Published online Jan 14, 2007. doi: 10.3748/wjg.v13.i2.219
Revised: October 7, 2006
Accepted: November 11, 2006
Published online: January 14, 2007
Abdominal pain and bowel habits alterations are common symptoms in the general population. The investigation to differentiate organic from functional bowel disorders represents a considerable burden both for patients and public health service. The selection of patients who should undergo endoscopic and/or radiological procedures is one of the key points of the diagnostic process, which should avoid the abuse of invasive and expensive tests as well as the underestimation of potentially harmful diseases. Over the coming years, clinicians and researchers will be challenged to develop strategies to increase the patient’s compliance and to reduce the economic and social costs of the intestinal diseases.
- Citation: Costa F, Mumolo MG, Marchi S, Bellini M. Differential diagnosis between functional and organic intestinal disorders: Is there a role for non-invasive tests? World J Gastroenterol 2007; 13(2): 219-223
- URL: https://www.wjgnet.com/1007-9327/full/v13/i2/219.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i2.219
For the sake of simplicity, bowel diseases have been divided into organic (OBD) and functional (FBD) disorders. In the past, FBD was merely considered an “umbrella” for many clinical pictures where the term functional reflected an unknown etiology and/or pathogenesis and their existence was even denied by some physicians[1,2]. In the last years, the fast-growing insight into the pathogenesis of intestinal diseases has been narrowing the field of disturbances “not explained by structural or biochemical abnormalities”, in parallel with the progress of diagnostic tools and the development of novel technologies. Recent evidences, such as the role of serotonin in visceral functions[3-5], the post-infective onset of irritable bowel syndrome (IBS)[6] or data about potential neuroendocrine dysfunctions[7] shed light on the phenomena underlying FBD. The “biopsychosocial model” focused on the complex interplay among genetics, environment, psychosocial and physiological factors, significantly contributed to clarify the true genesis of “functional” symptoms and to modify both treatment and clinical outcome[8]. However, while the new scenario of pathogenesis suggests an overlapping between morphologic and functional abnormalities, in clinical practice the distinction is maintained in prognostic terms, as “functional” identifies scarcely evolutive and virtually harmless conditions.
As the intestine reacts to different stimuli with a limited array of symptoms, the investigation to differentiate OBD and FBD represents a considerable burden for both the patients and public health service.
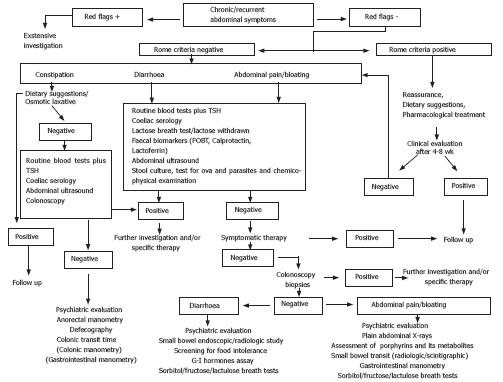
The selection of patients who should undergo endoscopic and/or radiological procedures is one of the key points of the diagnostic process, which should avoid the abuse of invasive and expensive tests as well as the underestimation of potentially dangerous diseases. In particular, we should take into account the high prevalence and increasing incidence of colo-rectal cancer which, at an early stage, can be successfully treated by endoscopic resection. Nevertheless, colonoscopy is not advisable in all patients with abdominal complaints in the absence of “red flag” features (age > 45 years, anaemia, bleeding, fever, weight loss, etc.) (Figure 1). Chronic or recurrent abdominal pain and bowel habit alterations are common symptoms in the general population. Because a wide range of etiologies may underlie these symptoms, they do not allow a differential diagnosis between OBD (neoplasm, infectious enteritis, Crohn’s disease, celiac disease, etc.) and FBD. Moreover, patients may present overlapping syndromes as OBD and FBD , are not mutually exclusive and can be present in the same patient. FBD, mainly IBS, which affect 5%-20% of general population, are the most common intestinal disorders in both primary and secondary care[9-11]. Most patients are diagnosed and treated by general practitioners (GPs) and only those unresponsive to conventional treatment[10,12] are eventually referred to a gastroenterologist[9,13].
In order to improve the positive identification of patients affected with FBD, the Rome classification system has been developed. Although these guidelines have raised controversies about duration, frequency, severity and terminology itself of symptoms, they have created a common language for FBD and are now considered the gold standard. Unfortunately, Rome criteria have been developed by and for specialists working in the secondary care setting; they are ignored by many GPs and considered by others, as well as by many specialists, too complex and time-consuming and/or restrictive, suitable only for the tertiary care setting and for research purposes[14]. Therefore, many GPs and gastroenterologists are confident of making a correct diagnosis based on their personal criteria[14,15] and, in the absence of any biological or instrumental marker, FBD is still an exclusive diagnosis which often require extensive investigation. The recent Rome III criteria appear to be simpler and less restrictive and hopefully will help the diagnosis of FBD on clinical basis[16].
When FBD is suspected, the clinical criteria can be combined with a number of non-invasive diagnostic tools. Unfortunately serological biomarkers of inflammation such as erythrocyte sedimentation rate, C-reactive protein, white cell count, platelet count, are not sufficiently sensitive or sufficiently specific because they do not directly reflect the level of local inflammation[17-19]. The faecal occult blood test is of little use in detecting inflammatory bowel diseases (IBD) and has a low sensitivity for the diagnosis of colon cancer, especially at an early stage[20,21]. Therefore, in recent years considerable effort has been devoted to find alternative solutions. The latest knowledge about the pathogenesis of FBD (infection, food allergy or intolerance)[22-24], have focused attention on the role of microscopic inflammation, bacterial overgrowth, altered immunity and even more subtle alterations, whose effects are detectable in non-invasive manner, by analysing stools, breath samples and blood.
Faecal neutrophil-derived proteins (mainly calprotectin and lactoferrin) assessment is receiving increasing attention as promising tools to differentiate OBD and FBD; although their clinical use needs definitive confirmation especially in the work-up of FBD, they could be the putative ideal test for non-invasive assessment of intestinal inflammation[25-27].
Calprotectin is a 36-kDa calcium and zinc binding protein that accounts for about 60% of total proteins in the cytosol fraction of neutrophil granulocytes[28,29]. An increase in faecal calprotectin levels in IBD, colorectal cancer and non-steroidal anti-inflammatory drugs enteropathy has been reported[30-33]. In a study of Dolwani, faecal calprotectin was superior to small bowel barium follow-up in identifying patients with organic diseases[34]. In Crohn’s disease (CD) and ulcerative colitis (UC), its levels closely correlated with the faecal excretion of 111In-labelled leukocytes, which is considered to be the gold standard for measuring intestinal inflammation[35] and recently it has been reported that a high faecal calprotectin concentration may identify those IBD patients in remission who are at risk of early relapse[36,37]. Calprotectin has a high negative predictive value for intestinal inflammation. It has low specificity for intestinal pathology but, at a cut-off of 30 mg/L (150 μg/g of faeces by the new method), it showed a sensitivity of 100% in discriminating between active Crohn’s disease and IBS[27]. The combined use of presence/absence of alarm features, Rome criteria and calprotectin test proved to be a non-invasive, effective mean of screening patients for organic intestinal disease[38].
Lactoferrin is an iron-binding protein contained in organic fluid, intestinal mucus and in neutrophils. Similarly to calprotectin, faecal lactoferrin proved to be a simple, sensitive marker of intestinal inflammation[25,39,40].
The molecular genetics of colorectal cancer provided the basis for the analysis of faecal DNA[41]. Colonoscopy is the best tool for the diagnosis of colorectal cancer but it cannot be proposed for a systematic screening of the entire population > 50 years of age. The recent availability of faecal-based, multi-target DNA panel has allowed a better sensitivity than faecal occult blood test for the detection of colorectal cancer[21]. This panel consists of different mutations (K-ras gene, APC gene, p53 gene), markers of microsatellite-instability and markers of disordered apoptosis, clearly involved in the progression of colorectal cancer. Although the performance of faecal DNA testing is not comparable to colonoscopy, it is simple and non-invasive, therefore its use at frequent intervals might compensate for the lower diagnostic accuracy[21].
Chronic pancreatitis is a frequent cause of abdominal pain and diarrhoea whose diagnosis often requires complex and expensive procedures. The assessment of pancreatic elastase on stools seems to offer a better performance than previous non-invasive tests (i.e. serology, Pancreolauryl test, faecal tests for pancreatic enzyme) with a high sensitivity for moderate and severe pancreatic insufficiency[42,43]; this faecal test, like faecal neutrophil-derived protein assessment, is easy to perform, requires a single stool sample and offers a great advantage in terms of patient’s compliance. Although most authors reported poor sensitivity for mild disease, its use has been recommended as a first choice test in patients with chronic diarrhoea of putative pancreatic origin[44].
If these experimental data are confirmed in large controlled studies, the routine use of faecal tests might contribute to the selection of patients with abdominal complaints both in the first diagnosis and in the follow-up avoiding invasive and expensive procedures.
Breath analysis is a simple and safe alternative to invasive tests to investigate digestive functions. Exhaled hydrogen (H2) and carbon (C) can be employed to assess malabsorption, gastrointestinal motility and H pylori infection. H2 in humans is produced only by bacterial fermentation of carbohydrates[45]. This process has been related to the onset of symptoms such as diarrhoea, bloating and abdominal pain[46,47]. Different hydrogen breath tests are currently used to detect carbohydrate malabsorption. Lactose, fructose, sorbitol are the most commonly tested carbohydrates, although their role in symptoms of FBD is controversial, and the prevalence of lactose, fructose and sorbitol malabsorption in IBS patients is not different from healthy subjects[48].
Small intestinal bacterial overgrowth (SIBO) is a malabsorption syndrome characterized by more than 105 colonic type bacterial/mL of jejunal juice described in case of structural bowel alterations (surgical blind loop, stenosis, etc), motility disturbances (pseudo-obstruction, diabetic autonomic neuropathy, sclerodermia) and also present in chronic diseases (liver cirrhosis, chronic pancreatitis, chronic renal failure)[49]. Recent data also indicate that an altered gut flora may play a pathogenic role both in IBS and IBD[50,51]. It has been shown that eradication of SIBO eliminates IBS symptoms in 48% of patients[52]. Although jejunal culture is considered the gold standard for the diagnosis of SIBO, some drawbacks limit its widespread use; thus, glucose and lactulose breath tests are commonly employed. Breath tests based on the excretion of CO2 subsequently measured by a mass spectrometer have been developed; they employ a variety of 13C substrates to investigate the exocrine pancreatic function (13C triolein, 13C mixed chain triglyceride)[53], gastric emptying (13C octanoate)[54], as well as in the diagnosis of H pylori infection (13C urea)[55].
The simplicity and the safety of breath tests encouraged a widespread use, but the data on their low diagnostic accuracy should be taken into account and their use on regular basis cannot be recommended in clinical practice[56].
Recent literature highlighted that approximately 4% of patients diagnosed as IBS are affected with celiac disease[57]. Altered bowel habits and abdominal pain, the clinical hallmark of IBS, are common in celiac patients, and serological assessment for anti-endomysial and anti-transglutaminase antibodies should be performed as a first level test when IBS is suspected. Many patients suffering from abdominal pain and/or bowel habit changes perceive their symptoms as related to some form of dietary intolerance and show a good response to an exclusive diet. Nevertheless, any attempt to correlate food-specific IgE production and chronic abdominal symptoms has been disappointing[24,58]. Although it has been reported that sometimes IgE-mediated reactivity can present with chronic abdominal complaints, the measurement of food-specific IgE antibody concentrations to ascertain food intolerance in FBD is not justified and should be discouraged[59]. Preliminary data showed that high titres of food-specific IgG4 antibodies are present in IBS patients suggesting a diagnostic role in those cases of IBS who could benefit mostly by an exclusive diet[60]. Their clinical follow-up and further research are needed to clarify the importance of these findings and their role in clinical practice.
Likely the near future will lead to a deep revision of the concept of “functional disorder”. The striking progress in our knowledge of the molecular basis of diseases is identifying new models for FBD pathogenesis, which tend to be less “functional” and more “organic”.
These new evidences will have a relevant effect on the clinical management of intestinal diseases. We are not far from the time when the development of minimally or non-invasive techniques will allow an accurate diagnosis, a serial monitoring and a “real time” adjustment of therapy.
S- Editor Wang GP L- Editor Ma JY E- Editor Lu W
| 1. | Drossman DA. Functional GI disorders: what's in a name? Gastroenterology. 2005;128:1771-1772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 36] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Christensen J. Heraclides or the physician. Gastroenterol Int. 1990;3:45-48. |
| 3. | Gershon MD. Review article: roles played by 5-hydroxytryptamine in the physiology of the bowel. Aliment Pharmacol Ther. 1999;13 Suppl 2:15-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 255] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 4. | Camilleri M. Pharmacogenomics and functional gastrointestinal disorders. Pharmacogenomics. 2005;6:491-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Bellini M, Rappelli L, Blandizzi C, Costa F, Stasi C, Colucci R, Giannaccini G, Marazziti D, Betti L, Baroni S. Platelet serotonin transporter in patients with diarrhea-predominant irritable bowel syndrome both before and after treatment with alosetron. Am J Gastroenterol. 2003;98:2705-2711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 46] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Drossman DA. Mind over matter in the postinfective irritable bowel. Gut. 1999;44:306-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Dinan TG, Quigley EM, Ahmed SM, Scully P, O'Brien S, O'Mahony L, O'Mahony S, Shanahan F, Keeling PW. Hypothalamic-pituitary-gut axis dysregulation in irritable bowel syndrome: plasma cytokines as a potential biomarker? Gastroenterology. 2006;130:304-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 440] [Cited by in RCA: 455] [Article Influence: 23.9] [Reference Citation Analysis (1)] |
| 8. | Drossman DA. The functional gastrointestinal disorders and the Rome II process. Gut. 1999;45 Suppl 2:II1-II5. [PubMed] |
| 9. | Jones R, Lydeard S. Irritable bowel syndrome in the general population. BMJ. 1992;304:87-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 408] [Cited by in RCA: 428] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 10. | Thompson WG, Heaton KW, Smyth GT, Smyth C. Irritable bowel syndrome in general practice: prevalence, characteristics, and referral. Gut. 2000;46:78-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 318] [Cited by in RCA: 341] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 11. | Drossman DA, Camilleri M, Mayer EA, Whitehead WE. AGA technical review on irritable bowel syndrome. Gastroenterology. 2002;123:2108-2131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 933] [Cited by in RCA: 950] [Article Influence: 41.3] [Reference Citation Analysis (1)] |
| 12. | Gladman LM, Gorard DA. General practitioner and hospital specialist attitudes to functional gastrointestinal disorders. Aliment Pharmacol Ther. 2003;17:651-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 31] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Heaton KW, O'Donnell LJ, Braddon FE, Mountford RA, Hughes AO, Cripps PJ. Symptoms of irritable bowel syndrome in a British urban community: consulters and nonconsulters. Gastroenterology. 1992;102:1962-1967. [PubMed] |
| 14. | Bellini M, Tosetti C, Costa F, Biagi S, Stasi C, Del Punta A, Monicelli P, Mumolo MG, Ricchiuti A, Bruzzi P. The general practitioner's approach to irritable bowel syndrome: from intention to practice. Dig Liver Dis. 2005;37:934-939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Vandvik PO, Aabakken L, Farup PG. Diagnosing irritable bowel syndrome: poor agreement between general practitioners and the Rome II criteria. Scand J Gastroenterol. 2004;39:448-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480-1491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3413] [Cited by in RCA: 3383] [Article Influence: 178.1] [Reference Citation Analysis (1)] |
| 17. | Cronin CC, Shanahan F. Immunological tests to monitor inflammatory bowel disease--have they delivered yet? Am J Gastroenterol. 1998;93:295-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999;340:448-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4404] [Cited by in RCA: 4614] [Article Influence: 177.5] [Reference Citation Analysis (0)] |
| 19. | Suffredini AF, Fantuzzi G, Badolato R, Oppenheim JJ, O'Grady NP. New insights into the biology of the acute phase response. J Clin Immunol. 1999;19:203-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 280] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 20. | Tibble J, Sigthorsson G, Foster R, Sherwood R, Fagerhol M, Bjarnason I. Faecal calprotectin and faecal occult blood tests in the diagnosis of colorectal carcinoma and adenoma. Gut. 2001;49:402-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 126] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 21. | Imperiale TF, Ransohoff DF, Itzkowitz SH, Turnbull BA, Ross ME. Fecal DNA versus fecal occult blood for colorectal-cancer screening in an average-risk population. N Engl J Med. 2004;351:2704-2714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 548] [Cited by in RCA: 525] [Article Influence: 25.0] [Reference Citation Analysis (3)] |
| 22. | Barbara G, Stanghellini V, De Giorgio R, Cremon C, Cottrell GS, Santini D, Pasquinelli G, Morselli-Labate AM, Grady EF, Bunnett NW. Activated mast cells in proximity to colonic nerves correlate with abdominal pain in irritable bowel syndrome. Gastroenterology. 2004;126:693-702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1004] [Cited by in RCA: 1025] [Article Influence: 48.8] [Reference Citation Analysis (0)] |
| 23. | Gonsalkorale WM, Perrey C, Pravica V, Whorwell PJ, Hutchinson IV. Interleukin 10 genotypes in irritable bowel syndrome: evidence for an inflammatory component? Gut. 2003;52:91-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 198] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 24. | Atkinson W, Sheldon TA, Shaath N, Whorwell PJ. Food elimination based on IgG antibodies in irritable bowel syndrome: a randomised controlled trial. Gut. 2004;53:1459-1464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 347] [Cited by in RCA: 344] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 25. | Kane SV, Sandborn WJ, Rufo PA, Zholudev A, Boone J, Lyerly D, Camilleri M, Hanauer SB. Fecal lactoferrin is a sensitive and specific marker in identifying intestinal inflammation. Am J Gastroenterol. 2003;98:1309-1314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 249] [Cited by in RCA: 259] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 26. | Limburg PJ, Ahlquist DA, Sandborn WJ, Mahoney DW, Devens ME, Harrington JJ, Zinsmeister AR. Fecal calprotectin levels predict colorectal inflammation among patients with chronic diarrhea referred for colonoscopy. Am J Gastroenterol. 2000;95:2831-2837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 126] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 27. | Tibble J, Teahon K, Thjodleifsson B, Roseth A, Sigthorsson G, Bridger S, Foster R, Sherwood R, Fagerhol M, Bjarnason I. A simple method for assessing intestinal inflammation in Crohn's disease. Gut. 2000;47:506-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 346] [Cited by in RCA: 351] [Article Influence: 14.0] [Reference Citation Analysis (1)] |
| 28. | Dale I, Fagerhol MK, Naesgaard I. Purification and partial characterization of a highly immunogenic human leukocyte protein, the L1 antigen. Eur J Biochem. 1983;134:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 165] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 29. | Fagerhol MK, Andersson KB, Naess-Andresen CF, Brandtzaeg P, Dale I. Calprotectin (the LI leukocyte protein). Stimulus Response Coupling: the role of intracellular calcium-binding proteins. Boca Raton FL: CRC Press Inc 1990; 187-210. |
| 30. | Røseth AG, Aadland E, Jahnsen J, Raknerud N. Assessment of disease activity in ulcerative colitis by faecal calprotectin, a novel granulocyte marker protein. Digestion. 1997;58:176-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 256] [Cited by in RCA: 258] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 31. | Costa F, Mumolo MG, Bellini M, Romano MR, Ceccarelli L, Arpe P, Sterpi C, Marchi S, Maltinti G. Role of faecal calprotectin as non-invasive marker of intestinal inflammation. Dig Liver Dis. 2003;35:642-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 209] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 32. | Kronborg O, Ugstad M, Fuglerud P, Johne B, Hardcastle J, Scholefield JH, Vellacott K, Moshakis V, Reynolds JR. Faecal calprotectin levels in a high risk population for colorectal neoplasia. Gut. 2000;46:795-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 64] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 33. | Tibble JA, Sigthorsson G, Foster R, Scott D, Fagerhol MK, Roseth A, Bjarnason I. High prevalence of NSAID enteropathy as shown by a simple faecal test. Gut. 1999;45:362-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 225] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 34. | Dolwani S, Metzner M, Wassell JJ, Yong A, Hawthorne AB. Diagnostic accuracy of faecal calprotectin estimation in prediction of abnormal small bowel radiology. Aliment Pharmacol Ther. 2004;20:615-621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 71] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 35. | Røseth AG, Schmidt PN, Fagerhol MK. Correlation between faecal excretion of indium-111-labelled granulocytes and calprotectin, a granulocyte marker protein, in patients with inflammatory bowel disease. Scand J Gastroenterol. 1999;34:50-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 296] [Cited by in RCA: 307] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 36. | Tibble JA, Sigthorsson G, Bridger S, Fagerhol MK, Bjarnason I. Surrogate markers of intestinal inflammation are predictive of relapse in patients with inflammatory bowel disease. Gastroenterology. 2000;119:15-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 545] [Cited by in RCA: 543] [Article Influence: 21.7] [Reference Citation Analysis (1)] |
| 37. | Costa F, Mumolo MG, Ceccarelli L, Bellini M, Romano MR, Sterpi C, Ricchiuti A, Marchi S, Bottai M. Calprotectin is a stronger predictive marker of relapse in ulcerative colitis than in Crohn's disease. Gut. 2005;54:364-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 383] [Cited by in RCA: 424] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 38. | Tibble JA, Sigthorsson G, Foster R, Forgacs I, Bjarnason I. Use of surrogate markers of inflammation and Rome criteria to distinguish organic from nonorganic intestinal disease. Gastroenterology. 2002;123:450-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 294] [Cited by in RCA: 301] [Article Influence: 13.1] [Reference Citation Analysis (2)] |
| 39. | Sugi K, Saitoh O, Hirata I, Katsu K. Fecal lactoferrin as a marker for disease activity in inflammatory bowel disease: comparison with other neutrophil-derived proteins. Am J Gastroenterol. 1996;91:927-934. [PubMed] |
| 40. | Parsi MA, Shen B, Achkar JP, Remzi FF, Goldblum JR, Boone J, Lin D, Connor JT, Fazio VW, Lashner BA. Fecal lactoferrin for diagnosis of symptomatic patients with ileal pouch-anal anastomosis. Gastroenterology. 2004;126:1280-1286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 82] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 41. | Sidransky D, Tokino T, Hamilton SR, Kinzler KW, Levin B, Frost P, Vogelstein B. Identification of ras oncogene mutations in the stool of patients with curable colorectal tumors. Science. 1992;256:102-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 513] [Cited by in RCA: 475] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 42. | Löser C, Möllgaard A, Fölsch UR. Faecal elastase 1: a novel, highly sensitive, and specific tubeless pancreatic function test. Gut. 1996;39:580-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 373] [Cited by in RCA: 375] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 43. | Glasbrenner B, Schön A, Klatt S, Beckh K, Adler G. Clinical evaluation of the faecal elastase test in the diagnosis and staging of chronic pancreatitis. Eur J Gastroenterol Hepatol. 1996;8:1117-1120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 50] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 44. | Thomas PD, Forbes A, Green J, Howdle P, Long R, Playford R, Sheridan M, Stevens R, Valori R, Walters J. Guidelines for the investigation of chronic diarrhoea, 2nd edition. Gut. 2003;52 Suppl 5:v1-v15. [PubMed] |
| 45. | Levitt MD. Production and excretion of hydrogen gas in man. N Engl J Med. 1969;281:122-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 391] [Cited by in RCA: 347] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 46. | Böhmer CJ, Tuynman HA. The effect of a lactose-restricted diet in patients with a positive lactose tolerance test, earlier diagnosed as irritable bowel syndrome: a 5-year follow-up study. Eur J Gastroenterol Hepatol. 2001;13:941-944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 62] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 47. | Farup PG, Monsbakken KW, Vandvik PO. Lactose malabsorption in a population with irritable bowel syndrome: prevalence and symptoms. A case-control study. Scand J Gastroenterol. 2004;39:645-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 77] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 48. | Nelis GF, Vermeeren MA, Jansen W. Role of fructose-sorbitol malabsorption in the irritable bowel syndrome. Gastroenterology. 1990;99:1016-1020. [PubMed] |
| 49. | Teo M, Chung S, Chitti L, Tran C, Kritas S, Butler R, Cummins A. Small bowel bacterial overgrowth is a common cause of chronic diarrhea. J Gastroenterol Hepatol. 2004;19:904-909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 29] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 50. | Franchimont D, Vermeire S, El Housni H, Pierik M, Van Steen K, Gustot T, Quertinmont E, Abramowicz M, Van Gossum A, Devière J. Deficient host-bacteria interactions in inflammatory bowel disease? The toll-like receptor (TLR)-4 Asp299gly polymorphism is associated with Crohn's disease and ulcerative colitis. Gut. 2004;53:987-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 438] [Cited by in RCA: 445] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 51. | Quigley EM. Irritable bowel syndrome and inflammatory bowel disease: interrelated diseases? Chin J Dig Dis. 2005;6:122-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 52. | Pimentel M, Chow EJ, Lin HC. Eradication of small intestinal bacterial overgrowth reduces symptoms of irritable bowel syndrome. Am J Gastroenterol. 2000;95:3503-3506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 508] [Cited by in RCA: 485] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 53. | Vantrappen GR, Rutgeerts PJ, Ghoos YF, Hiele MI. Mixed triglyceride breath test: a noninvasive test of pancreatic lipase activity in the duodenum. Gastroenterology. 1989;96:1126-1134. [PubMed] |
| 54. | Ghoos YF, Maes BD, Geypens BJ, Mys G, Hiele MI, Rutgeerts PJ, Vantrappen G. Measurement of gastric emptying rate of solids by means of a carbon-labeled octanoic acid breath test. Gastroenterology. 1993;104:1640-1647. [PubMed] |
| 55. | Soll AH. Consensus conference. Medical treatment of peptic ulcer disease. Practice guidelines. Practice Parameters Committee of the American College of Gastroenterology. JAMA. 1996;275:622-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 117] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 56. | Simrén M, Stotzer PO. Use and abuse of hydrogen breath tests. Gut. 2006;55:297-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 300] [Cited by in RCA: 287] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 57. | Spiegel BM, DeRosa VP, Gralnek IM, Wang V, Dulai GS. Testing for celiac sprue in irritable bowel syndrome with predominant diarrhea: a cost-effectiveness analysis. Gastroenterology. 2004;126:1721-1732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 86] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 58. | Monsbakken KW, Vandvik PO, Farup PG. Perceived food intolerance in subjects with irritable bowel syndrome-- etiology, prevalence and consequences. Eur J Clin Nutr. 2006;60:667-672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 255] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 59. | Sampson HA, Sicherer SH, Birnbaum AH. AGA technical review on the evaluation of food allergy in gastrointestinal disorders. American Gastroenterological Association. Gastroenterology. 2001;120:1026-1040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 78] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 60. | Zar S, Benson MJ, Kumar D. Food-specific serum IgG4 and IgE titers to common food antigens in irritable bowel syndrome. Am J Gastroenterol. 2005;100:1550-1557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 82] [Article Influence: 4.1] [Reference Citation Analysis (0)] |