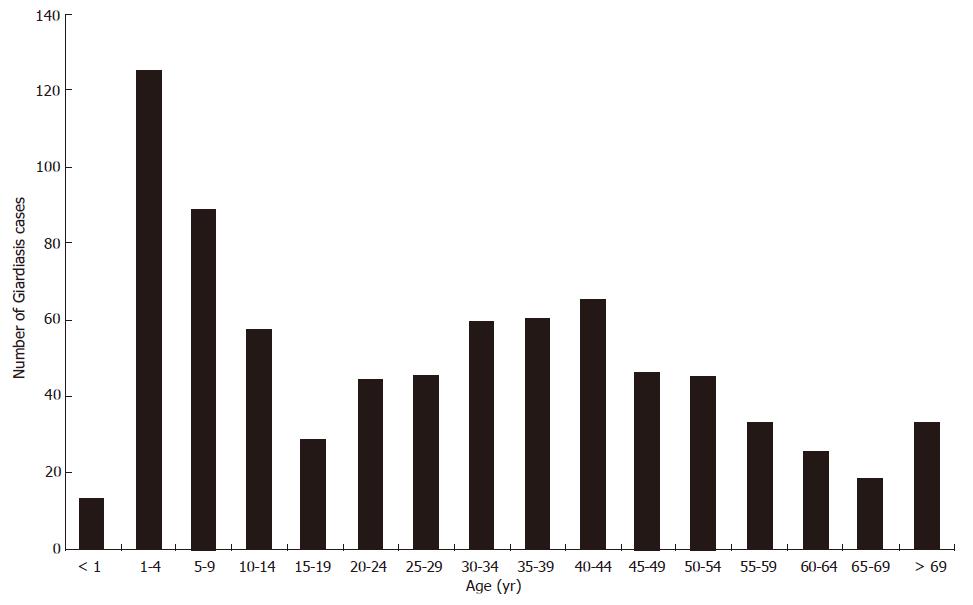
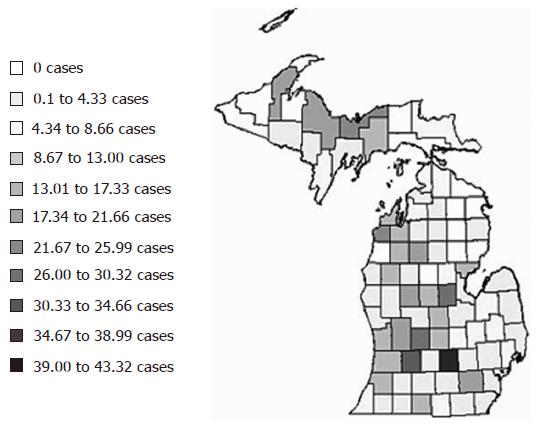
The total number of Giardia lamblia cases in Michigan, which has 83 counties, was 786 in 2005, which was down from 980 in 2000, but up from 733 in 2004, the year MDSS was introduced. Ingham County had 121 cases of Giardiasis in 2005, which gave it the highest incidence of 0.043%, which is about seven times the national average. Fourteen counties had no cases reported in 2005. The mean number of cases per county was 9.6, and the median was 3. The graph of incidence for each county by frequency was right-skewed (Figure 1). There were 362 (46%) female cases and 420 (53%) male cases with 4 unknown. One hundred and thirty-eight cases were children ≤ 4 years, and 89 were children between 5 and 9 years, for a total of 227 (29%) of the cases. There was another spike between ages 30 and 44 with a total of 184 (23%) cases. The number of cases gradually decreased after age 44 (Figure 2). The majority (51%) of cases were among 402 European Americans, with only 57 (7%) African Americans, 31 (4%) Asian Americans and 3 (< 1%) Native Americans. Race was not specified for 293 (37%) cases. Of the 393 whose ethnicity was known, 37 (9%) were Latino, and 356 (91%) were non-Latino.
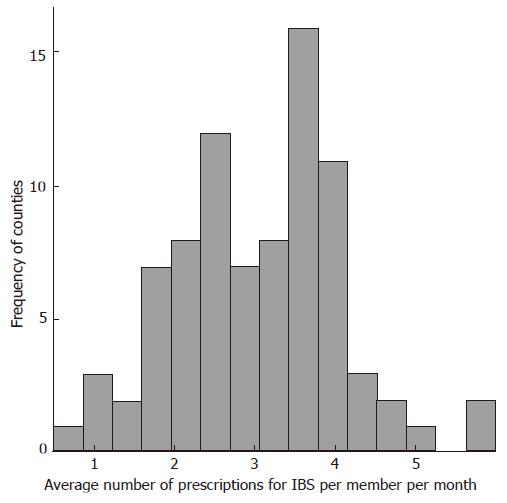
The number of BCBS prescriptions for IBS per 1000 members per month in 2005 was much less variable between counties. It ranged between 0.5 and 6.0, with a statewide total average of 3.3 (Figure 3). All six of the counties with rates above 4.3 were in the BCBS “western” region, and four of those counties were contiguous. There was no linear association between IBS prescriptions and per capita income by county.
There were 868 refugees admitted to Michigan in 2005. Of those, 342 were from Africa, 187 from the former Soviet Union, 167 from East Asia, 93 from the Middle East, 67 from Cuba, and 14 from Bosnia. Ingham County accepted 349 (40%) refugees. Thirteen other counties accepted at least one refugee. Sixty-nine counties did not receive any refugees that year. Of the nine counties that took at least 10 refugees, the number of Giardia lamblia cases ranged from 7 to 121, and the incidence was between 0.003% and 0.043% (Table 1).
| County | Giardia lamblia cases | Incidence per100 000 | Refugeesadmitted |
| Calhoun | 7 | 5 | 12 |
| Genesse | 12 | 3 | 45 |
| Ingham | 121 | 43 | 349 |
| Kent | 86 | 15 | 236 |
| Macomb | 32 | 4 | 17 |
| Oakland | 72 | 6 | 117 |
| Saginaw | 15 | 7 | 11 |
| Saint Clair | 14 | 9 | 10 |
| Wayne | 77 | 4 | 53 |
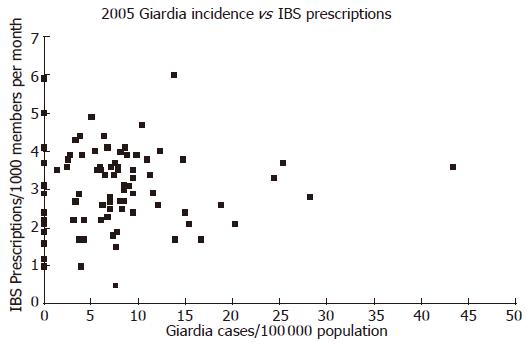
Graphing the number of Giardia lamblia infections versus the number of IBS prescriptions revealed no linear relationship (Figure 4). The simple linear regression estimate provided an R-square of 0.001. Similarly, looking at total foodborne illness versus IBS prescriptions, no significant linear association was seen.
Per capita income was not significantly linearly associated with either Giardiasis or IBS prescriptions. The number of refugees admitted did show an association with the incidence of Giardia lamblia by county in 2005 (R-square = 0.221, P < 0.001).
This study examined the evidence for an association between the parasite Giardia lamblia and IBS, but found none. This lack of association is contrary to multiple previous studies linking acute infectious gastroenteritis with IBS and is therefore notable. There were 786 cases of Giardiasis reported in Michigan in 2005, which is a rate of 7.8 per 100 000 people. In comparison, in 2005, Ohio had a rate of 7.1, and Wisconsin had 13.0 per 100 000[5]. The rate of cases among different counties in Michigan varied from zero up to 43 per 100 000 (Figure 5). In the US as a whole, the incidence in 2005 was 6.1 per 100 000 people[5]. Ingham County had the highest activity in Michigan, and also the highest number of refugees admitted in 2005, when it received 349 of the 868 total refuges that entered the state (Personal communication, Al Horn, Director of the Office of Refugee Services of the Michigan Department of Human Services). There was a positive linear association between the incidence of Giardiasis by county and the number of refugees admitted in 2005 (P < 0.001). This supports the previously described increased risk of Giardiasis in immigrants from developing countries[3].
Previous studies have posited a causal link between Giardia lamblia and IBS through inflammation of the mucosal lining of the gut[10,12]. Giardia lamblia is also known to cause dissacharide intolerance for up to 6 mo after infection[4]. This increases intestinal gas, causing painful distention of the colon, which could be misdiagnosed as IBS. These theoretical mechanisms need not be restricted to Giardia lamblia. Other parasites have been studied in relation to IBS, including Entamoeba histolytica[17], Dientamoeba fragilis[18], and Blastocystis hominis[19-21], but none of these are reportable diseases in Michigan. Likewise acute bacterial gastroenteritis epidemics with Salmonella enteritidis, Escherichia coli, and Campylobacter jejuni have been shown to increase subsequent levels of IBS in those populations exposed[22,23]. It might be expected, however, that Giardiasis alone, or foodborne illnesses in total, could act as a proxy for the myriad of parasitic and bacterial illnesses which are associated with IBS, since conditions which lead to high prevalence of one foodborne illness are likely to lead to increases in others as well. This study does not support such an association between Giardia lamblia, or foodborne illness in general, and IBS. It is possible that this lack of association is due to the relationship between high refugee numbers and the incidence of Giardia lamblia in Michigan. The refugee population may not have full access to regular health care, and so may be unlikely to receive a diagnosis of IBS, even if they meet the diagnostic criteria. There may also be a lag time between the onset of IBS and the use of disease-specific medication, and if this is true, then the large influx of refugees with Giardiais in 2005 might not show up as an increase in IBS prescriptions until 2006 or later.
One limitation of this study is that BCBS prescription numbers may not accurately define the prevalence of IBS, nor do they distinguish between recent onset IBS and chronic disease. Also, although Giardiasis is a reportable disease, the collection of cases is by passive and not active surveillance, and the percentage of infections diagnosed and reported may vary greatly between counties. It seems reasonable, however, that these under-estimates in prevalence of IBS and incidence of Giardia might average out over the state as a whole. Finally, the 2005 Michigan population data, used to determine incidence, was necessarily an estimate, since the US census is only done every ten years. Despite these limitations, this ecological study is a first step in attempting to go beyond case reports and small clinical studies to define the true association between a parasite and IBS.
The lack of a known etiologic factor for IBS, the similarity of symptoms between IBS and Giardiasis, and the large number of undiagnosed Giardia lamblia infections make it tempting to look for a causal link between these two diseases, but at present, there is not enough evidence to prove one exists. Prospective studies, in a young, healthy, population at risk for IBS, with routine examination of stools for parasites, and collection of IBS symptom data, would make a tremendous contribution in this area.
This article concerns the possible link between an acute parasitic illness, Giardia lamblia, and subsequent development of a chronic disease, irritable bowel syndrome (IBS). Giardia is a common parasite, transmitted through ingestion of the cyst form, which causes symptoms of diarrhea, bloating, mucus and abdominal discomfort in its victims.
Previous research has suggested associations of Giardia, other parasites, and some bacteria, with IBS. Mearin et al (Gastroenterology 2005; 129: 98-104) found a relative risk of IBS at one year after acute infection with Salmonella enteritidis to be 7.8 times that of the unexposed population. Two or three years after presumed infection with Escherichia coli 0157:H7 or Campylobacter jejuni gastroenteritis, Marshall et al (Gastroenterology 2006; 131: 445-450) found a rate of IBS 4.8 higher than expected. An earlier study of newly diagnosed Giardia cases in Italy by D'Anchino, Orlando and DeFeudis (Journal of Infection 2002; 45:169-172) noted that 82% of the patients had had at least six months of IBS symptoms before Giardia was diagnosed, suggesting that IBS predisposes patients to being symptomatic during Giardia infestation, and not that Giardia causes IBS. Whether Giardia and other intestinal infections actually cause IBS, or whether patients with IBS are simply more likely to be symptomatic during episodes of gastrointestinal infection has important implications for the diagnosis and treatment of IBS.
This study looked at rates of prevalence of IBS by county in Michigan, and compared that to incidence of newly diagnosed Giardia cases. No association was found, which implies that Giardia does not cause a significant number of cases of IBS.
This is an important and interesting topic but were concerned that the ecological methodology of the study made the conclusions weaker than they would otherwise be.
S- Editor Liu Y L- Editor Kumar M E- Editor Yin DH
| 1. | Ortega YR, Adam RD. Giardia: overview and update. Clin Infect Dis. 1997;25:545-549; quiz 550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 133] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Kucik CJ, Martin GL, Sortor BV. Common intestinal parasites. Am Fam Physician. 2004;69:1161-1168. [PubMed] |
| 3. | Hlavsa MC, Watson JC, Beach MJ. Giardiasis surveillance--United States, 1998-2002. MMWR Surveill Summ. 2005;54:9-16. [PubMed] |
| 5. | CDC . Notifiable diseases/deaths in selected cities weekly information. Morbidity and Mortality Weekly Report. 2006;45:1320-1330. |
| 6. | Feldman M, Scharschmidt BF, Sleisenger MH. Gastroinestinal and liver disease. 6th ed. Philadelphia: WB Saunders Company 1998; 1537. |
| 7. | Bujanda L, Gutiérrez-Stampa MA, Caballeros CH, Alkiza ME. Gastrointestinal disorders in Guatemala and their relation with parasitic infections. An Med Interna. 2002;19:179-182. [PubMed] |
| 8. | Grazioli B, Matera G, Laratta C, Schipani G, Guarnieri G, Spiniello E, Imeneo M, Amorosi A, Focà A, Luzza F. Giardia lamblia infection in patients with irritable bowel syndrome and dyspepsia: a prospective study. World J Gastroenterol. 2006;12:1941-1944. [PubMed] |
| 9. | Sánchez RC, Navarro Cano G. Diagnostic value of limited research in patients with irritable bowel syndrome. Rev Gastroenterol Mex. 2004;69:24-29. [PubMed] |
| 10. | D'Anchino M, Orlando D, De Feudis L. Giardia lamblia infections become clinically evident by eliciting symptoms of irritable bowel syndrome. J Infect. 2002;45:169-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Stermer E, Lubezky A, Potasman I, Paster E, Lavy A. Is traveler's diarrhea a significant risk factor for the development of irritable bowel syndrome? A prospective study. Clin Infect Dis. 2006;43:898-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 79] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 12. | Gómez-Escudero O, Schmulson-Wasserman MJ, Valdovinos-Díaz MA. Post-infectious irritable bowel syndrome. A review based on current evidence. Rev Gastroenterol Mex. 2003;68:55-61. [PubMed] |
| 13. | Stene LC, Honeyman MC, Hoffenberg EJ, Haas JE, Sokol RJ, Emery L, Taki I, Norris JM, Erlich HA, Eisenbarth GS. Rotavirus infection frequency and risk of celiac disease autoimmunity in early childhood: a longitudinal study. Am J Gastroenterol. 2006;101:2333-2340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 359] [Cited by in RCA: 371] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 14. | Nayak AK, Karnad DR, Abraham P, Mistry FP. Metronidazole relieves symptoms in irritable bowel syndrome: the confusion with so-called 'chronic amebiasis'. Indian J Gastroenterol. 1997;16:137-139. [PubMed] |
| 15. | Dear KL, Elia M, Hunter JO. Do interventions which reduce colonic bacterial fermentation improve symptoms of irritable bowel syndrome? Dig Dis Sci. 2005;50:758-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 63] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 16. | Bolin TD, Davis AE, Duncombe VM. A prospective study of persistent diarrhoea. Aust N Z J Med. 1982;12:22-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Sinha P, Ghoshal UC, Choudhuri G, Naik S, Ayyagari A, Naik SR. Does Entamoeba histolytica cause irritable bowel syndrome? Indian J Gastroenterol. 1997;16:130-133. [PubMed] |
| 18. | Lagacé-Wiens PR, VanCaeseele PG, Koschik C. Dientamoeba fragilis: an emerging role in intestinal disease. CMAJ. 2006;175:468-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Giacometti A, Cirioni O, Fiorentini A, Fortuna M, Scalise G. Irritable bowel syndrome in patients with Blastocystis hominis infection. Eur J Clin Microbiol Infect Dis. 1999;18:436-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 61] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Hussain R, Jaferi W, Zuberi S, Baqai R, Abrar N, Ahmed A, Zaman V. Significantly increased IgG2 subclass antibody levels to Blastocystis hominis in patients with irritable bowel syndrome. Am J Trop Med Hyg. 1997;56:301-306. [PubMed] |
| 21. | Yakoob J, Jafri W, Jafri N, Islam M, Asim Beg M. In vitro susceptibility of Blastocystis hominis isolated from patients with irritable bowel syndrome. Br J Biomed Sci. 2004;61:75-77. [PubMed] |
| 22. | Marshall JK, Thabane M, Garg AX, Clark WF, Salvadori M, Collins SM. Incidence and epidemiology of irritable bowel syndrome after a large waterborne outbreak of bacterial dysentery. Gastroenterology. 2006;131:445-450; quiz 660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 228] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 23. | Mearin F, Pérez-Oliveras M, Perelló A, Vinyet J, Ibañez A, Coderch J, Perona M. Dyspepsia and irritable bowel syndrome after a Salmonella gastroenteritis outbreak: one-year follow-up cohort study. Gastroenterology. 2005;129:98-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 289] [Cited by in RCA: 265] [Article Influence: 13.3] [Reference Citation Analysis (0)] |