Published online Jul 28, 2007. doi: 10.3748/wjg.v13.i28.3864
Revised: February 5, 2007
Accepted: February 8, 2007
Published online: July 28, 2007
AIM: To review 11 patients with parasitic cysts of the liver, who were treated by hepatic lobectomy using the liver hanging maneuver (LHM).
METHODS: Between January 2003 and June 2006, we retrospectively analyzed patients who underwent surgical treatment due to parasitic cysts of the liver, at the Ege University School of Medicine, Department of General Surgery. Of these, the patients who underwent hepatic lobectomy using the LHM were reviewed and evaluated for surgical treatment outcome.
RESULTS: Over a three-year period, there were 102 patients who underwent surgical treatment for parasitic cysts of the liver. Of these, 11 (10%) patients with parasitic cysts of the liver underwent hepatic lobectomy using the LHM. Presenting symptoms were abdominal pain, dyspepsia, and cholangitis. Cyst locations were as follows: right lobe filled with cyst, 7 (63%); segmental location, 2 (18%); and multiple locations, 2 patients (18%). All patients underwent hepatic lobectomy with an anterior approach using the LHM. The intraoperative blood transfusion requirement was one unit for 3 patients and two units for one patient. Postoperative complications included pulmonary atelectasy (2, 18%) and pleural effusion (2, 18%). No significant morbidity or mortality was observed.
CONCLUSION: We concluded that hepatic lobectomy using the LHM should be considered, not only for hepatic tumors or donor hepatectomy, but also to treat parasitic cysts of the liver.
- Citation: Unal A, Pinar Y, Murat Z, Murat K, Ahmet C. A new approach to the surgical treatment of parasitic cysts of the liver: Hepatectomy using the liver hanging maneuver. World J Gastroenterol 2007; 13(28): 3864-3867
- URL: https://www.wjgnet.com/1007-9327/full/v13/i28/3864.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i28.3864
In 2001, Belgithi first described the liver hanging maneuver (LHM) for right hepatectomy during donor operations in living-related liver transplantation or for hepatic tumors. However, it has been reported that this maneuver is also quite proper for any other disorder of the liver, except for donor hepatectomy and large hepatic tumors.
Complete excision of the cyst for patients with parasitic cysts of the liver was first described in 1981[1,2]. Currently, the best surgical procedure for complicated hydatic cysts of the liver is complete excision, including hepatic lobectomy of the cyst as well. A successful posterior approach, avoiding any complication, is quite difficult and risky. Conventional procedures are particularly chosen for parasitic cysts located in the right lobe of the liver. However, large cysts are much more prone to invade the vascular structures and diaphragm.
Can it be safer to perform hepatic lobectomy using the LHM for complicated hydatic cysts of the liver? We analyzed the results for patients who underwent hepatic lobectomy for parasitic cysts of the liver using the LHM.
Between January 2003 and July 2006, case records of 102 patients who underwent surgical treatment for hydatic cysts of the liver at Ege University School of Medicine, Department of General Surgery were retrospectively reviewed. There were 53 females and 49 males with a mean age of 52 (18-79) years. The diagnoses were as follows: hydatic cyst of the liver (n = 94), recurrent hydatic cyst (n = 4), alveolar cyst hydatic (n = 3), hydatic cyst of the liver with accompanying lung cyst (n = 1). The mean size of the cysts was 10 (4-27) cm and the most frequent location was the right lobe (64 patients; 62%).
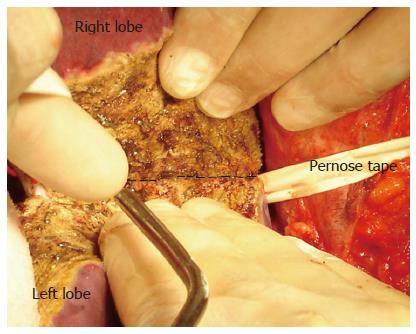
Eleven (10%) of these 102 patients underwent right hepatectomy using the LHM, whereas the remaining were treated with different surgical procedures. Before surgery, all patients were given mebendazole treatment (30 mg/kg per day) for four weeks. Data collection included demographic variables, clinical presentation, location of hydatic cysts, whether a relation with the diaphragm existed or not, the method of the LHM that was performed, intra-operative blood supplement, duration of hospital stay and postoperative complications. The anterior approach procedure for right hepatectomy was performed by using the LHM. With the last three patients, a bimanual “bi-finger” LHM was performed[3]. This alternative technique is performed without using any surgical instrument, such as a clamp, but using fingers only. In the course of retrohepatic tunnel dissection and insertion of the penrose tape, the index fingers were used, giving the advantage of feeling the accessory vascular constructions, which offered less risk of vascular injury, considering both the IVC and accessory hepatic veins (Figure 2). All patients were routinely evaluated with intraoperative Doppler ultrasonography (IOUS) to demonstrate the morphology of cysts, vascular involvement, and relation with peripheral tissue. The ultrasonographic features of the cysts were assessed according to the classification of Gharbi et al[4].
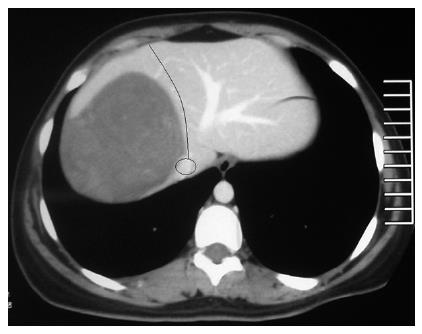
Over a three-year period, 11 (10%) patients with parasitic cysts of the liver, on whom a right hepatectomy was performed, were identified. There were 6 females and 5 males with a mean age of 41.7 (23-59) years. There were 3 patients with alveolar hydatic cysts. In addition, only one patient had a recurrent hydatic cyst for which cystotomy and drainage was performed 10 years previously for a cyst that was located in the right lobe of the liver. The mean size of the cysts was 16.3 (13-24) cm and the location of the cysts were as follows: multiple in the right lobe (n = 2), segmental (n = 2) and with remains filling the right lobe of the liver (n = 7). Abdominal pain and dyspeptic problems were the most common presenting symptoms in eight patients. One of the remaining two patients had clinical symptoms of cholangitis and the other case was asymptomatic. All serologic studies were found positive except for one. Laboratory findings showed elevated liver function enzymes in two patients and mildly elevated levels in three patients. USG and CT were performed on all of the patients for preoperative evaluation (Figure 1). In two cases, MR was needed for further evaluation. All patients were also examined with chest radiography before surgery to exclude any cyst located in the thoracic cavity. The locations of the cysts and Gharbi’s classifications are showed in Table 1. There was no typeIor type V cyst. All cysts were located in the liver and there was no evidence of spread to the abdominal cavity. The mean diameter of the cysts was 16.3 (10-24) cm. All patients were submitted to surgical exploration through a Mercedes-like incision. In all of the patients, except for one, intraoperative observation revealed adhesions between the right diaphragm and the liver. Adhesion of the cyst to the adjacent tissue was demonstrated with IOUS. In addition, the vascular relationship of the cyst with the right hepatic vein and retrohepatic inferior vena cava was evaluated. The vascular condition was as follows: pushing the hepatic vein medially (3, 37%), occlusion of the hepatic vein (4, 50%), and occlusion of the accessory vein (5, 62%). In one patient, the cyst leaned on the inferior vena cava in the caudal half. A right hepatectomy using the LHM was performed on all patients, with Belgithi’s technique[5] being used with eight patients and the bimanual “bifinger” liver hanging maneuver, which was explained in briefly in the method section (Figure 2), was used with the last three patients. All patients underwent right hepatectomy without any perforation of the cyst. Three patients needed only one unit of blood transfusion, and two units of blood transfusion were delivered to one patient. Postoperative fever was experienced by 2 patients (18%) due to pulmonary atelectasy and by 2 patients due to pleural effusion. The mean hospital stay was 8.2 (4-15) d. No postoperative surgical morbidity, such as bile leakage or hemorrhage, and no mortality were observed.
| PatientNo. | Sex | Age(yr) | Clinicalsymptom | Type | Diameter(cm) | Location | Gharbi’sclassification | Type ofLHM | BT | Postoperativecomplication |
| 1 | F | 42 | AP, D | HC | 13 | RL fulled | III | BLHM | - | - |
| 2 | F | 23 | Routine control | Alveolar HC | 10 | Segmental | - | BLHM | - | - |
| 3 | M | 51 | AP, D | HC | 16 (max) | Multiple (RL) | IV | BLHM | 1U | PA |
| 4 | F | 35 | Cholangitis | HC | 14 | RL fulled | III | BLHM | - | - |
| 5 | M | 43 | AP, D | HC | 17 | RL fulled | II | BLHM | - | - |
| 6 | M | 59 | AP, D | Alveolar HC | 24 | RL fulled | - | BBLHM | 2U | PE |
| 7 | F | 32 | AP, D | HC | 18 | RL fulled | IV | BLHM | - | - |
| 8 | F | 41 | AP, D | Alveolar HC | 16 | Segmental | - | BBLHM | - | - |
| 9 | F | 51 | Cholangitis | HC1 | 17 | RL fulled | III | BLHM | 1U | PE |
| 10 | M | 55 | AP, D | HC | 22 | RL fulled | III | BLHM | 1U | PA |
| 11 | M | 27 | AP, D | HC | 13 (max) | Multiple | IV | BLHM | - | - |
Until now, conventional surgical methods, including cystotomy and drainage, were used for the treatment of hydatic cysts of the liver. Since the 1980s, many surgical institutions have reported satisfying results with hepatectomy for hydatic cysts, due to technical advances in hepatobiliary surgery. The main concept of total cystectomy and segmentectomy or lobectomy is the excision of the cyst without perforation. By using this technique, the prevention of perforation, as well as parasitic dissemination, which is one of the likely complications, can be safely managed. Performing parenchymal transaction, which is concordant with segmental anatomy of the liver, decreases the risk of postoperative bile leakage. Although total cystectomy is the most common surgical technique in the advanced hepatobiliary centers, conventional procedures are still considered as the most proper approach, particularly for large and complicated cysts that are located next to large vascular structures. As we mentioned previously, IOUS may provide adequate information about features of the cyst.
A complicated right lobe cyst is one of the indications for total cystectomy. If we perform a posterior approach for total cystectomy, a difficult dissection may easily damage the diaphragm because of the tight adhesions between the cyst and the diaphragm or abdominal wall (Figure 3). Another problem, other than adhesions, is rupture of the cyst and subsequent dissemination, which is particularly a problem with large tumors[6]. The patients with alveolar echinococcosis are more at risk for both adhesions and dissemination. By using the liver hanging maneuver, both dissemination and uncontrollable hemorrhage during dissection of adhesions can be avoided.
An anterior approach can also be dangerous because of difficult outflow control and thus difficult homeostasis when bleeding occurs in the deep crevice of the parenchymal dissection[7]. Although the cases with hydatic cyst are suitable for an anterior approach, the risks explained above must be considered even for this benign disease. After Belgithi et al[5] first described the avascular space located in the midline of the anterior surface of the retrohepatic IVC to perform the LHM, an anterior approach could be managed safely. The last evaluation with IOUS is very helpful in deciding whether an anterior approach is convenient or not. Because the vascular pattern of both IVC and the middle hepatic vein can be demonstrated by IOUS, the surgeon may easily carry out this type of surgery. In the case of observation of any cystic adhesion to vascular patterns, an anterior approach should be avoided.
Recently, although there were many reports about the LHM, none included any information about using this technique for patients with parasitic cysts of the liver. In our study, the benefits of the LHM during hepatectomy for the surgical treatment of hydatic cysts were evaluated. According to the results of this initial study, neither intraoperative complications, including excessive hemorrhage, diaphragm injury, or cyst rupture, nor postoperative complications, including bile leakage and hemorrhage, were observed. Furthermore, no significant postoperative complication and mortality were found. However, one of the contraindications for the LHM during surgical treatment of hydatic cysts is a closed relation with IVC. Because invasion of the hydatic cyst to the IVC may cause the cyst to rupture during retrohepatic dissection, the LHM should be avoided to prevent a fatal complication in these types of patients.
In conclusion, if a right hepatectomy is planned for a large parasitic cyst of the liver, performing hepatectomy using the LHM will be much safer and more useful. It should be recognized that the experience of both the surgeon and the institution are also important in determining the outcome. We concluded that large parasitic cysts of the liver may be regarded as an indication for hepatic lobectomy using the LHM, but a much larger study is required to demonstrate the importance of this surgical procedure for parasitic cysts of the liver.
S- Editor Zhu LH L- Editor Lutze M E- Editor Wang HF
| 1. | Grundmann R, Eitenmüller J, Pichlmaier H. Indications for the various surgical procedures in hepatic echinococcosis. Chirurg. 1981;52:332-337. [PubMed] |
| 2. | Sbarounis CN, Toubouras M, Mikrou I, Kappas A, Lazarides DP. Operative treatment of the invasion of Echinococcus cysticus of the liver into the bile ducts. Chirurg. 1981;52:445-449. [PubMed] |
| 3. | Aydin U, Yazici P, Zeytunlu M, Kilic M, Coker A. Bimanual 'bi-finger' liver hanging maneuver: an alternative and safe technique for liver hanging. HPB (Oxford). 2007;9:195-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Gharbi HA, Hassine W, Brauner MW, Dupuch K. Ultrasound examination of the hydatic liver. Radiology. 1981;139:459-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 528] [Cited by in RCA: 487] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 5. | Belghiti J, Guevara OA, Noun R, Saldinger PF, Kianmanesh R. Liver hanging maneuver: a safe approach to right hepatectomy without liver mobilization. J Am Coll Surg. 2001;193:109-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 385] [Cited by in RCA: 356] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 6. | Fan ST, Lo CM, Liu CL, Lam CM, Yuen WK, Yeung C, Wong J. Hepatectomy for hepatocellular carcinoma: toward zero hospital deaths. Ann Surg. 1999;229:322-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 542] [Cited by in RCA: 559] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 7. | Lai EC, Fan ST, Lo CM, Chu KM, Liu CL. Anterior approach for difficult major right hepatectomy. World J Surg. 1996;20:314-317; discussion 318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 120] [Article Influence: 4.1] [Reference Citation Analysis (0)] |