Published online May 21, 2007. doi: 10.3748/wjg.v13.i19.2722
Revised: January 21, 2007
Accepted: February 8, 2007
Published online: May 21, 2007
AIM: To evaluate the impact of the diagnosis of hepatitis C infection on lifestyle habits such as smoking, drinking, sports activity and diet.
METHODS: A self-administered, anonymous question-naire was offered to out-patients with HCV infection consecutively attending three clinical centres in Italy.
RESULTS: Of the 275 respondents, 62.2% (171) were male. Mean age was 51 (range 20-80) years. Overall, after the diagnosis of hepatitis C, 74.5% of drinkers had modified (giving up or reducing) alcohol consumption, 21.3% of smokers had modified their habits and 32.3% of subjects who reported sports activity had either stopped or reduced frequency of activity or chose a less fatiguing sport. Sixty-four percent of the respondents reported having modified their diet, most of them on physician's advice.
CONCLUSION: After the diagnosis of hepatitis C many patients correctly modified their alcohol consumption and a minority their smoking habits. The reason for reported changes in diet and physical activity needs further investigations.
- Citation: Scognamiglio P, Galati V, Navarra A, Longo MA, Aloisi MS, Antonini MG, Puoti M, Almasio PL, Ippolito G, Girardi E. Impact of hepatitis C virus infection on lifestyle. World J Gastroenterol 2007; 13(19): 2722-2726
- URL: https://www.wjgnet.com/1007-9327/full/v13/i19/2722.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i19.2722
Hepatitis C virus (HCV) is now the most frequent cause of chronic liver disease, including cirrhosis and hepatocellular carcinoma (HCC)[1]. HCV may diminish health-related quality of life (HRQOL) also in the absence of clinically significant liver disease; in particular the impact of HCV seems to be most dramatic in social and physical function, general health and vitality[2]. Physicians involved in the management of chronic hepatitis C are consulted by their patients regarding measures that may prevent further liver disease progression and about correct health-related behaviours such as nutrition or physical activity. However current international guidelines do not address these issues with the exception of alcohol and obesity[3-8], while evidence on the influence of lifestyle on disease progression and outcome are accumulating[9-11]. In contrast, reflecting patients’ needs for specific information, recommendations about health-promoting lifestyle for individuals with hepatitis C infection are widely available on web sites or magazines.
There are few data available regarding how many patients with hepatitis C infection change their lifestyle, adopting healthy behaviours and/or unnecessary restrictions[12-14]. This information is necessary to plan educational programmes and to improve counselling given to chronic hepatitis C patients.
Here we report results from a questionnaire-based survey we conducted among out-patients attending three clinical centres in Italy, on the impact of the diagnosis of hepatitis C infection on lifestyle habits such as smoking, drinking, sports activity and diet.
Between July 2001 and October 2002 we have consecu-tively offered a self-administered, anonymous questionnaire to out-patients with HCV infection attending three clinical centres in Italy (National Institute of Infectious Disease L. Spallanzani, Rome; Gastroenterology Unit, University of Palermo; Department of Infectious and Tropical Diseases, University of Brescia).
The questionnaire contained 67 items investigating the following areas: (1) Sociodemographic characteristics (gender; age; years of education; job status; marital status); (2) Health status and lifestyle (smoking and drinking habits; diet; sports activity; risk factors for HCV); (3) History of infection/disease (date of first HCV-Ab positive test; reason for HCV-Ab test; years of clinical follow-up; number of visits in the last year; healthcare provider; liver biopsy; treatment); (4) Information sources on hepatitis C; (5) Knowledge on hepatitis C virus infection (transmission; progression of disease and treatment); (6) Current at-risk behaviours (sexual behaviours; drug addiction). In the present study we analyzed only answers to the first 4 areas of the questionnaire.
Informed consent was obtained from participants and our ethics committee approved the study.
Chi-square test and Fisher's exact test were performed. Only questionnaires with a rate of missing answers less than 20% were considered valid for statistical analysis; this rate was calculated on 31 items to which all patients had to answer. Data were entered into an Access database, verified by double entry and analyzed using SPSS package (version 11.00 SPSS Inc., Chicago, Illinois). To verify the validity of the questionnaire as a good source of information, for 19 subjects we compared the information obtained for 2 items (liver biopsy; antiviral treatment) with pertinent data derived from their clinical records by using the kappa (κ) measure of agreement. Results of this comparison show a high degree of accordance: liver biopsy (κ = 1) and antiviral treatment (κ = 1).
Of the 303 enrolled patients, 275 returned a valid questionnaire (102 from Rome, 86 from Palermo and 87 from Brescia). Of the 275 respondents, 62.2% (171) were male. Mean age was 51 (range 20-80) years and median age was 53 + 13.7 years (SD). Regarding formal education, 53.3% had attended school for 8 years, 34.9% for 9-13 years and 11.3% for 14 years or more. Forty-eight percent of patients were employed and most (70.5%) were married and not living alone. Table 1 shows the distribution of characteristics regarding the history of infection. The most commonly reported potential risk factors for HCV acquisition were: surgical procedures (55.3%); transfusion before 1992 (15.3%); injection drug use (12.4%); tattoo/piercing (6.9%); sexual partner infected with HCV (6.9%); sexual intercourses with injection drug users (11.6%). Twenty-eight percent of patients reported more than one risk factor.
| Years since HCV (+) (median ± SD) | 5 + 4 |
| Age at diagnosis (median ± SD) | 46 + 14.1 |
| First visit n (%) | 23 (8.4) |
| Years of follow-up n (%) | |
| < 1 | 47 (17.1) |
| 1-2 | 47 (17.1) |
| 3-4 | 38 (13.8) |
| 5-6 | 34 (12.4) |
| > 7 | 67 (24.4) |
| not known | 19 (6.8) |
| Healthcare provider n (%) | |
| family physician | 11 (4) |
| hepatologist | 218 (79.3) |
| other | 10 (3.6) |
| not known | 13 (4.7) |
| Visits during the last year n (%) | |
| 0 | 10 (3.6) |
| 1 | 35 (12.7) |
| 2-4 | 84 (30.5) |
| >4 | 114 (41.5) |
| not known | 9 (3.3) |
| Liver biopsy n (%) | 213 (77.5) |
| Treatment n (%) | 186 (67.6) |
Information on hepatitis C was received by a healthcare provider (mostly a physician) in 270 cases (69% of answers). Additionally, more than 30% of patients retrieved information through the media (internet, TV, magazines) (86 cases; 21.9% of answers) and 13% through relatives or friends (35 cases, 8.9% of answers).
Fifty-six percent (55.6%) (153/275) of the respondents reported alcohol consumption. One hundred-sixteen subjects were former drinkers, in particular 89 stopped drinking after the diagnosis of hepatitis C. Thirty-seven subjects were current drinkers with a moderate alcohol consumption according to WHO limits (< 28 U/wk for men and < 14 U/wk for woman)[15]; 25 of these reduced their alcohol consumption after the diagnosis of hepatitis C. Overall, 74.5% (114/153) of these subjects had modified their drinking habits due to HCV infection.
Sixty-five percent (178/275) of the respondents reported tobacco consumption. Eighty-four subjects were former smokers, in particular 12 had given up after the diagnosis of hepatitis C, while 90 (32.7% of the respondents) were current smokers, 25 of whom reduced their tobacco consumption after the diagnosis of hepatitis C. Overall, 20.8% (37/178) of these subjects had modified their smoking habits due to HCV infection.
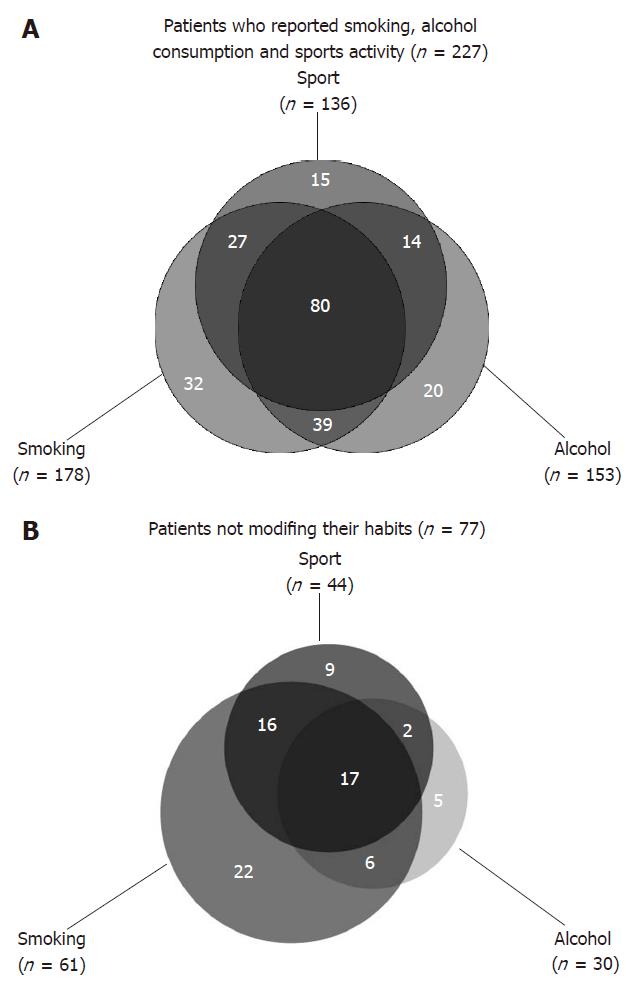
Approximately half of the respondents practiced sports, 32.3% (44/136) of whom had modified their habits after the diagnosis of hepatitis C. In particular, 15 stopped their practice, 16 reduced their frequency and 13 chose a less fatiguing sport. The percentage of HCV drinkers with other overlapping habits (sports activity, tobacco consumption) was 86.9% (133/153); the percentage of smokers with other overlapping habits was 82% (146/178) and that of patients practicing sports with other overlapping habits was 89% (121/136) (Figure 1A). Overall, 227 respondents reported smoking, alcohol, sports or a combination of these, and 150 (54.5%) modified at least one of these habits, while 77 did not (Figure 1B).
Sixty-four percent (176/275) of the respondents reported to have modified their diet after the diagnosis of hepatitis C, particularly reducing their fat intake (138 patients) and/or reducing consumption of some foods (88 patients) such as fried food, sausages, fat food and chocolate. Most of those who modified their diet because of hepatitis did so on medical advice, either from their specialist (47.7%; 84/176) or from their general practitioner (23.8%), while for 38 subjects (21.6%) it was a personal choice.
At univariate analysis, changes in smoking habit and sport practicing due to the diagnosis of hepatitis C were strongly related to a previous antiviral treatment (P = 0.056 and 0.014), while no correlation was found between other modifications of lifestyle habits and sociodemographic characteristics or variables on history of infection (Table 2).
| Patients modifying smoking habit after HCV infectionn (%) | Patients modifying sport activity after HCV infectionn (%) | |||||||
| Previous treatment | Yes | No | Total | P | Yes | No | Total | P |
| Yes | 28 (90.3) | 84 (73.7) | 112 (77.2) | 0.056 | 36 (87.8) | 47 (66.2) | 83 (74.1) | 0.014 |
| No | 3 (9.7) | 30 (26.3) | 33 (22.8) | 5 (12.2) | 24 (33.8) | 29 (25.9) | ||
| Total | 31 | 114 | 145 | 41 | 71 | 112 | ||
Results of this study show that more than half of the respondents have modified at least one of their lifestyle habits after the diagnosis of hepatitis C. Overall, 74.5% (114/153) of drinkers had modified their alcohol consumption (89 giving up and 25 reducing), 20.8% (37/178) of smokers had modified their habits (12 giving up and 25 reducing) and 32.3% (44/136) of subjects who reported sports activity had either stopped or reduced frequency of activity or chose a less fatiguing sport after the diagnosis of hepatitis C. These changes seem to be rather long-lasting, since the median time interval between the diagnosis of HCV infection and the survey was 5 years.
It is well established that alcohol consumption is associated with an increased rate of fibrosis progression in established chronic HCV infection[16]. Even with moderate alcohol consumption, there is a linear correlation between both histological activity and fibrosis and amount of alcohol ingested, as suggested by Hezode et al[17]. All international guidelines recommend that patients with hepatitis C virus infection or other chronic liver disease consume no alcohol[3-8]. Our data, in line with pervious studies, indicate that most patients with chronic HCV infection do modify their alcohol intake following diagnosis[12-14].
Possible hepatotoxicity of tobacco has been suggested only recently. Tobacco consumption has been associated in chronic hepatitis C (CHC) patients with increased fibrosis and histological activity[11,18], with an increased risk of hepatocellular carcinoma[19-21] and with poorer response to interferon therapy[10]. A synergism between alcohol drinking and cigarette smoking has been suggested[22].
In our study only 20.8% (37/178) of smokers had modified their habits after the diagnosis of hepatitis C, whereas 40.4% (72/178) had given up independently. Moreover a proportion of current smokers (32.7%) in our study was slightly higher than that reported for the adult Italian population (26.6% in 2002)[23]. These findings underline the necessity to inform HCV-positive patients that tobacco smoking could influence liver disease. In addition, considering the general health benefits of smoking cessation and that our patients were frequently under medical care, our results may indicate a missed opportunity for promoting healthy behaviour.
Currently, there is no evidence resulting from controlled clinical trials in favour or against physical activity in patients with chronic liver disease[24]. Groups of patients affected by liver cirrhosis studied so far seem to tolerate physical activity like vigorous walking, swimming and ergometer bicycle training without deterioration of liver function[24]. Some studies conducted in the 80s seemed to demonstrate the innocuous effect of physical exercise on chronic hepatitis[25,26] while when daily physical labour is strenuous (over 2 h), it seems to be related to elevated ALT levels[9].
It is surprising that one third of subjects who reported sports activity had modified their habits after the diagnosis of hepatitis C. However, changes in sports practicing after the diagnosis of hepatitis C were strongly related to previous antiviral treatment and we cannot exclude that some patients modified their habits particularly as a consequence of adverse effects such as asthenia or nausea. On the other hand, our results may suggest the existence of a misconception regarding the need for people affected by liver disease to refrain from significant physical exertion, possibly as a result of the tradition to prescribe a strict bed-rest during acute hepatitis, in spite of the availability of evidence against this[24].
Although no specific dietary recommendations can be made for most persons with HCV infection excluding patients with cirrhosis, steatosis, obesity and other metabolic disease[27-29], sixty-four percent (176/275) of our patients modified their dietary habits after the diagnosis of hepatitis C. The most frequent modification was the reduction of dietary fat intake (40.8% of the answers). A single epidemiologic investigation suggested an association between higher lipid intake and increased risk for cirrhosis in persons with HCV infection[30]; however there is no evidence of the need to routinely limit the dietary fat content[27]. Most patients declared to have modified their diet on physician's advice and we do not know how many patients were affected by liver cirrhosis or co-morbidities (such as steatosis, obesity or diabetes) needing particular nutritional intervention. On the other hand it can be speculated that these changes may reflect at least in part a misconception regarding the negative effect of some foods such as fried for people affected by liver diseases.
In this study we have chosen a completely anonymous and self-administered questionnaire in order to assure confidentiality and increased reliability of the answers. However this study design makes it impossible to correlate the observed changes with the clinical data of the patients enrolled. Another limitation is that our study sample consists of out-patients with HCV infection attending three specialized clinical centres, consequently it is not necessarily representative of the overall population of HCV-infected patients, for example patients with normal ALT or not eligible for treatment may be under-represented.
In conclusion, our investigation shows that some healthy modifications like those regarding alcohol consumption are largely adopted by chronic hepatitis C patients, whereas this diagnosis has less impact on smoking habits. On the other hand, our results suggest the likelihood of some misconceptions regarding diet and physical activity leading to possible unnecessary restrictions. In our study population the principal source of information on hepatitis C was the physician. This underlies the central role of physicians involved in the management of chronic hepatitis C and the need to counsel patients on measures that may maximize quality of life and prevent further disease progression.
In order to counsel patients with chronic hepatitis C, a general consent is necessary on recommendations about lifestyle habits, such as smoking, physical activity and nutrition.
The authors thank Tim Sladden for allowing them to view his questionnaire which has been useful during the design of our study, and Gabriella De Carli for reviewing the manuscript.
S- Editor Zhu LH L- Editor Alpini GD E- Editor Chen GJ
| 1. | Alberti A, Chemello L, Benvegnù L. Natural history of hepatitis C. J Hepatol. 1999;31 Suppl 1:17-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 240] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 2. | Spiegel BM, Younossi ZM, Hays RD, Revicki D, Robbins S, Kanwal F. Impact of hepatitis C on health related quality of life: a systematic review and quantitative assessment. Hepatology. 2005;41:790-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 273] [Cited by in RCA: 273] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 3. | National Institutes of Health Consensus Development Conference Statement. 2002--June 10-12, 2002. Hepatology. 2002;36:S3-S20. [PubMed] [DOI] [Full Text] |
| 4. | National Institute for Clinical Excellence (2000), Guidance on the use of ribavirin and interferon alpha for hepatitis C, NICE Technology Appraisal No. 14. London: National Institute for Clinical Excellence. Available from: http//www.nice.org.uk; www.nice.org.uk/TA075guidance. |
| 5. | British Columbia Medical Association; Ministry of Health Services; Ministry of Health Planning, Guidelines and Protocols Advisory Committee British Columbia Centre for Disease Control. Clinical Management of Chronic Hepatitis C. Available from: http//www.bccdc.org/hepatitis/research. |
| 6. | Canadian association for study of the liver. The management of viral hepatitis, Consensus Conference Montreal, Quebec March 1999. Available from: http//www.lhsc.on.ca/casl/cont.htm. |
| 7. | Booth JC, O'Grady J, Neuberger J. Clinical guidelines on the management of hepatitis C. Gut. 2001;49 Suppl 1:I1-I21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 96] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 8. | Agence Nationale d’Accréditation et d’Évaluation en Santé, Consensus Conference. Treatment of hepatitis C. Paris, France, 27-28 February 2002. Available from: http//www.anaes.fr. |
| 9. | Kubo N, Furusyo N, Nakashima H, Kashiwagi K, Hayashi J. Strenuous physical labor is important as a cause of elevated alanine aminotransferase levels in Japanese patients with chronic hepatitis C viremia. Eur J Epidemiol. 2005;20:251-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | El-Zayadi A, Selim O, Hamdy H, El-Tawil A, Badran HM, Attia M, Saeed A. Impact of cigarette smoking on response to interferon therapy in chronic hepatitis C Egyptian patients. World J Gastroenterol. 2004;10:2963-2966. [PubMed] |
| 11. | Pessione F, Ramond MJ, Njapoum C, Duchatelle V, Degott C, Erlinger S, Rueff B, Valla DC, Degos F. Cigarette smoking and hepatic lesions in patients with chronic hepatitis C. Hepatology. 2001;34:121-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 133] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 12. | Sladden TJ, Hickey AR, Dunn TM, Beard JR. Hepatitis C virus infection: impacts on behaviour and lifestyle. Aust N Z J Public Health. 1998;22:509-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Castera L, Constant A, Bernard PH, de Ledinghen V, Couzigou P. Lifestyle changes and beliefs regarding disease severity in patients with chronic hepatitis C. J Viral Hepat. 2006;13:482-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Fabris P, Tositti G, Giordani MT, Baldo V, Grasso A, Pignattari E, Canton S, Rossato S, Floreani A. Assessing patients' understanding of hepatitis C virus infection and its impact on their lifestyle. Aliment Pharmacol Ther. 2006;23:1161-1170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Jessor R. Prevention of alcohol problems. Technical Report Series No. 650. Geneva: World Health Organization 1980; 28-44. |
| 16. | Poynard T, Bedossa P, Opolon P. Natural history of liver fibrosis progression in patients with chronic hepatitis C. The OBSVIRC, METAVIR, CLINIVIR, and DOSVIRC groups. Lancet. 1997;349:825-832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2199] [Cited by in RCA: 2160] [Article Influence: 77.1] [Reference Citation Analysis (0)] |
| 17. | Hézode C, Lonjon I, Roudot-Thoraval F, Pawlotsky JM, Zafrani ES, Dhumeaux D. Impact of moderate alcohol consumption on histological activity and fibrosis in patients with chronic hepatitis C, and specific influence of steatosis: a prospective study. Aliment Pharmacol Ther. 2003;17:1031-1037. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 82] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 18. | Pessione F, Degos F, Marcellin P, Duchatelle V, Njapoum C, Martinot-Peignoux M, Degott C, Valla D, Erlinger S, Rueff B. Effect of alcohol consumption on serum hepatitis C virus RNA and histological lesions in chronic hepatitis C. Hepatology. 1998;27:1717-1722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 240] [Cited by in RCA: 231] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 19. | Mori M, Hara M, Wada I, Hara T, Yamamoto K, Honda M, Naramoto J. Prospective study of hepatitis B and C viral infections, cigarette smoking, alcohol consumption, and other factors associated with hepatocellular carcinoma risk in Japan. Am J Epidemiol. 2000;151:131-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 87] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 20. | Mukaiya M, Nishi M, Miyake H, Hirata K. Chronic liver diseases for the risk of hepatocellular carcinoma: a case-control study in Japan. Etiologic association of alcohol consumption, cigarette smoking and the development of chronic liver diseases. Hepatogastroenterology. 1998;45:2328-2332. [PubMed] |
| 21. | Yu MW, Chiu YH, Yang SY, Santella RM, Chern HD, Liaw YF, Chen CJ. Cytochrome P450 1A1 genetic polymorphisms and risk of hepatocellular carcinoma among chronic hepatitis B carriers. Br J Cancer. 1999;80:598-603. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 54] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 22. | Wang CS, Wang ST, Chang TT, Yao WJ, Chou P. Smoking and alanine aminotransferase levels in hepatitis C virus infection: implications for prevention of hepatitis C virus progression. Arch Intern Med. 2002;162:811-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 44] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 23. | Gallus S, Pacifici R, Colombo P, La Vecchia C, Garattini S, Apolone G, Zuccaro P. Tobacco dependence in the general population in Italy. Ann Oncol. 2005;16:703-706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Harrington DW. Viral hepatitis and exercise. Med Sci Sports Exerc. 2000;32:S422-S430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Ritland S, Foss NE, Gjone E. Physical activity in liver disease and liver function in sportsmen. Scand J Soc Med Suppl. 1982;29:221-226. [PubMed] |
| 26. | Ritland S, Foss NE, Skrede S. The effect of a standardized work load on 'liver tests' in patients with chronic active hepatitis. Scand J Gastroenterol. 1982;17:1013-1016. [PubMed] |
| 27. | Herrine SK. Approach to the patient with chronic hepatitis C virus infection. Ann Intern Med. 2002;136:747-757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 28. | Hickman IJ, Jonsson JR, Prins JB, Ash S, Purdie DM, Clouston AD, Powell EE. Modest weight loss and physical activity in overweight patients with chronic liver disease results in sustained improvements in alanine aminotransferase, fasting insulin, and quality of life. Gut. 2004;53:413-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 302] [Cited by in RCA: 288] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 29. | Wendland BE. Nutritional guidelines for persons infected with the hepatitis C virus: a review of the literature. Can J Diet Pract Res. 2001;62:7-15. [PubMed] |
| 30. | Corrao G, Ferrari PA, Galatola G. Exploring the role of diet in modifying the effect of known disease determinants: application to risk factors of liver cirrhosis. Am J Epidemiol. 1995;142:1136-1146. [PubMed] |