Published online Jun 7, 2007. doi: 10.3748/wjg.v13.i21.2999
Revised: April 1, 2007
Accepted: April 7, 2007
Published online: June 7, 2007
AIM: To estimate the prognosis of patients with liver failure using a scoring model of severe viral hepatitis (SMSVH) and a model of end stage liver disease (MELD) to provide a scientific basis for clinical decision of treatment.
METHODS: One hundred and twenty patients with liver failure due to severe viral hepatitis were investigated with SMSVH established. Patients with acute, subacute, and chronic liver failure were 40, 46 and 34, respectively. The follow-up time was 6 mo. The survival rates of patients with liver failure in 2 wk, 4 wk, 3 mo and 6 mo were estimated with Kaplan-Meier method. Comparison between SMSVH and MELD was made using ROC statistic analysis.
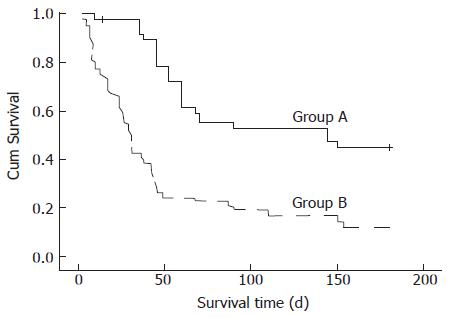
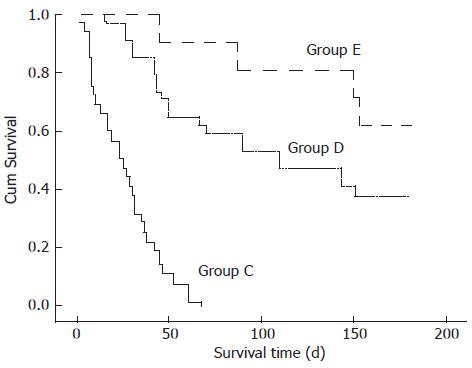
RESULTS: The survival curves of group A (at low risk, SMSVH score ≤ 4) and group B (at high risk, SMSVH score ≥ 5) were significantly different (The 4-wk, 3-mo, 6-mo survival rates were 94.59%, 54.05%, 43.24% in group A, and 51.81%, 20.48%, 12.05% in group B, respectively, P < 0.001). The survival curves of group C (SMSVH scores unchanged or increased), group D (SMSVH scores decreased by 1) and group E (SMSVH scores decreased by 2 or more) were significantly different .The survival rates of groups C, D and E were 66.15%, 100%, 100% in 2-wk; 40.0%, 91.18%, 100% in 4-wk; 0%, 58.82%, 80.95% in 3-mo and 0%, 38.24%, 61.90% in 6-mo, respectively, P < 0.001). The area under the ROC curve (AUC) of SMSVH scores at baseline and after 2 wk of therapy was significantly higher than that under the ROC curve of MELD scores (0.804 and 0.934 vs 0.689, P < 0.001).
CONCLUSION: SMSVH is superior to MELD in the estimation of the prognosis of patients with severe viral hepatitis within 6 mo. SMSVH may be regarded as a criterion for estimation of the efficacy of medical treatment and the decision of clinical treatment.
- Citation: Zhou L, Dong PL, Ding HG. Comparison scoring model of severe viral hepatitis and model of end stage liver disease for the prognosis of patients with liver failure in China. World J Gastroenterol 2007; 13(21): 2999-3002
- URL: https://www.wjgnet.com/1007-9327/full/v13/i21/2999.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i21.2999
The prognosis of patients with severe viral hepatitis is a concern of clinicians, patients and their relatives. The factors that may influence the prognosis of patients with severe viral hepatitis are complicated. Many investigators have studied the clinical condition and prognosis of severe viral hepatitis with multiple factor regression analysis, and the results are generally consistent[1-3]. We have previously established a scoring model of severe viral hepatitis (SMSVH) with logistic regression analysis[1]. The survival rate of patients with liver failure in 6 mo was investigated with SMSVH in this study, and the accuracy of SMSVH and model of end stage liver disease (MELD) was compared.
One hundred and twenty patients with liver failure due to severe viral hepatitis admitted to Beijing Youan Hospital in October 2002-January 2004 were enrolled in this study. A diagnostic workup was performed including physical examination, laboratory tests and liver pathology according to the criteria suggested by Chinese Medical Association for Liver Diseases in 2000. In brief, the diagnostic criteria of acute liver failure include significant digestive symptoms, extreme fatigue, hepatic encephalopathy within 2 wk, and prothrombin activity less than 40%. The diagnostic criteria of subacute liver failure include symptoms, physical examination and laboratory test between 15 d and 24 wk. The chronic liver failure diagnostic criteria include a history of chronic liver diseases, clinical manifestations similar to those of subacute liver failure, prothrombin activity lower than 40%, serum total bilirubin greater than 10 times of normal upper limit. Of the 120 subjects, 40 had acute liver failur, 46 had subacute liver failure, and 34 had chronic liver failure. The ratio of males to females was 98/22 and the age ranged from 17 to 74 years, the mean age was 42.5 years. The study was performed in accordance with the Declaration of Helsinki. The study program was explained to the patients and/or their relatives and informed consent was obtained from all patients. The study was approved by the Ethical Committee of Beijing You'an Hospital of Capital Medical University.
Blood was drawn from all patients for analysis of prothrombin, albumin, ALT, AST, alkaline phosphatase, gamma glutamyl transferase, bilirubin, cholesterol, createinine, urea nitrogen, serum Na+, Cl- and K+ using OLYMPUS automatic biochemical analyzer. In addition, blood was obtained for markers of hepatitis B or C by ELISA method and hepatitis B DNA by real-time PCR. Complications of liver disease were noted in the patients. The data for blood test were provided by the National Center for Clinical Laboratory.
The scoring model established with 4 independent risk factors is presented in Table 1. The patients were scored with SMSVH at admission and after 2 wk of medical therapy, and divided into group A (at low risk, SMSVH score ≤ 4) and group B (at high risk, SMSVH score ≥ 5) according to the cutoff value of the SMSVH score 5 at admission.
| Variables | Scores | |||
| 0 | 1 | 2 | 3 | |
| Clinical type | - | Chronic | Subacute | Acute |
| HE | - | Grade 1-2 | Grade 3 | Grade 4-5 |
| PTA (%) | ≥ 80 | 60-80 | 40-60 | < 40 |
| Serum sodium (mmol/L) | ≥ 135 | 125-135 | 120-125 | < 120 |
The MELD score was calculated using MELD formula[4]: MELDscore = 3.8 × ln (total bilirubin mg/dL) + 11.2 × ln (INR) + 9.6 × ln (creatinine mg/dL) + 6.4× ln (etiology: coefficient was zero in alcoholic hepatitis patients, or 1 in virus hepatitis). INR = prothrombin time ÷ 12.
A case database was established with 6 mo as the follow-up endpoint. The subjects were divided into 3 groups according to the changes in SMSVH scores after 2 wk of medical therapy: group C (SMSVH scores unchanged or increased), group D (SMSVH scores decreased by 1) and group E (SMSVH scores decreased by 2 or more).
Statistical analysis was performed using SPSS softa-ware(version13.0 for Windows). For dichotomous variables, data were analyzed by Fisher's exact test, and chi-square test. For continuous variables, data were evaluated with Student's t test. Logistic analysis was used to assess the likelihood of influence of various factors on risk of progressive diseases. Survival curves of patients with liver failure were plotted according to the Kaplan-Meier method. P < 0.05 was considered statistically significant. The accuracy of SMSVH and MELD in estimating the prognosis of patients was compared by ROC statistical analysis.
The 3- and 6-mo survival rate was 54.05% and 43.24%, respectively in group A and 20.48% and 12.05%, respectively in group B (P < 0.001, Table 2). The survival curves of the two groups differed significantly (χ2 = 22.858, P < 0.001), and the average survival time of groups A and B was 116.4 d (95% CI: 95.7-137.1) and 53.3 d (95% CI: 40.8-65.8), respectively (Table 3).
| Group A | Group B | χ2 | P | |
| 2 wk (N) | 97.30% (36/37) | 74.70% (62/83) | 8.729 | 0.003 |
| 4 wk (N) | 94.59% (35/37) | 51.81% (43/83) | 20.594 | < 0.001 |
| 3 mo (N) | 54.05% (20/37) | 20.48% (17/83) | 13.525 | < 0.001 |
| 6 mo (N) | 43.24% (16/37) | 12.05% (10/83) | 14.673 | < 0.001 |
| Group C | Group D | Group E | χ2 | P | |
| 2 wk (N) | 66.15% (43/65) | 100% (34/34) | 100% (21/21) | 22.794 | < 0.001 |
| 4 wk (N) | 40% (26/65) | 91.18% (31/34) | 100% (21/21) | 39.405 | < 0.001 |
| 3 mo (N) | 0% (0/65) | 58.82% (20/34) | 80.95% (17/21) | 66.201 | < 0.001 |
| 6 mo (N) | 0% (0/65) | 38.24% (13/34) | 61.90% (13/21) | 43.512 | < 0.001 |
Statistical analysis with Kaplan-Meier method showed that the 4-wk survival rate was 40.0% in group C and the 4-wk, 3-and 6-mo survival rate was 91.18%, 58.82% and 38.24%, respectively in group D, and 100%, 80.95% and 61.90%, respectively in group E (Table 3). The survival curves for the 3 groups differed significantly (χ2 = 91.159, P < 0.001). The average survival time of groups C, D and E was 25.8 d (95% CI: 21.6-30.1), 110.4 d (95% CI: 89.1-131.8), and 153.0 d (95% CI: 133.9-172.0), respectively. The survival time of the three groups increased gradually. The 6-mo survival rate of patients with liver failure whose SMSVH scores decreased by 2 or more was 61.90%, significantly higher than that of the patients whose SMSVH scores unchanged or increased after 2 wk of medical therapy (P < 0.001). SMSVH score could help estimate the survival time of patients with liver failure within 6 mo and decide clinical treatment and reasonable distribution of medical resources (Figures 1 and 2).
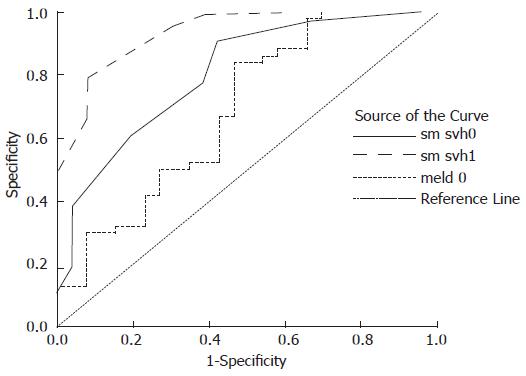
The SMSVH scores were analyzed with ROC curve (Figure 3), and the cutoff value for the scores was 5. The sensitivity and specificity were 77.7% and 88.0%, respectively. The area under the ROC curve of SMSVH scores at baseline and after 2 wk of medical therapy was 0.804 (95% CI: 0.708-0.901) and 0.934 (95% CI: 0.883-0.985), respectively. The area under the ROC curve of MELD scores at baseline was 0.689 (95% CI: 0.563-0.814), significantly lower than that under the ROC curve of SMSVH scores at baseline and after 2 wk of medical therapy (P < 0.001). The results demonstrated that the SMSVH scores at baseline and after 2 wk of medical therapy were more useful than MELD scores at baseline in estimating the prognosis of patients with liver failure.
Liver failure is induced by severe viral hepatitis and a series of complications due to extensive degeneration, necrosis and apoptosis of hepatocytes[2]. Severe viral hepatitis is dangerous, deteriorates rapidly and the case fatality rate is up to 60%-80%[1,5]. The factors that influence the prognosis of patients with severe viral hepatitis are multiple and complicated. Many investigators have studied the clinical condition and prognosis of severe hepatitis by multiple factor regression analysis, and the results are generally consistent[1-3]. In our previous study[1], 9 factors including metabolic acidosis, serum sodium, PTA, serum bilirubin, clinical type, hepatic encephalopathy, gastrointestinal bleeding, serum urea nitrogen, and spontaneous peritonitis were found to be associated with the prognosis of severe viral hepatitis, while 4 factors including serum sodium, PTA, clinical type and hepatic encephalopathy could be used as independent risk factors in estimation of the prognosis of patients with severe viral hepatitis, and SMSVH was established according to the four factors. The SMSVH scores of ≥ 5 were taken as the cutoff value in estimating the prognosis of the patients, and its accuracy was 80%[1]. Other factors such as the sex and age of patients, the type and titration of the virus were not significantly related to the prognosis of patients with severe viral hepatitis, which is consistent with the reported results[1,6-8]. A prognostic index consisting of 4 clinical and laboratory features, namely clinical type, low serum sodium and PTA, hepatic encephalopathy, can predict the likelihood of death significantly better than other published models suggesting that disease specific prognostic models and may be of value in patients with severe liver diseases in China.
It was reported that recovery from liver impairment after hepatectomy for hepatocellular carcinoma in cirrhosis starts from postoperative d 3 (POD), increased MELD scores between PODs 3 and 5 may identify patients at risk of liver failure and represents the trigger for beginning intensive treatment or evaluating salvage transplantation[9]. In this study, the survival time of 120 patients with liver failure was investigated with SMSVH, the results showed that SMSVH score of ≥ 5 was the best cutoff value in estimating the prognosis of the patients. The case fatality rate in 3- and 6-mo was 79.52% and 87.95%, respectively, which is similar to the reported results[10]. This study also demonstrated that the 2- and 4-wk survival rate of patients whose SMSVH score had no change or increased after 2 wk of medical therapy was 66.15% and 40.0%, respectively; the 2- and 4-wk, 3- and 6-mo survival rate of patients whose SMSVH score decreased by 1 was 100%, 91.18%, 58.82% and 38.24%, respectively; the 2- and 4-wk, 3- and 6-mo survival rate of patients whose SMSVH score decreased by 2 or more was 100%, 100%, 80.95% and 61.90%, respectively. The survival rates of patients with different SMSVH scores differed were significantly, suggesting that SMSVH is helpful in estimating the survival time of patients with liver failure within 6 mo. Furthermore, in comparison with the the reported survival rates[1], the survival rate of each group in this study was higher, and the reason is that some of the patients in this study administered growth hormone in combination with lactulose. Growth hormones have been demonstrated to be able to increase the survival rate of patients[11].
The Child-Pugh scoring system is the most commonly used model in the assessment of liver reservation function and prognosis of patients with liver cirrhosis[7-8,12]. The classification criteria of Child-Pugh system are strict, but lack of quantification of patients’ survival status and the inclusion of objective evaluation parameters such as ascites make the Child-Pugh system easily influenced by clinical treatment. It was reported that that cirrhotics admitted to ICU with > or = 3 failing organ systems have a 90% mortality of 90%. Sequential organ failure assessment (SOFA) and MELD are better predictors than acute physiology and chronic health evaluation (APACHE) II or Child-Pugh scores. Salerno et al[14] used MELD to estimate the short-term outcome of patients with liver cirrhosis and compared it with the Child-Pugh system, demonstrating that the MELD scoring system is superior to the Child-Pugh scoring system in the estimation of the short-term outcome of patients with liver cirrhosis receiving transjugular intrahepatic portosystemic shunt (TIPS), but the accuracy of MELD decreases in the long-term estimation[14]. Another study showed that the MELD scoring system is also a reliable method for predicting mortality in patients with AOCH[15].
At present, no easy, objective and effective model is available to estimate the prognosis of patients with severe hepatitis. SMSVH was used in this study and the score of 5 was demonstrated on ROC curve to be the best cutoff value in the estimation of the prognosis of patients with severe hepatitis. The specificity, sensitivity and discrimination power of SMSVH were 88.0%, 77.7% and 0.804 (95% CI: 0.708-0.901), respectively, suggesting that SMSVH is a relatively scientific and objective scoring system in estimation of the prognosis of patients with severe hepatitis, and can be used in clinical practice.
There is no ideal treatment for severe hepatitis so far, and the case fatality rate is up to 80%. Therefore, how to utilize the limited medical resources effectively and reduce unnecessary medical cost is concerned by all levels of government and lots of physicians. SMSVH score may help determine the clinical treatment optimum. SMSVH as a prognostic tool should be considered in predicating the progress of liver failure.
S- Editor Liu Y L- Editor Wang XL E- Editor Chen GJ
| 1. | Ding HG, Xiang HP, Shan J, Zhou L, Ma B, Liu M, Wang JT. A scoring model for predicting the prognosis of severe viral hepatitis. Chin Med J (Engl). 2005;118:249-251. [PubMed] |
| 2. | Auth MK. Are hepatic growth factors predictors of clinical outcome in fulminant hepatic failure? J Pediatr Gastroenterol Nutr. 2007;44:168-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 3. | Riordan SM, Williams R. Acute liver failure: targeted artificial and hepatocyte-based support of liver regeneration and reversal of multiorgan failure. J Hepatol. 2000;32:63-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 55] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Forman LM, Lucey MR. Predicting the prognosis of chronic liver disease: an evolution from child to MELD. Mayo End-stage Liver Disease. Hepatology. 2001;33:473-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 147] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 5. | Shakil AO, Kramer D, Mazariegos GV, Fung JJ, Rakela J. Acute liver failure: clinical features, outcome analysis, and applicability of prognostic criteria. Liver Transpl. 2000;6:163-169. [PubMed] |
| 6. | Taylor RM, Davern T, Munoz S, Han SH, McGuire B, Larson AM, Hynan L, Lee WM, Fontana RJ. Fulminant hepatitis A virus infection in the United States: Incidence, prognosis, and outcomes. Hepatology. 2006;44:1589-1597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 125] [Article Influence: 6.6] [Reference Citation Analysis (1)] |
| 7. | Durand F, Valla D. Assessment of the prognosis of cirrhosis: Child-Pugh versus MELD. J Hepatol. 2005;42 Suppl:S100-S107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 376] [Cited by in RCA: 427] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 8. | Yu JW, Wang GQ, Li SC. Prediction of the prognosis in patients with acute-on-chronic hepatitis using the MELD scoring system. J Gastroenterol Hepatol. 2006;21:1519-1524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Cucchetti A, Ercolani G, Cescon M, Ravaioli M, Zanello M, Del Gaudio M, Lauro A, Vivarelli M, Grazi GL, Pinna AD. Recovery from liver failure after hepatectomy for hepatocellular carcinoma in cirrhosis: meaning of the model for end-stage liver disease. J Am Coll Surg. 2006;203:670-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 38] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2000;31:864-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1967] [Cited by in RCA: 2069] [Article Influence: 82.8] [Reference Citation Analysis (0)] |
| 11. | Ding HG, Shan J, Zhang B, Ma HB, Zhou L, Jin R, Tan YF, He LX. Combined human growth hormone and lactulose for prevention and treatment of multiple organ dysfunction in patients with severe chronic hepatitis B. World J Gastroenterol. 2005;11:2981-2983. [PubMed] |
| 12. | Uka K, Aikata H, Takaki S, Shirakawa H, Jeong SC, Yamashina K, Hiramatsu A, Kodama H, Takahashi S, Chayama K. Clinical features and prognosis of patients with extrahepatic metastases from hepatocellular carcinoma. World J Gastroenterol. 2007;13:414-420. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 272] [Cited by in RCA: 346] [Article Influence: 19.2] [Reference Citation Analysis (1)] |
| 13. | Cholongitas E, Senzolo M, Patch D, Kwong K, Nikolopoulou V, Leandro G, Shaw S, Burroughs AK. Risk factors, sequential organ failure assessment and model for end-stage liver disease scores for predicting short term mortality in cirrhotic patients admitted to intensive care unit. Aliment Pharmacol Ther. 2006;23:883-893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 180] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 14. | Salerno F, Merli M, Cazzaniga M, Valeriano V, Rossi P, Lovaria A, Meregaglia D, Nicolini A, Lubatti L, Riggio O. MELD score is better than Child-Pugh score in predicting 3-month survival of patients undergoing transjugular intrahepatic portosystemic shunt. J Hepatol. 2002;36:494-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 214] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 15. | Blendis L. Child, MELD, hyponatremia, and now portal pressure. Gastroenterology. 2006;130:1920-1921; discussion 1921-1922;. [PubMed] |