Published online Aug 7, 2007. doi: 10.3748/wjg.v13.i29.3981
Revised: May 1, 2007
Accepted: May 12, 2007
Published online: August 7, 2007
AIM: To evaluate the effectiveness of endoscopic submucosal dissection using an insulation-tipped diathermic knife (IT-ESD) for the treatment of patients with over 20 mm early gastric cancer (EGC).
METHODS: A total of 112 patients with over 10 mm EGC were treated with IT-ESD at Sumitomo Besshi Hospital and Shikoku Cancer Center in the 5 year period from January 2002 to December 2006, including 40 patients with over 20 mm EGC. We compared patient backgrounds, the one-piece resection rate, complete resection (CR) rate, operation time, bleeding rate, perforation rate between patients with over 20 mm EGC [over 20 mm group (21-40 mm)] and the remaining patients (under 20 mm group).
RESULTS: We found no significant difference in the rate of underlying cardiopulmonary disease (over 20 mm group vs under 20 mm group, 5.0% vs 5.6%), one-piece resection rate (95% vs 96%), CR rate (85% vs 89%), operation time (72.3 min vs 66.5 min), bleeding rate (5% vs 4.2%), and perforation rate (0% vs 1.4%) between the 2 groups. Three patients in each group had submucosal invasion and two in each groups underwent additional surgery.
CONCLUSION: There was no significant difference in the outcome resulting from IT-ESD between the 2 groups. Our study proves that IT-ESD is a feasible treatment for patients with over 20 mm mucosal gastric cancer although the long-term outcome should be evaluated in the future.
- Citation: Hirasaki S, Kanzaki H, Matsubara M, Fujita K, Ikeda F, Taniguchi H, Yumoto E, Suzuki S. Treatment of over 20 mm gastric cancer by endoscopic submucosal dissection using an insulation-tipped diathermic knife. World J Gastroenterol 2007; 13(29): 3981-3984
- URL: https://www.wjgnet.com/1007-9327/full/v13/i29/3981.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i29.3981
Endoscopic mucosal resection (EMR) of early gastric cancer (EGC) is effective for the treatment of mucosal malignancies, but one-piece resection is often not achieved by conventional EMR[1]. Endoscopic submucosal dissection (ESD) techniques using a variety of knives, such as the insulation-tipped diathermic knife (IT-knife), hook knife or flex knife, have been developed in Japan[2,3] and high one-piece resection rates have been reported[1,3]. Recently, expanded criteria for ESD have been proposed and many patients with over 20 mm EGC undergo ESD in clinical research in Japan. The purpose of this study was to evaluate the effectiveness of ESD using an insulation-tipped diathermic knife (IT-ESD) for patients with over 20 mm EGC.
We retrospectively reviewed the records of patients admitted to Sumitomo Besshi Hospital and Shikoku Cancer Center with gastric cancer between January 2002 and December 2006. Patients admitted during this period were divided into an over 20 mm group (21-40 mm) and an under 20 mm group (11-20 mm) according to the size of the tumor. Patients whose tumor sizes were 20 mm were included in the under 20 mm group. Patients backgrounds, the one-piece resection rate, complete resection (CR) rate, operation times, bleeding rate, and perforation rate were compared among the groups. We had already treated more than 100 EGC patients (10 mm or less) with IT-ESD; however, they were excluded from this study, because small tumors could be completely removed by conventional EMR method. Patients with severe underlying disease such as heart disease, respiratory disease, liver disease, or bleeding tendency were excluded from the indication of ESD in our institute; however, those severe underlying diseases have not been observed in patients included in this study. Patients taking drugs to promote bleeding such as ticlopidine, aspirin or warfarin underwent ESD after a definite term of drug discontinuance. All patients fulfilled the following criteria: (1) diagnosed with mucosal gastric carcinoma by endoscopic findings or endoscopic ultrasonography, (2) had a biopsy specimen obtained from the lesion that revealed differentiated adenocarcinoma, (3) did not have ulceration of the lesion, and (4) the diameter of their lesion was 40 mm or less. No patients with aforementioned conditions who underwent endoscopic therapy other than ESD such as laser therapy were included. In our institute, if the size of the mucosal cancer is over 20 mm up to 40 mm in diameter, the patient can undergo ESD if they wish. The performance status (PS) of each patient was less than 2 on the Eastern Cooperative Oncology Group (ECOG) scale. IT-ESD was performed under informed consent. Two highly skilled endoscopists familiar with ESD performed IT-ESD in this study.
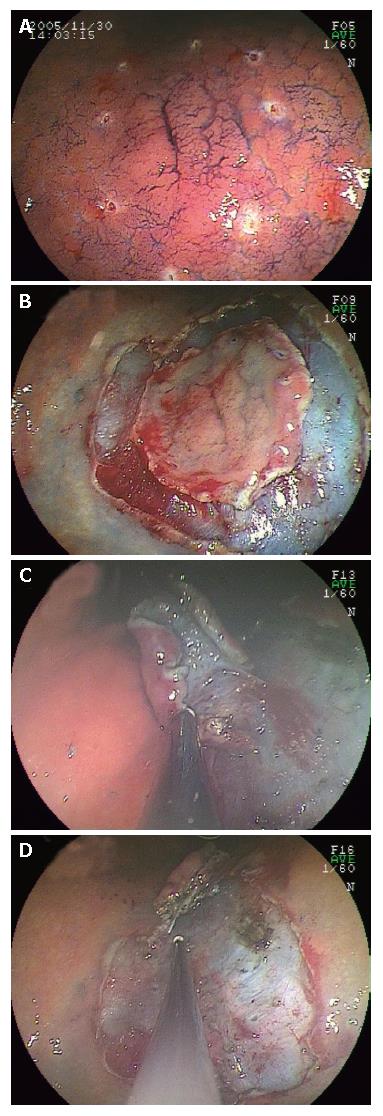
IT-ESD was performed as we previously described[3,4]: (1) marks were made at several points along the outline of the lesion with a coagulation current, using a marking tip (Type KD-1L; Olympus) (Figure 1A), (2) an injection of 20 mL of saline containing 0.0025% epinephrine was carried out just outside the marks to prevent perforation until the mucosa around the lesion was raised, (3) a hole (about 2 mm) for inserting the ceramic ball of the IT-knife into the submucosal layer was made with hot biopsy forceps on the raised mucosa, (4) starting from the hole made by the hot biopsy forceps, the mucosa just outside the marks with the IT-knife was incised, (5) after completion of the IT-knife cut around the lesion with a safe lateral margin (Figure 1B), the submucosal tissue under the circumcised area was abraded with it (Figure 1C), (6) as the abrasion made progress, the circumcised area shrank gradually, (7) the specimen was then either completely resected using the IT-knife (Figure 1D), or finally removed using a conventional polypectomy snare if it was attached only to a pedicle. In more than half of the patients in this study, we removed the lesions with an IT-knife and without using snaring.
A gastrointestinal pathologist evaluated the ESD specimens with special attention to the depth of tumor invasion and the lateral and deep margins of the excision. Resected specimens were cut into 2 mm slices according to the Japanese Classification of Gastric Carcinoma[5] and evaluated as to whether cancerous glands were present or absent at the margin of each slice.
Patients in this study were managed according to the clinical pathway that we previously reported[3]. Patients underwent follow-up endoscopic examination the following morning to prevent delayed bleeding.
When one-piece resection could be performed, it was easy to evaluate the completeness of the resection histologically. The efficacy of resection was determined according to the completeness of the resection: when the tumor was resected as a single piece, contained within the mucosal layer and when the margin was definitely free of tumorous glands, resection was considered to be complete. Multifragment resections were defined as incomplete when tumorous glands were present in 2 or more fragments histologically, even if endoscopically the lesion had been completely removed. If the lateral margin of the lesion could not be evaluated histologically because of the effects of the electrosurgical current or mechanical damage, the resection was defined as being incomplete.
Bleeding and perforation were two major complications of ESD. Bleeding (delayed bleeding) was defined as clinical evidence of bleeding as evidenced by hematemesis or melena at 1-10 days after ESD and requiring endoscopic treatment in this study.
Values are expressed as the mean ± SD. Statistical analysis was performed using the unpaired Student’s t-test and the chi-square test. P value of less than 0.05 was considered significant.
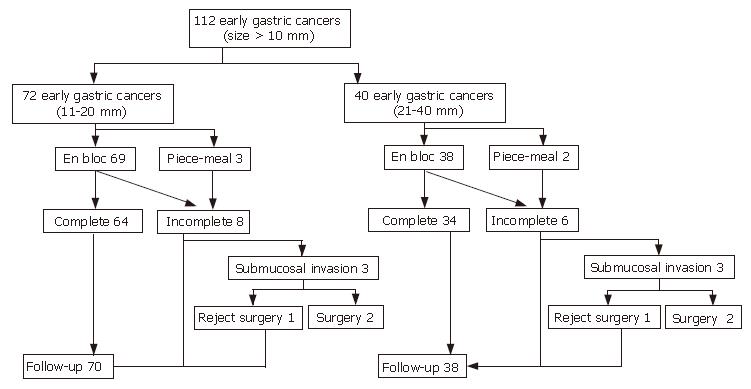
There were 40 patients in the over 20 mm group and 72 in the under 20 mm group (Table 1, Figure 2). The mean ages were 70.6 ± 8.3 years (range, 54 to 85 years) in the over 20 mm group and 70.1 ± 8.7 years (range, 45 to 89 years) in the under 20 mm group, respectively. The mean sizes of the lesions were 27.6 ± 5.7 mm in the over 20 mm group and 14.9 ± 3.2 mm in the under 20 mm group, respectively, a significant difference between the 2 groups (P < 0.001). There was no significant difference in the rate of having underlying cardiopulmonary disease between the 2 groups [2 patients (5.0%) in the over 20 mm group and 4 patients (5.6%) in the under 20 mm group]. There was no significant difference in the number of patients who had anticoagulant therapy among the groups, [4 patients (10%) in the over 20 mm group versus 8 patients (11%) in the under 20 mm group]. There was no significant difference in the one-piece resection rate among the groups (95% in the over 20 mm group versus 96% in the under 20 mm group). The one-piece resection rate was over 90% even if the tumor size was over 20 mm. There was no significant difference in the CR rate among the groups (85% in the over 20 mm group versus 89% in the under 20 mm group). The mean operation time was 72.3 ± 46.8 min for the over 20 mm group and 66.5 ± 59.7 min for the under 20 mm group, respectively. There were 5 cases of bleeding after IT-ESD: 2 (5%) in the over 20 mm group and 3 (4.2%) in the under 20 mm group, but no patient needed further surgery. Perforation occurred in one patient in the under 20 mm group and no patient needed further surgery. Fourteen patients were judged as incomplete resection. The margin of the fragment was positive for tumor or the lateral margin of the lesion could not be evaluated because of the effects of the electrosurgical current in 5 patients (3 in the over 20 mm group and 2 in the under 20 mm group). Among these 5 patients, no patients underwent additional laser or surgical therapy, although they have remained under close periodic observation. Six patients (3 in the over 20 mm group and 3 in the under 20 mm group) were judged as having submucosal invasion and 4 underwent additional surgery. The remaining 2 cases (one in each group) refused surgery and they have been under close periodic observation.
| Over 20 mmgroup(21-40 mm) | Under 20 mmgroup(11-20 mm) | P | |
| Number of patients | 40 | 72 | |
| Mean age (yr) | 70.6 ± 5.7 | 70.1 ± 8.7 | NS |
| Mean size of the lesion (mm) | 27.6 ± 5.7 | 14.9 ± 3.2 | < 0.001 |
| Frequency of the cardiopulmonary underlying disease (%) | 5.0 | 5.6 | NS |
| Frequency of the anticoagulant therapy (%) | 10 | 11 | NS |
| One piece resection rate (%) | 95 | 96 | NS |
| Complete resection rate (%) | 85 | 89 | NS |
| Operation time (min) | 72.3 ± 46.8 | 66.5 ± 59.7 | NS |
| Complications | |||
| Rate of bleeding (%) | 5 | 4.2 | NS |
| Rate of perforation (%) | 0 | 1.4 | NS |
| Depth of invasion (mucosa:submucosa) | 37:3 | 69:3 |
EMR has become a standard treatment for intramucosal gastric cancer because it is less invasive for patients compared with surgical resection. To achieve cure by EMR, one-piece resection is optimal for all lesions because it may reduce the local recurrence rate. It is easier to remove a tumor larger than 10 mm in diameter with ESD techniques using an IT-knife than with the usual strip biopsy method.
In the present study, the one-piece resection rate and CR rate were high for large lesions including those over 20 mm. The CR rate of 88% (98/112) in the present series of patients is higher than that previously reported by Miyamoto et al[6] and Imagawa et al[7]. The reason why the one-piece resection rate and CR rate were higher in our study than in that of Miyamoto et al[6] and Imagawa et al[7] might be as follows: (1) we adequately abraded the submucosal tissue under the lesion before snaring, and (2) in more than half of the patients in this study, direct dissection of the submucosal layer was carried out with an IT-knife until complete removal had been achieved.
Also, in the present study, PS for all patients was less than 2, and no patient had severe underlying diseases that might affect the result of IT-ESD in both groups. There were no patients in whom the circulatory and respiratory states were worsened during ESD even if the patients had over 20 mm lesions. We should pay particular attention to patients with hypertension or anticoagulation therapy before or during ESD because they are related to bleeding during IT-ESD or operation time[8]. The good result of IT-ESD in the over 20 mm group in this study might be due to the small number of patients having anticoagulation therapy.
The operation time for IT-ESD was longer than that of EMR using conventional methods[3,8]. The reason why IT-ESD takes longer than conventional methods might be as follows: (1) complicated operation of the IT-knife on the abrasion of the submucosal tissue and (2) a high frequency of bleeding. However, it might be worth trying as the first therapy for treating patients with mucosal gastric cancer because of its high one-piece resection rate[1,6]. In our study, there was no significant difference in the operation time among the groups because highly skilled endoscopists familiar with ESD conducted all procedures. The delayed bleeding frequency was 4.5% (5/112) which was lower than Onozato et al[9] who reported it as high as 7.6% because we prevented delayed bleeding by follow-up endoscopic examination according to the clinical pathway[3]. No patient developed delayed bleeding by one year post procedure. The perforation rate was 0.9% (1/112) in this study and no patient needed surgery. It is necessary to pay particular attention to perforations[10] because Ohkuwa et al[1], Fujishiro et al[10], Ono et al[11] and Imagawa et al[7] reported that the incidence of perforation with IT-ESD is 5%-6.1%, although the perforation frequency in the present study was extremely lower than that of the aforementioned 4 reports.
In conclusion, there was no significant difference in the result of ESD (one-piece resection rate, CR rate, operation time, bleeding rate, and perforation rate) between the over 20 mm group and the under 20 mm group. Our study proved that ESD is a feasible treatment for patients with over 20 mm mucosal gastric cancer for which their PS is less than 2, although the long-term outcome should be evaluated in the future.
S- Editor Liu Y L- Editor Kremer M E- Editor Lu W
| 1. | Ohkuwa M, Hosokawa K, Boku N, Ohtu A, Tajiri H, Yoshida S. New endoscopic treatment for intramucosal gastric tumors using an insulated-tip diathermic knife. Endoscopy. 2001;33:221-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 309] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 2. | Rösch T, Sarbia M, Schumacher B, Deinert K, Frimberger E, Toermer T, Stolte M, Neuhaus H. Attempted endoscopic en bloc resection of mucosal and submucosal tumors using insulated-tip knives: a pilot series. Endoscopy. 2004;36:788-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 185] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 3. | Hirasaki S, Tanimizu M, Moriwaki T, Hyodo I, Shinji T, Koide N, Shiratori Y. Efficacy of clinical pathway for the management of mucosal gastric carcinoma treated with endoscopic submucosal dissection using an insulated-tip diathermic knife. Intern Med. 2004;43:1120-1125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Hirasaki S, Endo H, Nishina T, Masumoto T, Tanimizu M, Hyodo I. Gastric cancer concomitant with inflammatory fibroid polyp treated with endoscopic mucosal resection using an insulation-tip diathermic knife. Intern Med. 2003;42:259-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Japanese Research Society for Gastric Cancer. Japanese Classification of Gastric Carcinoma. Tokyo: Kanehara & Co., Ltd 1999; . |
| 6. | Miyamoto S, Muto M, Hamamoto Y, Boku N, Ohtsu A, Baba S, Yoshida M, Ohkuwa M, Hosokawa K, Tajiri H. A new technique for endoscopic mucosal resection with an insulated-tip electrosurgical knife improves the completeness of resection of intramucosal gastric neoplasms. Gastrointest Endosc. 2002;55:576-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 183] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 7. | Imagawa A, Okada H, Kawahara Y, Takenaka R, Kato J, Kawamoto H, Fujiki S, Takata R, Yoshino T, Shiratori Y. Endoscopic submucosal dissection for early gastric cancer: results and degrees of technical difficulty as well as success. Endoscopy. 2006;38:987-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 233] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 8. | Hirasaki S, Tanimizu M, Nasu J, Shinji T, Koide N. Treatment of elderly patients with early gastric cancer by endoscopic submucosal dissection using an insulated-tip diathermic knife. Intern Med. 2005;44:1033-1038. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Onozato Y, Ishihara H, Iizuka H, Sohara N, Kakizaki S, Okamura S, Mori M. Endoscopic submucosal dissection for early gastric cancers and large flat adenomas. Endoscopy. 2006;38:980-986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 117] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 10. | Fujishiro M, Yahagi N, Kakushima N, Kodashima S, Muraki Y, Ono S, Kobayashi K, Hashimoto T, Yamamichi N, Tateishi A. Successful nonsurgical management of perforation complicating endoscopic submucosal dissection of gastrointestinal epithelial neoplasms. Endoscopy. 2006;38:1001-1006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 128] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 11. | Ono H, Kondo H, Gotoda T, Shirao K, Yamaguchi H, Saito D, Hosokawa K, Shimoda T, Yoshida S. Endoscopic mucosal resection for treatment of early gastric cancer. Gut. 2001;48:225-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1134] [Cited by in RCA: 1148] [Article Influence: 47.8] [Reference Citation Analysis (4)] |