INTRODUCTION
Heterotopic pancreas (HP) is defined as the presence of pancreatic tissue lying outside its normal location and lacking anatomical or vascular continuity with the pancreas proper[1]. In 85% to 90% of reported cases, HP has been found in stomach, duodenum, upper jejunum, whereas its presence in the gallbladder is very rare[1-3]. Similar to HP of other organs, HP of the gallbladder itself has no clinical importance and is found incidentally in most cases. However, there have been some reports of symptomatic gallbladder disease[4-7]. Herein we report a case of HP in the neck of the gallbladder who presented with clinical findings of cholecystitis.
CASE REPORT
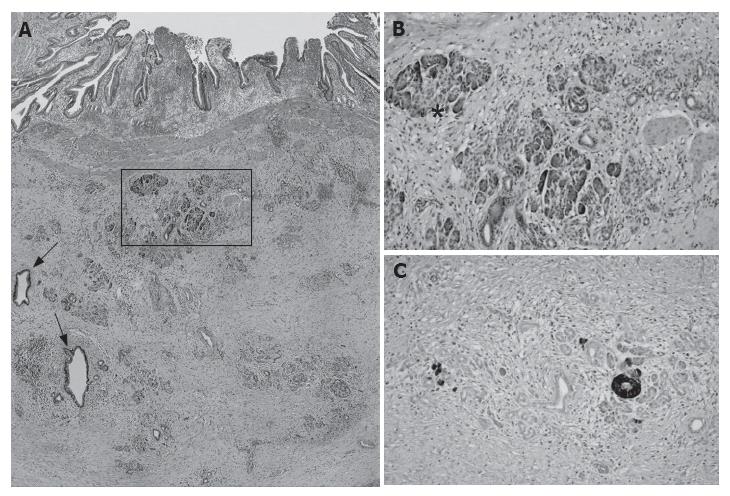
A 40-year old male presented to the hospital with epigastric pain, abdominal fullness and fever three days ago. On physical examination, the right upper abdomen was tender with a positive Murphy’s sign. His laboratory data revealed total bilirubin = 1.5 mg/dL, direct bilirubin = 0.8 mg/dL, ALP = 398 U/dL, SGOT = 70 U/dL, SGPT = 60 U/dL, GGT = 90U/dL. Ultrasonographic (US) examination showed a hydropic gallbladder without stones. A cholecystectomy was performed. The macroscopic findings were as follows: gallbladder measuring 80 mm × 50 mm × 40 mm, wall thickness 3-12 mm. In the neck region, a yellowish-white intramural nodule measuring 9 mm × 8 mm × 8 mm was observed. Microscopic examination revealed aberrant pancreatic tissue consisting of acini, ducts and chromogranin A expressing islet cells. No direct connection with the gallbladder lumen was observed (Figure 1). The whole specimen was embedded stepwise for further microscopic evaluation, but any other pancreatic tissue was not detected. The diagnosis was thereby established as chronic cholecystitis with heterotopic pancreas. All symptoms disappeared following cholecystectomy and the patient recovered completely.
Figure 1 Histological sections of HP showing dilated ducts (arrows, H&E x 100) and acini (A), acinar and islet cells (asterisk, H&E x 250) (B), and chromogranin A expressing islet cells (Mayer’s haematoxylin x 250) (C) in submucosa of gallbladder neck.
DISCUSSION
Although HP is the second most prevalent pancreatic anomaly, the incidence in gastrointestinal tract is estimated to be from 0.55% to 13.7% on autopsy, and 0.2% in laparatomy[6]. Despite the frequent occurrence of HP in the stomach, duodenum and upper jejunum, the gallbladder localization is extremely rare. Since the first publication by Poppi in 1916, only 29 more cases of HP worldwide in the gallbladder have been reported in a review of the literature up to the present[8]. In these cases there is a higher incidence of female patients between 40 and 50 years of age[9]. However, similar to our case, its occurrences have been reported in men. In half of the reported cases, HP is preferentially localized close to the neck of the gallbladder[9]. Parallel to this observation, in our patient HP was located in the neck region.
HP in the gallbladder is very rarely symptomatic. In most reported cases, it is an incidental pathological findings and coexists with gallstones[9,10]. However, there have been some reported symptomatic gallbladder diseases due to HP[4-7]. In one case HP has been found to cause perforation of the gallbladder and lead to peritonitis[5]. Similar to our case, in two cases HP has been found to stimulate cholecystopathy with all symptoms disappearing following cholecystectomy[4,7]. Inceoglu et al[6] have reported a case of HP in the cystic duct with hydrops of the gallbladder and chronic pancreatitis of the ectopic tissue. In all cases including the case presented here, because of its rare occurrence as a symptomatic lesion, HP is not taken into consideration in the clinical differential diagnosis. Indeed, as in other organs, the preoperative diagnosis of HP in gallbladder is difficult[10,11]. Symptomatology and clinical findings in most cases suggest gallbladder disease, mainly lithiasis and cholecystitis[9]. It was pointed out that HP located especially in the neck region might prevent bile flow like a stone and cause hydrops of the gallbladder mimicking the clinical findings of these diseases[6]. From this point of view, in our case localization of HP in the neck region might explain the clinical findings of cholecystitis related to hydrops of the gallbladder without cholelithiasis. Recently it was indicated that, despite its high resolution, US is not specific for HP and impossible to distinguish HP from other lesions such as cholesterol polyps, adenoma and carcinoma[9,11]. Parallel to these observations, in our case while US examination revealed a hydropic gallbladder without stones, it failed to detect HP. For these reasons, we suggest that the rare occurrence of HP in the gallbladder and its presence as an incidental finding in cholecystectomy materials do not exclude its consideration in the differential diagnosis of symptomatic gallbladder diseases.
Our histopathological examination revealed a HP constituted of acini, ducts and islet cells, corresponding to the total heterotopia[8]. Although panreatitis may occur in HP, the present case had no histopathological findings of pancreatitis[6].
The origin of heterotopic pancreatic tissue is controversial but two theories have been proposed. One suggests that pancreatic tissue is separated from the main pancreas during embryonic rotation[5,6], the other is that during the growth of the ventral pancreatic bud a proportion is transported by the longitudinal growth of the intestines[5,6]. Therefore its presence in the gallbladder might indicate derivation from the ventral diverticulum. On the other hand, the site of organ/tissue formation is also determined by strictly coordinated developmental programs involving interplay between extracellular signaling and intracellular transcriptional factor networks. It has been demonstrated that in mammals the developmental decisions according to the state of the immediate neighbors are controlled through the Notch signaling system[12]. Several studies indicate that this system also plays an essential role in the precise orchestration of cell-fate decisions in the developing pancreas[13]. Hes-1 (Hairy enhancer of split), a main effector of Notch signaling is required for region-appropriate specification of the pancreas in the developing foregut endoderm[14]. In experimental studies, ectopic pancreas formation has been observed in Hes-1 knockout mice and the plasticity of endodermal progenitors of the gut, bile duct, and pancreas has been suggested[14,15]. In light of these observations, we consider that besides two proposed theories, abnormalities in the Notch signaling system, especially in Hes-1 expression during embryogenesis may also contribute to the formation of HP of the gallbladder.
In conclusion, HP of the gallbladder is a very rare condition which is diagnosed incidentally, but may cause clinical symptoms such as cholecystitis and should be taken into consideration in patients with symptomatic gallbladder disease without any other specific clinical and laboratory findings before it is diagnosed as idiopathic.